Clin Orthop Surg.
2019 Mar;11(1):131-136. 10.4055/cios.2019.11.1.131.
Preganglionic Epidural Steroid Injection through Translateral Recess Approach
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul Red Cross Hospital, Seoul, Korea. orthopedicspinae@gmail.com
- 2Department of Orthopedic Surgery, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- KMID: 2438344
- DOI: http://doi.org/10.4055/cios.2019.11.1.131
Abstract
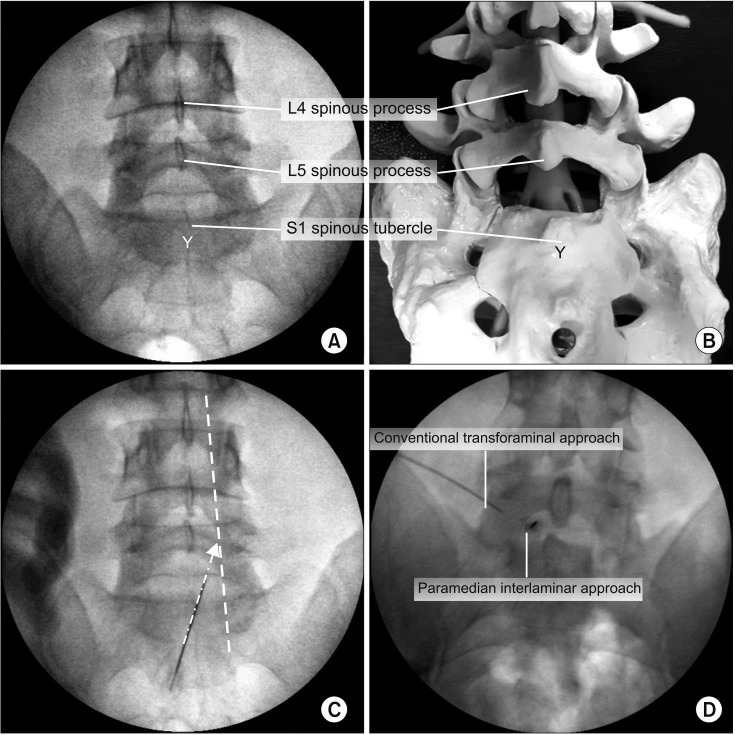
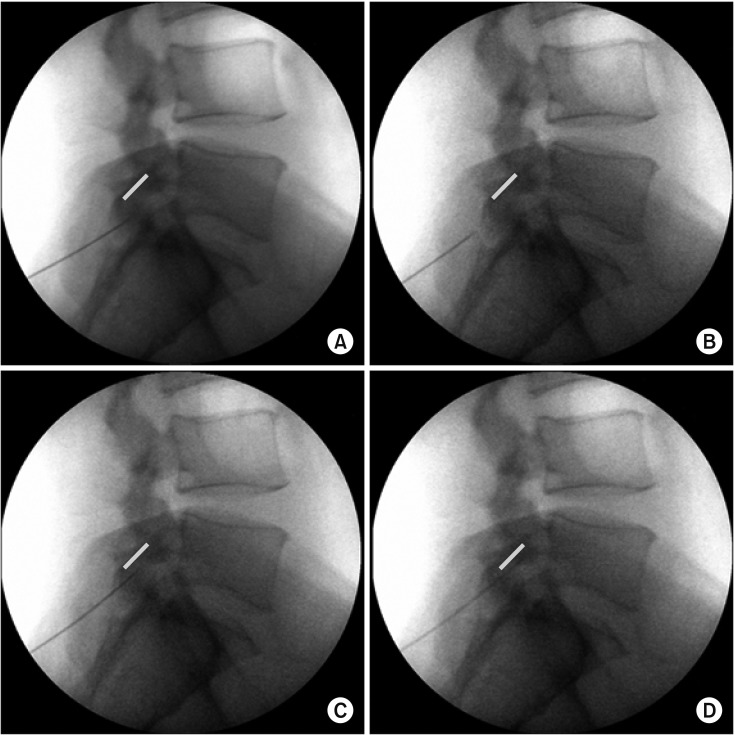
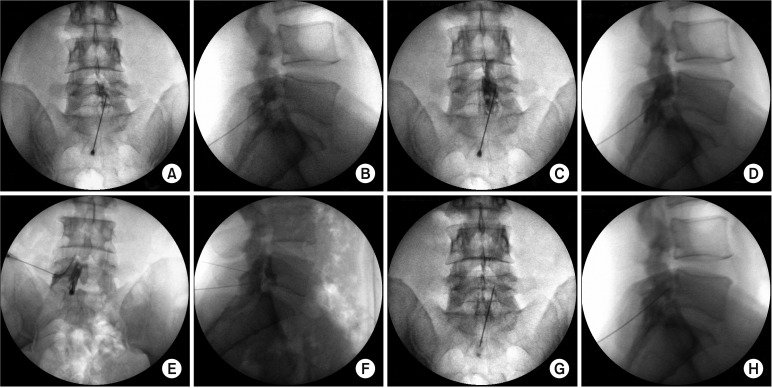
- The approach we suggest was developed for cases in which the fourth and fifth lumbar and first sacral spinal nerves were affected in lumbar degenerative disc disease. Retrodiscal transforaminal epidural injection is known to be very effective for lumbar radiculopathy because of excellent access to primary pathology; however, access below L5 is often restricted by the anatomic characteristics of the L5-S1. In the translateral recess approach (TLR), proper final needle placement (i.e., in the axillary portion between the exiting and traversing nerve roots) can be achieved by setting the direction of the needle laterally and superiorly from the distal tip of the infra-adjacent spinous process toward the medial wall of the pedicle and neural foramen of the given level without neural injury. This approach is possible because of the wide interlaminar space in the L5-S1. Preganglionic epidural injection through TLR is an effective and safe spinal intervention for lumbosacral radiculopathy.
Figure
Reference
-
1. Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013; 38(2):157–168. PMID: 22781007.2. Bicket MC, Horowitz JM, Benzon HT, Cohen SP. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. Spine J. 2015; 15(2):348–362. PMID: 25463400.
Article3. Kabatas S, Cansever T, Yilmaz C, et al. Transforaminal epidural steroid injection via a preganglionic approach for lumbar spinal stenosis and lumbar discogenic pain with radiculopathy. Neurol India. 2010; 58(2):248–252. PMID: 20508344.
Article4. Kortelainen P, Puranen J, Koivisto E, Lahde S. Symptoms and signs of sciatica and their relation to the localization of the lumbar disc herniation. Spine (Phila Pa 1976). 1985; 10(1):88–92. PMID: 3983706.
Article5. Ebraheim NA, Miller RM, Xu R, Yeasting RA. The location of the intervertebral lumbar disc on the posterior aspect of the spine. Surg Neurol. 1997; 48(3):232–236. PMID: 9290709.
Article6. Shim DM, Choi YH, Yang JH, Oh SK, Kim CG, Park JH. Analysis and measurement of the lumbar spinal canal dimension using magnetic resonance imaging. J Korean Orthop Assoc. 2008; 43(5):588–594.
Article7. Xu R, Burgar A, Ebraheim NA, Yeasting RA. The quantitative anatomy of the laminas of the spine. Spine (Phila Pa 1976). 1999; 24(2):107–113. PMID: 9926378.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Persistent Hiccup after Epidural Steroid Injection: Case reports
- Epidural Steroid Injection
- Pneumocephalus after Epidural Steroid Injection: A case report
- Selective Epidural Steroid Injection in a Patient with Refractory Radicular Leg Pain: A case report
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy