Clin Orthop Surg.
2019 Mar;11(1):36-42. 10.4055/cios.2019.11.1.36.
The Effect of Valgus Reduction on the Position of the Blade of the Proximal Femoral Nail Antirotation in Intertrochanteric Hip Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, Samsung Medical Center, Seoul, Korea.
- 2Department of Orthopedic Surgery, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. ybs58@paik.ac.kr
- 3Department of Orthopedic Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2438332
- DOI: http://doi.org/10.4055/cios.2019.11.1.36
Abstract
- BACKGROUND
The purpose of this study was to evaluate the quantitative association between the degree of reduction and the position of the blade of the proximal femoral nail antirotation (PFNA) in intertrochanteric hip fractures.
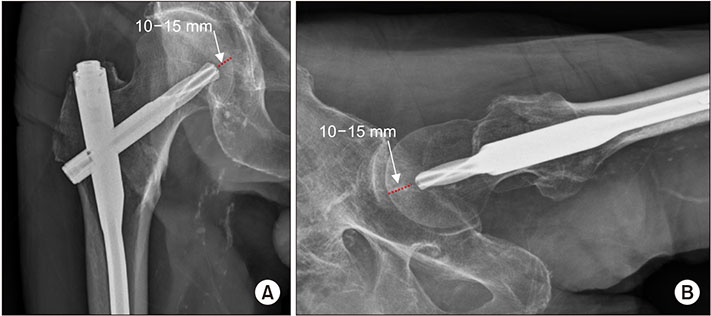
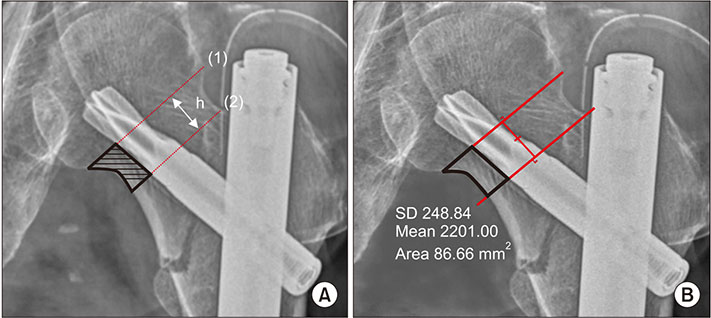
METHODS
From March 2009 to April 2015, 530 patients treated with PFNA for intertrochanteric hip fractures were retrospectively reviewed. Patients were divided into a valgus reduced group (group 1) and a non-valgus reduced group (group 2), and the "valgus reduced" was defined as valgus reduction over 5°. We compared the calcar referenced tip-apex distance (calTAD) and the area between the blade of PFNA and the medial cortex of the femoral neck between the two groups.
RESULTS
The calTAD was measured as 22.5 ± 4.1 mm in group 1 and 24.8 ± 3.8 mm in group 2 (p < 0.05). The area between the blade and the medial femoral neck was measured as 135.5 ± 49.8 mm2 in group 1 and 145.1 ± 54.8 mm2 in group 2 (p = 0.074). The area corrected for the length difference in the femoral neck was 0.55 ± 0.16 in group 1 and 0.79 ± 0.19 in group 2 (p < 0.05).
CONCLUSIONS
Valgus reduction resulted in less calTAD and inferior position of the blade at the femoral neck in the treatment of intertrochanteric hip fractures with PFNA.
MeSH Terms
Figure
Cited by 1 articles
-
Risk Factors Associated with Failure of Cephalomedullary Nail Fixation in the Treatment of Trochanteric Hip Fractures
Jehyun Yoo, Jundong Chang, Changwon Park, Jihyo Hwang
Clin Orthop Surg. 2020;12(1):29-36. doi: 10.4055/cios.2020.12.1.29.
Reference
-
1. Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003; 17(1):53–56.
Article2. Zhang K, Zhang S, Yang J, et al. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: a meta-analysis. Med Sci Monit. 2014; 20:1628–1633.
Article3. Kaufer H, Matthews LS, Sonstegard D. Stable fixation of intertrochanteric fractures. J Bone Joint Surg Am. 1974; 56(5):899–907.
Article4. Ma KL, Wang X, Luan FJ, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res. 2014; 100(8):859–866.
Article5. Chang SM, Zhang YQ, Du SC, et al. Anteromedial cortical support reduction in unstable pertrochanteric fractures: a comparison of intra-operative fluoroscopy and post-operative three dimensional computerised tomography reconstruction. Int Orthop. 2018; 42(1):183–189.
Article6. Choi NY, Nah KH, Song HS, Seo SI, Choi JK, Han SK. Treatment of the intertrochanteric fractures of the femur in elderly patients: comparision of Wayne-County reduction and anatomical reduction. J Korean Fract Soc. 2004; 17(4):301–307.
Article7. Park JK, Shon HC, Kim YM, et al. Effectiveness of the valgus reduction technique in treatment of intertrochanteric fractures using proximal femoral nail antirotation. J Korean Orthop Assoc. 2013; 48(6):441–448.
Article8. Lee DY, Hwang SC, Jeong ST, Oh JY, Kim DH. Risk factors of cut-out in treatment of femoral intertrochanteric fractures by proximal femur nail. J Korean Orthop Assoc. 2017; 52(4):319–326.
Article9. Stiehl JB, Jacobson D, Carrera G. Morphological analysis of the proximal femur using quantitative computed tomography. Int Orthop. 2007; 31(3):287–292.
Article10. Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir O, Kuzyk PR. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J. 2014; 96(8):1029–1034.
Article11. Paul O, Barker JU, Lane JM, Helfet DL, Lorich DG. Functional and radiographic outcomes of intertrochanteric hip fractures treated with calcar reduction, compression, and trochanteric entry nailing. J Orthop Trauma. 2012; 26(3):148–154.
Article12. Puthezhath K, Jayaprakash C. Is calcar referenced tip-apex distance a better predicting factor for cutting out in biaxial cephalomedullary nails than tip-apex distance? J Orthop Surg (Hong Kong). 2017; 25(3):2309499017727920.
Article13. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma. 2007; 21(7):485–489.
Article14. Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009; 91(3):712–719.15. Caruso G, Bonomo M, Valpiani G, et al. A six-year retrospective analysis of cut-out risk predictors in cephalomedullary nailing for pertrochanteric fractures: can the tip-apex distance (TAD) still be considered the best parameter? Bone Joint Res. 2017; 6(8):481–488.
Article16. Laskin RS, Gruber MA, Zimmerman AJ. Intertrochanteric fractures of the hip in the elderly: a retrospective analysis of 236 cases. Clin Orthop Relat Res. 1979; (141):188–195.17. Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015; 135(6):811–818.
Article18. Jiamton C, Boernert K, Babst R, Beeres FJ, Link BC. The nail-shaft-axis of the of proximal femoral nail antirotation (PFNA) is an important prognostic factor in the operative treatment of intertrochanteric fractures. Arch Orthop Trauma Surg. 2018; 138(3):339–349.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fixation Failure of Proximal Femoral Nail Anti-rotation in Femoral Intertrochanteric Fracture
- Factors Associated with Mechanical Complications in Intertrochanteric Fracture Treated with Proximal Femoral Nail Antirotation
- Factors Affecting Telescoping of Spiral Blade after Operation for Intertrochanteric Fracture with Proximal Femoral Nail Antirotation II
- Results of the Proximal Femoral Nail-Antirotation (PFNA) in Patients with an Unstable Pertrochanteric Fracture
- Mid-term Results of Patients with Femoral Intertrochanteric Fractures Treated with Proximal Femoral Nail Antirotation