Clin Orthop Surg.
2019 Mar;11(1):21-27. 10.4055/cios.2019.11.1.21.
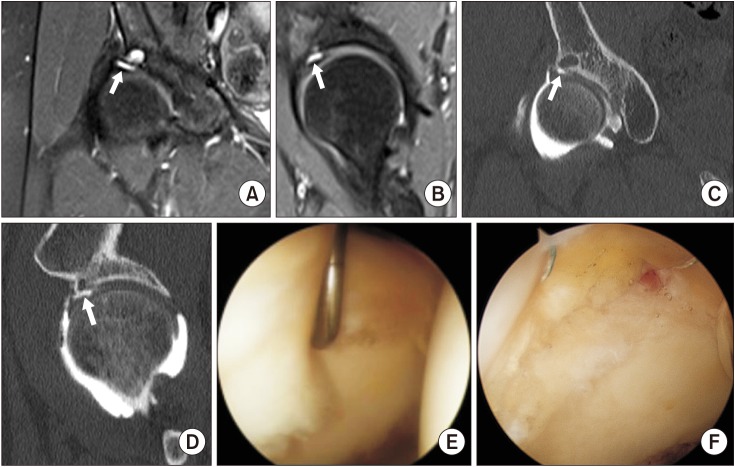
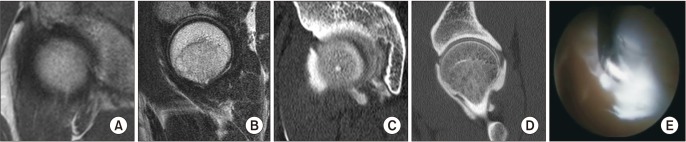
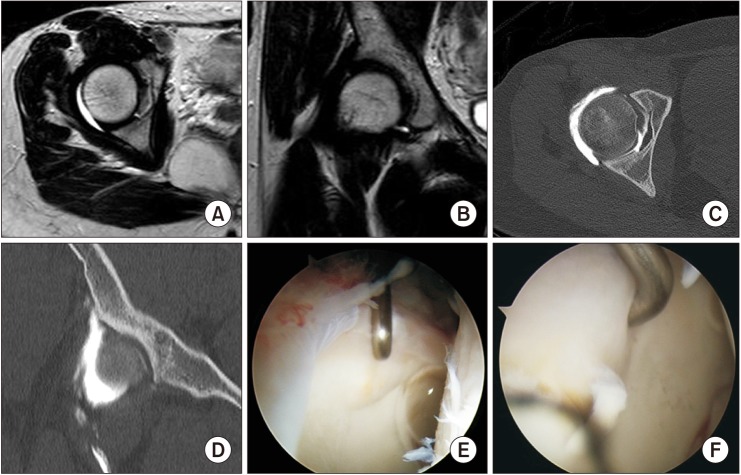
Accuracy of Magnetic Resonance Imaging and Computed Tomography Arthrography in Diagnosing Acetabular Labral Tears and Chondral Lesions
- Affiliations
-
- 1Department of Radiology, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Department of Orthopaedic Surgery, Chung-Ang University College of Medicine, Seoul, Korea. hayongch@naver.com
- KMID: 2438330
- DOI: http://doi.org/10.4055/cios.2019.11.1.21
Abstract
- BACKGROUND
We investigated sensitivity, specificity, and accuracy of magnetic resonance imaging (MRI) and computed tomography arthrography (CTA), on the basis of arthroscopic findings, to diagnose acetabular labral tears and chondral lesions.
METHODS
We retrospectively reviewed the results of MRI and subsequent CTA in 36 hips that underwent arthroscopic surgery (33 patients; 17 males [17 hips] and 16 females [19 hips]; average age, 35 years). All patients had positive impingement test results and groin pain. We analyzed sensitivity, specificity, and accuracy of MRI and CTA by comparing with the arthroscopic findings. Interobserver agreement and intraobserver reproducibility of the presence of tears and cartilage lesions on MRI and CTA were calculated using Kappa coefficients.
RESULTS
The sensitivity, specificity, and accuracy of MRI for detection of acetabular labral tears by two observers were 60%, 80%, and 64%, respectively, and 65%, 70%, and 69%, respectively. The sensitivity, specificity, and accuracy of CTA for detection of labral tears by both observers were 85%, 90%, and 86%, respectively, and 92%, 80%, and 89%, respectively. However, the sensitivity and specificity of MRI for detection of acetabular chondral lesions by both observers were 36% and 84%, respectively, and 46% and 88%, respectively. The sensitivity and specificity of CTA for detecting acetabular cartilage lesions by both observers were 46% and 72%, respectively, and 64% and 72%, respectively. Intraobserver reproducibility for detection of labral tears and chondral lesions by using MRI was substantial (κ = 0.756 and κ = 0.693, respectively). Interobserver reliability for detection of labral tears and chondral lesions by using MRI was substantial (κ = 0.700 and κ = 0.875, respectively). Intraobserver reproducibility for detection of labral tears and chondral lesions by using CTA was substantial (κ = 0.832 and κ = 0.774, respectively). Interobserver reliability for detection of labral tears and chondral lesions by using CTA was high (κ = 0.886 and κ = 0.596, respectively).
CONCLUSIONS
This study demonstrated that the accuracy of MRI to detect an acetabular labral tear and a chondral lesion of the hip joint was not sufficient. CTA was reliable in the diagnosis of acetabular labral tears. However, both CTA and MRI were also of limited value to detect chondral lesions.
Keyword
MeSH Terms
Figure
Reference
-
1. Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986; (213):20–33.2. Jung JY, Kim GU, Lee HJ, Jang EC, Song IS, Ha YC. Diagnostic value of ultrasound and computed tomographic arthrography in diagnosing anterosuperior acetabular labral tears. Arthroscopy. 2013; 29(11):1769–1776. PMID: 24071389.3. Ha YC, Choi JA, Lee YK, et al. The diagnostic value of direct CT arthrography using MDCT in the evaluation of acetabular labral tear: with arthroscopic correlation. Skeletal Radiol. 2013; 42(5):681–688. PMID: 23073899.
Article4. Nishii T, Tanaka H, Nakanishi K, Sugano N, Miki H, Yoshikawa H. Fat-suppressed 3D spoiled gradient-echo MRI and MDCT arthrography of articular cartilage in patients with hip dysplasia. AJR Am J Roentgenol. 2005; 185(2):379–385. PMID: 16037508.
Article5. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004; 32(7):1668–1674. PMID: 15494331.
Article6. Czerny C, Hofmann S, Neuhold A, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology. 1996; 200(1):225–230. PMID: 8657916.
Article7. Sundberg TP, Toomayan GA, Major NM. Evaluation of the acetabular labrum at 3.0-T MR imaging compared with 1.5-T MR arthrography: preliminary experience. Radiology. 2006; 238(2):706–711. PMID: 16436825.
Article8. Lage LA, Patel JV, Villar RN. The acetabular labral tear: an arthroscopic classification. Arthroscopy. 1996; 12(3):269–272. PMID: 8783819.
Article9. Blankenbaker DG, De Smet AA, Keene JS, Fine JP. Classification and localization of acetabular labral tears. Skeletal Radiol. 2007; 36(5):391–397. PMID: 17226059.
Article10. Jin W, Kim KI, Rhyu KH, et al. Sonographic evaluation of anterosuperior hip labral tears with magnetic resonance arthrographic and surgical correlation. J Ultrasound Med. 2012; 31(3):439–447. PMID: 22368134.
Article11. Perdikakis E, Karachalios T, Katonis P, Karantanas A. Comparison of MR-arthrography and MDCT-arthrography for detection of labral and articular cartilage hip pathology. Skeletal Radiol. 2011; 40(11):1441–1447. PMID: 21298428.
Article12. Vande Berg BC, Lecouvet FE, Poilvache P, Maldague B, Malghem J. Spiral CT arthrography of the knee: technique and value in the assessment of internal derangement of the knee. Eur Radiol. 2002; 12(7):1800–1810. PMID: 12111072.
Article13. Byrd JW. Avoiding the labrum in hip arthroscopy. Arthroscopy. 2000; 16(7):770–773. PMID: 11027766.
Article14. Byrd JW. Hip arthroscopy: the supine position. Clin Sports Med. 2001; 20(4):703–731. PMID: 11675882.15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33(1):159–174. PMID: 843571.
Article16. Petersilge CA, Haque MA, Petersilge WJ, Lewin JS, Lieberman JM, Buly R. Acetabular labral tears: evaluation with MR arthrography. Radiology. 1996; 200(1):231–235. PMID: 8657917.
Article17. Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006; 186(2):449–453. PMID: 16423951.
Article18. Cohen SB, Huang R, Ciccotti MG, Dodson CC, Parvizi J. Treatment of femoroacetabular impingement in athletes using a mini-direct anterior approach. Am J Sports Med. 2012; 40(7):1620–1627. PMID: 22562788.
Article19. Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009; 467(3):747–752. PMID: 19089524.
Article20. Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004; (429):178–181.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Diagnostic Accuracy of 3.0-T MR Arthrography and CT Arthrography in Intraarticular Hip Pathology
- Comparison of MDCTA (16-Slice Multi-Detector Row Computed Tomography Arthrography) and MRA (Magnetic Resonance Arthrography) for Detecting Labral Lesions of the Shoulder
- Diagnostic Accuracy and Inter-Observer Agreement of Shoulder Magnetic Resonance Arthrography in the Detection of Labral Lesion and Assessment of Lesion Location
- Anterior Labral Tear: Diagnostic Value of MR Arthrography of the Shoulder
- 16-Slice MDCT Arthrography of the Shoulder: Accuracy for Detection of Glenoid Labral and Rotator Cuff Tears