J Pathol Transl Med.
2019 Jan;53(1):66-69. 10.4132/jptm.2017.12.13.
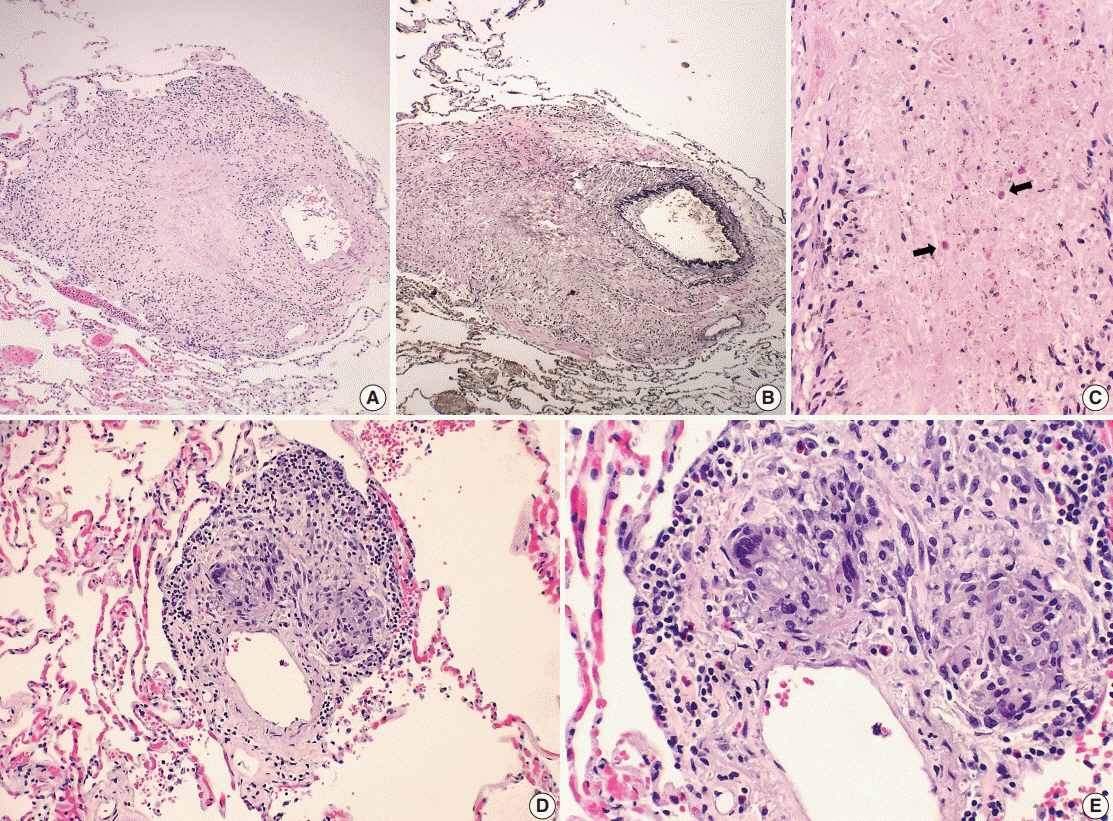
Rare Manifestations of Churg-Strauss Syndrome with Mediastinal and Hilar Lymphadenopathies: Report of an Autopsy Case
- Affiliations
-
- 1Department of Pathology and Laboratory Medicine, Hartford Hospital, Hartford, CT, USA. woocheal.cho@hhchealth.org
- KMID: 2437581
- DOI: http://doi.org/10.4132/jptm.2017.12.13
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Casey M, Radel E, Ratech H. Lymph node manifestations of limited Churg-Strauss syndrome. J Pediatr Hematol Oncol. 2000; 22:468–71.
Article2. Choi JY, Kim JE, Choi IY, et al. Churg-Strauss syndrome that presented with mediastinal lymphadenopathy and calculous cholecystitis. Korean J Intern Med. 2016; 31:179–83.
Article3. Choi YH, Im JG, Han BK, Kim JH, Lee KY, Myoung NH. Thoracic manifestation of Churg-Strauss syndrome: radiologic and clinical findings. Chest. 2000; 117:117–24.4. Churg A, Brallas M, Cronin SR, Churg J. Formes frustes of Churg-Strauss syndrome. Chest. 1995; 108:320–3.
Article5. Cualing H, Schroder L, Perme C. Allergic granulomatosis secondary to a limited form of Churg-Strauss syndrome. Arch Pathol Lab Med. 2001; 125:954–7.
Article6. Lesens O, Hansmann Y, Nerson J, et al. Severe Churg-Strauss syndrome with mediastinal lymphadenopathy treated with interferon therapy. Eur J Intern Med. 2002; 13:458.
Article7. Churg A. Recent advances in the diagnosis of Churg-Strauss syndrome. Mod Pathol. 2001; 14:1284–93.
Article8. Watts RA, Carruthers DM, Scott DG. Epidemiology of systemic vasculitis: changing incidence or definition? Semin Arthritis Rheum. 1995; 25:28–34.
Article9. Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol. 1951; 27:277–301.10. Masi AT, Hunder GG, Lie JT, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990; 33:1094–100.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Churg-Strauss Syndrome Presenting Umbilicated Ulcerative Papules
- A case of Churg-Strauss syndrome that underwent endoscopic sinus surgery under total intravenous anesthesia: A case report
- An atypical case of Churg-Strauss syndrome without asthma
- A Case of Chrug-Strauss Syndrome Complicated with Intestinal Perforation
- A Case of Churg-Strauss Syndrome with Endomyocardial Fibrosis