J Korean Orthop Assoc.
2018 Dec;53(6):466-477. 10.4055/jkoa.2018.53.6.466.
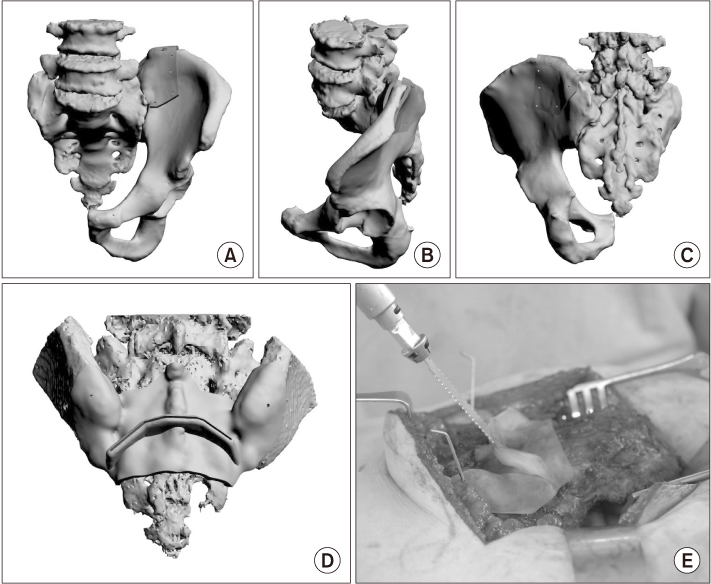
Three Dimensional Printing Technique and Its Application to Bone Tumor Surgery
- Affiliations
-
- 1Orthpaedic Oncology Clinic, National Cancer Center, Goyang, Korea. ostumor@ncc.re.kr
- 2Innovative Medical Engineering and Technology, National Cancer Center, Goyang, Korea.
- KMID: 2430053
- DOI: http://doi.org/10.4055/jkoa.2018.53.6.466
Abstract
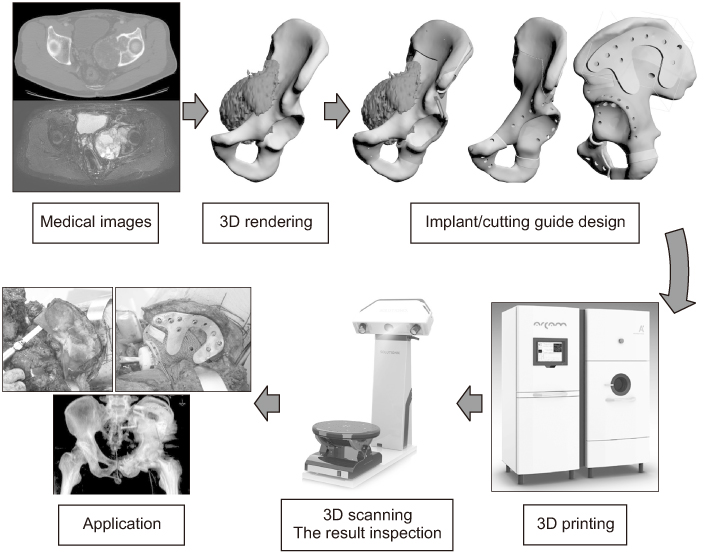
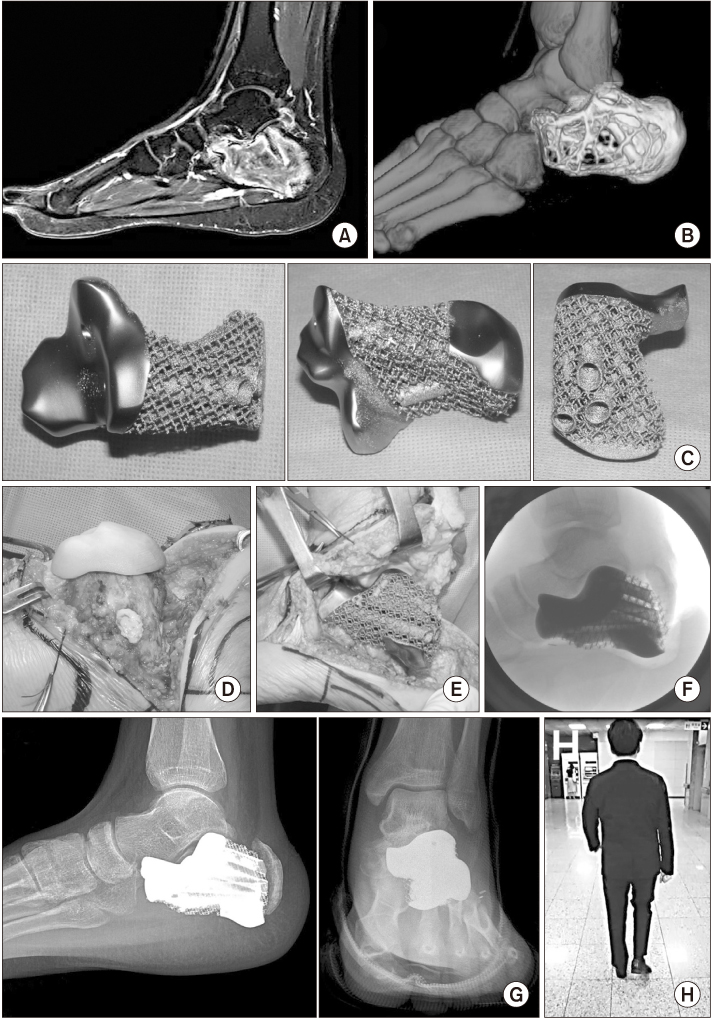
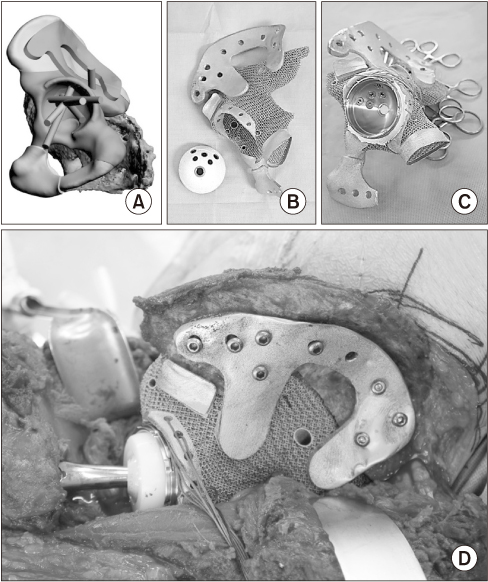
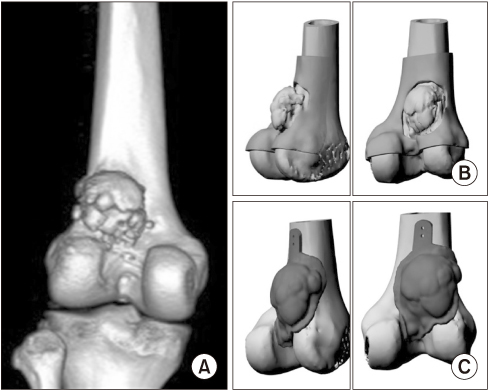
- Orthopaedics is an area where 3-dimensional (3D) printing technology is most likely to be utilized because it has been used to treat a range of diseases of the whole body. For arthritis, spinal diseases, trauma, deformities, and tumors, 3D printing can be used in the form of anatomical models, surgical guides, metal implants, bio-ceramic body reconstruction, and orthosis. In particular, in orthopaedic oncology, patients have a wide variety of tumor locations, but limited options for the limb salvage surgery have resulted in many complications. Currently, 3D printing personalized implants can be fabricated easily in a short time, and it is anticipated that all bone tumors in various surgical sites will be reconstructed properly. An improvement of 3D printing technology in the healthcare field requires close cooperation with many professionals in the design, printing, and validation processes. The government, which has determined that it can promote the development of 3D printing-related industries in other fields by leading the use of 3D printing in the medical field, is also actively supporting with an emphasis on promotion rather than regulation. In this review, the experience of using 3D printing technology for bone tumor surgery was shared, expecting orthopaedic surgeons to lead 3D printing in the medical field.
Keyword
MeSH Terms
Figure
Reference
-
1. Hoang D, Perrault D, Stevanovic M, Ghiassi A. Surgical applications of three-dimensional printing: a review of the current literature & how to get started. Ann Transl Med. 2016; 4:456.2. Petzold R, Zeilhofer HF, Kalender WA. Rapid protyping technology in medicine--basics and applications. Comput Med Imaging Graph. 1999; 23:277–284.3. Kim GB, Lee S, Kim H, et al. Three-dimensional printing: basic principles and applications in medicine and radiology. Korean J Radiol. 2016; 17:182–197.
Article4. Lee S. Prospect for 3D printing technology in medical, dental, and pediatric dental field. J Korean Acad Pediatr Dent. 2016; 43:93–108.
Article5. Byrne N, Velasco Forte M, Tandon A, Valverde I, Hussain T. A systematic review of image segmentation methodology, used in the additive manufacture of patient-specific 3D printed models of the cardiovascular system. JRSM Cardiovasc Dis. 2016; 5:2048004016645467.
Article6. Park JH, Lee Y, Shon OJ, Shon HC, Kim JW. Surgical tips of intramedullary nailing in severely bowed femurs in atypical femur fractures: simulation with 3D printed model. Injury. 2016; 47:1318–1324.
Article7. Chung KJ, Hong DY, Kim YT, Yang I, Park YW, Kim HN. Preshaping plates for minimally invasive fixation of calcaneal fractures using a real-size 3D-printed model as a preoperative and intraoperative tool. Foot Ankle Int. 2014; 35:1231–1236.
Article8. Jeong HS, Park KJ, Kil KM, et al. Minimally invasive plate osteosynthesis using 3D printing for shaft fractures of clavicles: technical note. Arch Orthop Trauma Surg. 2014; 134:1551–1555.
Article9. Parchi PD, Ferrari V, Piolanti N, et al. Computer tomography prototyping and virtual procedure simulation in difficult cases of hip replacement surgery. Surg Technol Int. 2013; 23:228–234.10. Cherkasskiy L, Caffrey JP, Szewczyk AF, et al. Patient-specific 3D models aid planning for triplane proximal femoral osteotomy in slipped capital femoral epiphysis. J Child Orthop. 2017; 11:147–153.
Article11. Qiao F, Li D, Jin Z, Hao D, Liao Y, Gong S. A novel combination of computer-assisted reduction technique and three dimensional printed patient-specific external fixator for treatment of tibial fractures. Int Orthop. 2016; 40:835–841.
Article12. Qiao F, Li D, Jin Z, et al. Application of 3D printed customized external fixator in fracture reduction. Injury. 2015; 46:1150–1155.
Article13. Shuang F, Hu W, Shao Y, Li H, Zou H. Treatment of intercondylar humeral fractures with 3D-printed osteosynthesis plates. Medicine (Baltimore). 2016; 95:e2461.
Article14. Chung SS, Lee KJ, Kwon YB, Kang KC. Characteristics and efficacy of a new 3-dimensional printed mesh structure titanium alloy spacer for posterior lumbar interbody fusion. Orthopedics. 2017; 40:e880–e885.
Article15. Li H, Qu X, Mao Y, Dai K, Zhu Z. Custom acetabular cages offer stable fixation and improved hip scores for revision THA with severe bone defects. Clin Orthop Relat Res. 2016; 474:731–740.
Article16. Kaneyama S, Sugawara T, Sumi M. Safe and accurate midcervical pedicle screw insertion procedure with the patient-specific screw guide template system. Spine (Phila Pa 1976). 2015; 40:E341–E348.
Article17. Chen H, Guo K, Yang H, Wu D, Yuan F. Thoracic pedicle screw placement guide plate produced by three-dimensional (3-D) laser printing. Med Sci Monit. 2016; 22:1682–1686.
Article18. Chen H, Wu D, Yang H, Guo K. Clinical use of 3D printing guide plate in posterior lumbar pedicle screw fixation. Med Sci Monit. 2015; 21:3948–3954.
Article19. Hirao M, Ikemoto S, Tsuboi H, et al. Computer assisted planning and custom-made surgical guide for malunited pronation deformity after first metatarsophalangeal joint arthrodesis in rheumatoid arthritis: a case report. Comput Aided Surg. 2014; 19:13–19.
Article20. Imanishi J, Choong PF. Three-dimensional printed calcaneal prosthesis following total calcanectomy. Int J Surg Case Rep. 2015; 10:83–87.
Article21. Wei R, Guo W, Ji T, Zhang Y, Liang H. One-step reconstruction with a 3D-printed, custom-made prosthesis after total en bloc sacrectomy: a technical note. Eur Spine J. 2017; 26:1902–1909.
Article22. Wong KC, Kumta SM. Joint-preserving tumor resection and reconstruction using image-guided computer navigation. Clin Orthop Relat Res. 2013; 471:762–773.
Article23. Wong KC, Kumta SM, Geel NV, Demol J. One-step reconstruction with a 3D-printed, biomechanically evaluated custom implant after complex pelvic tumor resection. Comput Aided Surg. 2015; 20:14–23.
Article24. Wong KC, Kumta SM, Sze KY, Wong CM. Use of a patient-specific CAD/CAM surgical jig in extremity bone tumor resection and custom prosthetic reconstruction. Comput Aided Surg. 2012; 17:284–293.
Article25. Fletcher CD, Bridge JA, Hogendoorn PCW. WHO classification of tumours of soft tissue and bone. Lyon: International Agency for Research on Cancer;2013.26. Wong KC, Kumta SM, Leung KS, Ng KW, Ng EW, Lee KS. Integration of CAD/CAM planning into computer assisted orthopaedic surgery. Comput Aided Surg. 2010; 15:65–74.
Article27. Wong KC, Sze KY, Wong IO, Wong CM, Kumta SM. Patient-specific instrument can achieve same accuracy with less resection time than navigation assistance in periacetabular pelvic tumor surgery: a cadaveric study. Int J Comput Assist Radiol Surg. 2016; 11:307–316.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of Three-Dimensional Printing Technology in Craniofacial Plastic Surgery
- Application of Three-Dimensional Printing in the Fracture Management
- Application of 3-dimensional printing implants for bone tumors
- Three-Dimensional Printing Technology in Orthopedic Surgery
- Emergence of Three-Dimensional Printing Technology and Its Utility in Spine Surgery