Korean J Radiol.
2019 Jan;20(1):58-68. 10.3348/kjr.2018.0012.
Factors Affecting Breast Cancer Detectability on Digital Breast Tomosynthesis and Two-Dimensional Digital Mammography in Patients with Dense Breasts
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. kimsmlms@daum.net
- 2Department of Radiology, Chungbuk National University Hospital, Cheongju, Korea.
- 3Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 4Division of Biomedical Engineering, Hankuk University of Foreign Studies, Yongin, Korea.
- 5Department of Radiology, Gyeongsang National University Hospital and College of Medicine, Gyeongsang National University, Jinju, Korea.
- KMID: 2429920
- DOI: http://doi.org/10.3348/kjr.2018.0012
Abstract
OBJECTIVE
To compare digital breast tomosynthesis (DBT) and conventional full-field digital mammography (FFDM) in the detectability of breast cancers in patients with dense breast tissue, and to determine the influencing factors in the detection of breast cancers using the two techniques.
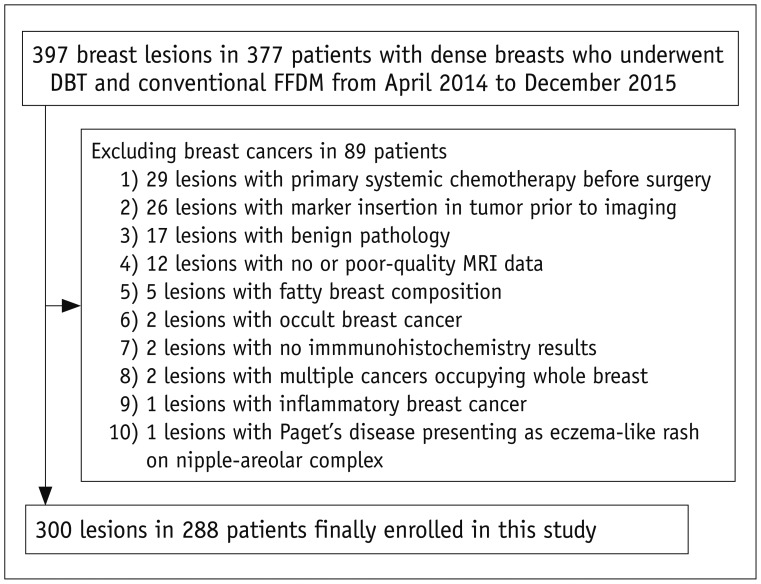
MATERIALS AND METHODS
Three blinded radiologists independently graded cancer detectability of 300 breast cancers (288 women with dense breasts) on DBT and conventional FFDM images, retrospectively. Hormone status, histologic grade, T stage, and breast cancer subtype were recorded to identify factors affecting cancer detectability. The Wilcoxon signed-rank test was used to compare cancer detectability by DBT and conventional FFDM. Fisher's exact tests were used to determine differences in cancer characteristics between detectability groups. Kruskal-Wallis tests were used to determine whether the detectability score differed according to cancer characteristics.
RESULTS
Forty breast cancers (13.3%) were detectable only with DBT; 191 (63.7%) breast cancers were detected with both FFDM and DBT, and 69 (23%) were not detected with either. Cancer detectability scores were significantly higher for DBT than for conventional FFDM (median score, 6; range, 0-6; p < 0.001). The DBT-only cancer group had more invasive lobular-type breast cancers (22.5%) than the other two groups (i.e., cancer detected on both types of image [both-detected group], 5.2%; cancer not detected on either type of image [both-non-detected group], 7.3%), and less detectability of ductal carcinoma in situ (5% vs. 16.8% [both-detected group] vs. 27.5% [both-non-detected group]). Low-grade cancers were more often detected in the DBT-only group than in the both-detected group (22.5% vs. 10%, p = 0.026). Human epidermal growth factor receptor-2 (HER-2)-negative cancers were more often detected in the DBT-only group than in the both-detected group (92.3% vs. 70.5%, p = 0.004). Cancers surrounded by mostly glandular tissue were detected less often in the DBT only group than in the both-non-detected group (10% vs. 31.9%, p = 0.016). DBT cancer detectability scores were significantly associated with cancer type (p = 0.012), histologic grade (p = 0.013), T and N stage (p = 0.001, p = 0.024), proportion of glandular tissue surrounding lesions (p = 0.013), and lesion type (p < 0.001).
CONCLUSION
Invasive lobular, low-grade, or HER-2-negative cancer is more detectable with DBT than with conventional FFDM in patients with dense breasts, but cancers surrounded by mostly glandular tissue might be missed with both techniques.
Keyword
MeSH Terms
Figure
Reference
-
1. Pisano ED, Gatsonis C, Hendrick E, Yaffe M, Baum JK, Acharyya S, et al. Digital Mammographic Imaging Screening Trial (DMIST) Investigators Group. Diagnostic performance of digital versus film mammography for breast-cancer screening. N Engl J Med. 2005; 353:1773–1783. PMID: 16169887.
Article2. Kopans DB. The most recent breast cancer screening controversy about whether mammographic screening benefits women at any age: nonsense and nonscience. AJR Am J Roentgenol. 2003; 180:21–26. PMID: 12490471.
Article3. Baker JA, Lo JY. Breast tomosynthesis: state-of-the-art and review of the literature. Acad Radiol. 2011; 18:1298–1310. PMID: 21893296.4. Lei J, Yang P, Zhang L, Wang Y, Yang K. Diagnostic accuracy of digital breast tomosynthesis versus digital mammography for benign and malignant lesions in breasts: a meta-analysis. Eur Radiol. 2014; 24:595–602. PMID: 24121712.
Article5. Yang TL, Liang HL, Chou CP, Huang JS, Pan HB. The adjunctive digital breast tomosynthesis in diagnosis of breast cancer. Biomed Res Int. 2013; 6. 17. [Epub]. DOI: 10.1155/2013/597253.
Article6. Mun HS, Kim HH, Shin HJ, Cha JH, Ruppel PL, Oh HY, et al. Assessment of extent of breast cancer: comparison between digital breast tomosynthesis and full-field digital mammography. Clin Radiol. 2013; 68:1254–1259. PMID: 23969151.
Article7. Gilbert FJ, Tucker L, Gillan MG, Willsher P, Cooke J, Duncan KA, et al. Accuracy of digital breast tomosynthesis for depicting breast cancer subgroups in a UK retrospective reading study (TOMMY Trial). Radiology. 2015; 277:697–706. PMID: 26176654.
Article8. Kim JY, Kang HJ, Shin JK, Lee NK, Song YS, Nam KJ, et al. Biologic profiles of invasive breast cancers detected only with digital breast tomosynthesis. AJR Am J Roentgenol. 2017; 209:1411–1418. PMID: 28834445.
Article9. Skaane P, Bandos AI, Gullien R, Eben EB, Ekseth U, Haakenaasen U, et al. Comparison of digital mammography alone and digital mammography plus tomosynthesis in a population-based screening program. Radiology. 2013; 267:47–56. PMID: 23297332.
Article10. Ciatto S, Houssami N, Bernardi D, Caumo F, Pellegrini M, Brunelli S, et al. Integration of 3D digital mammography with tomosynthesis for population breast-cancer screening (STORM): a prospective comparison study. Lancet Oncol. 2013; 14:583–589. PMID: 23623721.
Article11. Rose SL, Tidwell AL, Bujnoch LJ, Kushwaha AC, Nordmann AS, Sexton R Jr. Implementation of breast tomosynthesis in a routine screening practice: an observational study. AJR Am J Roentgenol. 2013; 200:1401–1408. PMID: 23701081.
Article12. Greenberg JS, Javitt MC, Katzen J, Michael S, Holland AE. Clinical performance metrics of 3D digital breast tomosynthesis compared with 2D digital mammography for breast cancer screening in community practice. AJR Am J Roentgenol. 2014; 203:687–693. PMID: 24918774.
Article13. Andersson I, Ikeda DM, Zackrisson S, Ruschin M, Svahn T, Timberg P, et al. Breast tomosynthesis and digital mammography: a comparison of breast cancer visibility and BIRADS classification in a population of cancers with subtle mammographic findings. Eur Radiol. 2008; 18:2817–2825. PMID: 18641998.
Article14. Nakashima K, Uematsu T, Itoh T, Takahashi K, Nishimura S, Hayashi T, et al. Comparison of visibility of circumscribed masses on Digital Breast Tomosynthesis (DBT) and 2D mammography: are circumscribed masses better visualized and assured of being benign on DBT? Eur Radiol. 2017; 27:570–577. PMID: 27236817.
Article15. Nam KJ, Han BK, Ko ES, Choi JS, Ko EY, Jeong DW, et al. Comparison of full-field digital mammography and digital breast tomosynthesis in ultrasonography-detected breast cancers. Breast. 2015; 24:649–655. PMID: 26292782.
Article16. Svahn TM, Chakraborty DP, Ikeda D, Zackrisson S, Do Y, Mattsson S, et al. Breast tomosynthesis and digital mammography: a comparison of diagnostic accuracy. Br J Radiol. 2012; 85:e1074–e1082. PMID: 22674710.
Article17. Wang WS, Hardesty L, Borgstede J, Takahashi J, Sams S. Breast cancers found with digital breast tomosynthesis: a comparison of pathology and histologic grade. Breast J. 2016; 22:651–656. PMID: 27870337.
Article18. Bernardi D, Macaskill P, Pellegrini M, Valentini M, Fantò C, Ostillio L, et al. Breast cancer screening with tomosynthesis (3D mammography) with acquired or synthetic 2D mammography compared with 2D mammography alone (STORM-2): a population-based prospective study. Lancet Oncol. 2016; 17:1105–1113. PMID: 27345635.
Article19. Lång K, Andersson I, Zackrisson S. Breast cancer detection in digital breast tomosynthesis and digital mammography-a side-by-side review of discrepant cases. Br J Radiol. 2014; 87:20140080. PMID: 24896197.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Digital Mammography
- Mammography-Guided Interventional Procedure
- Digital Breast Tomosynthesis Screening
- Digital Breast Tomosynthesis versus MRI as an Adjunct to Full-Field Digital Mammography for Preoperative Evaluation of Breast Cancer according to Mammographic Density
- Performance of Digital Mammography-Based Artificial Intelligence Computer-Aided Diagnosis on Synthetic Mammography From Digital Breast Tomosynthesis