J Periodontal Implant Sci.
2018 Dec;48(6):395-404. 10.5051/jpis.2018.48.6.395.
Periodontal biotype modification using a volume-stable collagen matrix and autogenous subepithelial connective tissue graft for the treatment of gingival recession: a case series
- Affiliations
-
- 1Department of Periodontics, Seoul National University Dental Hospital, Seoul, Korea.
- 2Department of Periodontology, Dental Research Institute, Seoul National University School of Dentistry, Seoul, Korea. kst72@snu.ac.kr
- 3Department of Restorative Dentistry, University at Buffalo School of Dental Medicine, Buffalo, NY, USA.
- KMID: 2429867
- DOI: http://doi.org/10.5051/jpis.2018.48.6.395
Abstract
- PURPOSE
The purpose of this study was to propose a technique for periodontal biotype modification through thickening of the entire facial aspect using a volume-stable collagen matrix and autogenous subepithelial connective tissue graft (CTG) for the treatment of gingival recession.
METHODS
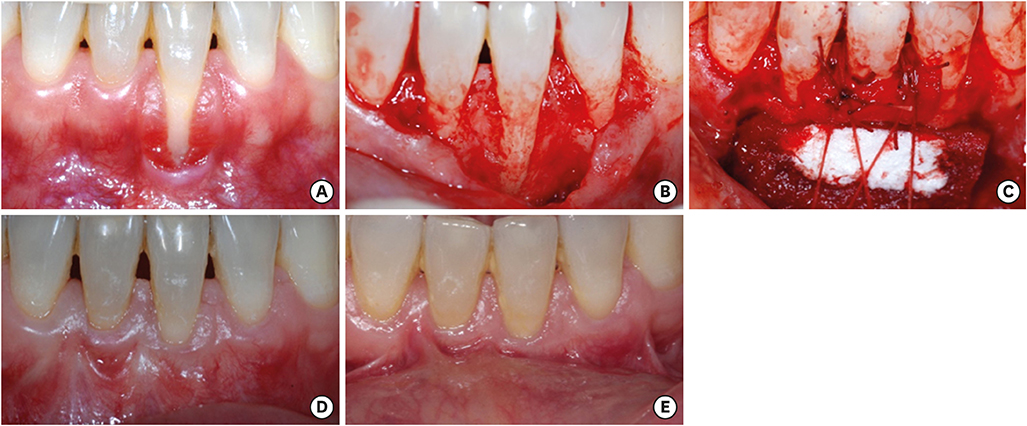
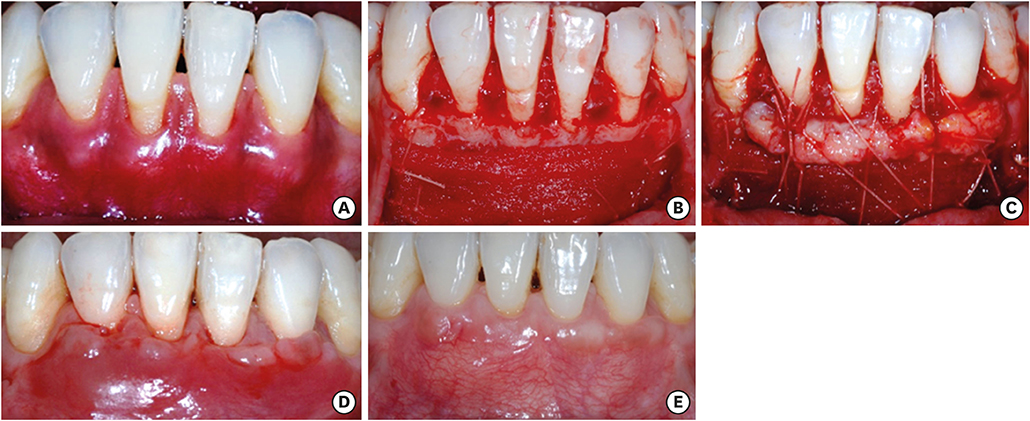
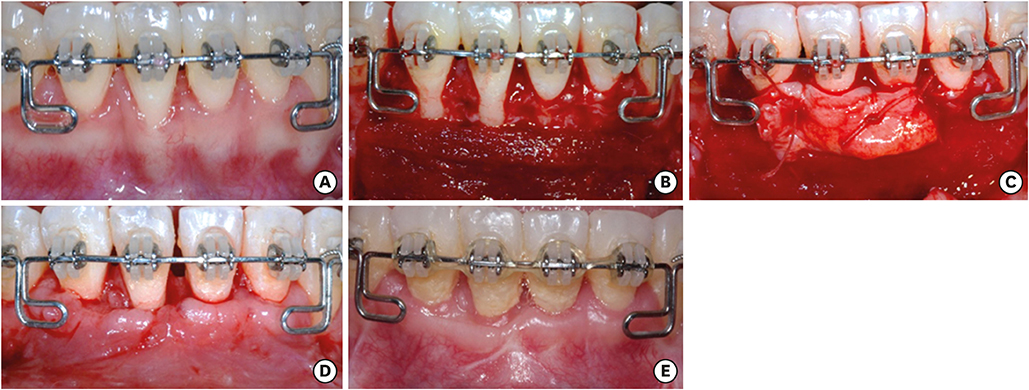
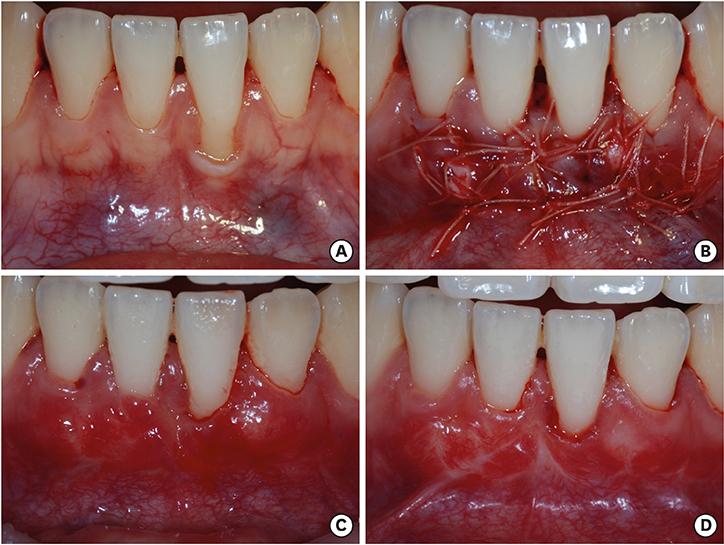
Four systemically healthy patients showing Miller class I or class II gingival recession in the mandibular incisor area were included in this study. Full-mouth scaling and root planing procedures were performed at least 4 weeks prior to periodontal plastic surgery. A split-thickness flap with a horizontal intrasulcular incision and 2 vertical incisions was used in cases 1-3, and the modified tunnel technique was used in case 4 for coronal advancement of the mucogingival complex. After the exposed root surfaces were debrided thoroughly, double-layered volume-stable collagen matrix was placed on the apical part of the recession and a subepithelial CTG harvested from the palatal area was placed on the coronal part. The amount of root coverage at 3 months postoperatively was evaluated in cases 1-3, and facio-lingual volumetric changes were analyzed in cases 1 and 2.
RESULTS
Healing was uneventful in all 4 cases and complete root coverage was shown in cases 1-3. In case 4, reduction of gingival recession was observed at 3 months after surgery. In cases 1 and 2, a comparison of stereolithographic files from the preoperative and postoperative time points demonstrated that the entire facio-lingual volume had increased.
CONCLUSIONS
The surgical technique suggested herein, using a volume-stable collagen matrix and autogenous subepithelial CTG, may be an effective method for periodontal biotype modification through thickening of the entire facial aspect for the treatment of gingival recession.
MeSH Terms
Figure
Cited by 1 articles
-
Evaluation of 2 techniques of epithelial removal in subepithelial connective tissue graft surgery: a comparative histological study
Paola Marques de Mattos, Vula Papalexiou, Vinícius Augusto Tramontina, Sung Hyun Kim, Sônia Mara Luczyszyn, Patrícia Vida Cassi Bettega, Aline Cristina Batista Rodrigues Johann
J Periodontal Implant Sci. 2020;50(1):2-13. doi: 10.5051/jpis.2020.50.1.2.
Reference
-
1. Hall WB. Present status of soft tissue grafting. J Periodontol. 1977; 48:587–597.
Article2. Radentz WH, Barnes GP, Cutright DE. A survey of factors possibly associated with cervical abrasion of tooth surfaces. J Periodontol. 1976; 47:148–154.
Article3. Geiger AM. Malocclusion as an etiologic factor in periodontal disease: a retrospective essay. Am J Orthod Dentofacial Orthop. 2001; 120:112–115.
Article4. Geiger AM, Wasserman BH. Relationship of occlusion and periodontal disease: part IX-incisor inclination and periodontal status. Angle Orthod. 1976; 46:99–110.5. Reed J. Recession of mandibular anterior gingival following orthodontics in adults. Todays FDA. 2005; 17:45.6. Zimmer B, Seifi-Shirvandeh N. Changes in gingival recession related to orthodontic treatment of traumatic deep bites in adults. J Orofac Orthop. 2007; 68:232–244.
Article7. Tilliss TS, Keating JG. Understanding and managing dentin hypersensitivity. J Dent Hyg. 2002; 76:296–310. quiz 311-3.8. Joshipura KJ, Kent RL, DePaola PF. Gingival recession: intra-oral distribution and associated factors. J Periodontol. 1994; 65:864–871.
Article9. Bouchard P, Malet J, Borghetti A. Decision-making in aesthetics: root coverage revisited. Periodontol 2000. 2001; 27:97–120.
Article10. Harris RJ. Root coverage with connective tissue grafts: an evaluation of short- and long-term results. J Periodontol. 2002; 73:1054–1059.
Article11. Müller HP, Eger T, Schorb A. Gingival dimensions after root coverage with free connective tissue grafts. J Clin Periodontol. 1998; 25:424–430.
Article12. Tarnow DP. Semilunar coronally repositioned flap. J Clin Periodontol. 1986; 13:182–185.
Article13. Zucchelli G, Mounssif I. Periodontal plastic surgery. Periodontol 2000. 2015; 68:333–368.
Article14. Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root-coverage procedures for the treatment of localized recession-type defects: a Cochrane systematic review. J Periodontol. 2010; 81:452–478.
Article15. Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985; 56:715–720.
Article16. Seibert JL, Lindhe J. Esthetics and periodontal therapy. In : Lindhe J, editor. Textbook of clinical periodontology. Copenhangen: Munksgaard;1989. p. 477–514.17. Cohen ES. Atlas of cosmetic and reconstructive periodontal surgery. 3rd ed. Hamilton: BC Decker Inc.;2007.18. Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010; 81:569–574.
Article19. Ahmad I. Anterior dental aesthetics: gingival perspective. Br Dent J. 2005; 199:195–202.
Article20. Hürzeler MB, Weng D. A single-incision technique to harvest subepithelial connective tissue grafts from the palate. Int J Periodontics Restorative Dent. 1999; 19:279–287.21. Kolte R, Kolte A, Mahajan A. Assessment of gingival thickness with regards to age, gender and arch location. J Indian Soc Periodontol. 2014; 18:478–481.
Article22. Allen EP, Miller PD Jr. Coronal positioning of existing gingiva: short term results in the treatment of shallow marginal tissue recession. J Periodontol. 1989; 60:316–319.23. Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontol. 2008; 35:Suppl. 136–162.
Article24. Cairo F, Nieri M, Pagliaro U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J Clin Periodontol. 2014; 41:Suppl 15. S44–S62.
Article25. Allen AL. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int J Periodontics Restorative Dent. 1994; 14:216–227.26. Yeung SC. Biological basis for soft tissue management in implant dentistry. Aust Dent J. 2008; 53:Suppl 1. S39–S42.
Article27. Heitz F, Heitz-Mayfield LJ, Lang NP. Effects of post-surgical cleansing protocols on early plaque control in periodontal and/or periimplant wound healing. J Clin Periodontol. 2004; 31:1012–1018.
Article28. Lang NP, Joss A, Tonetti MS. Monitoring disease during supportive periodontal treatment by bleeding on probing. Periodontol 2000. 1996; 12:44–48.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laterally positioned flap using subepithelial connective tissue graft for iatrogenic gingival recession treatment
- Influence of gingival biotype on the amount of root coverage following the connective tissue graft
- Periodontal regenerative treatment with connective tissue grafts in deep intrabony defect and gingival recession in the maxillary canine: a case report with 3-year follow-up
- The laterally closed tunnel for the treatment of mandibular gingival recession in thin biotype patients: case report
- Root coverage with subeptithelial connective tissue grafts