Asian Oncol Nurs.
2018 Jun;18(2):104-113. 10.5388/aon.2018.18.2.104.
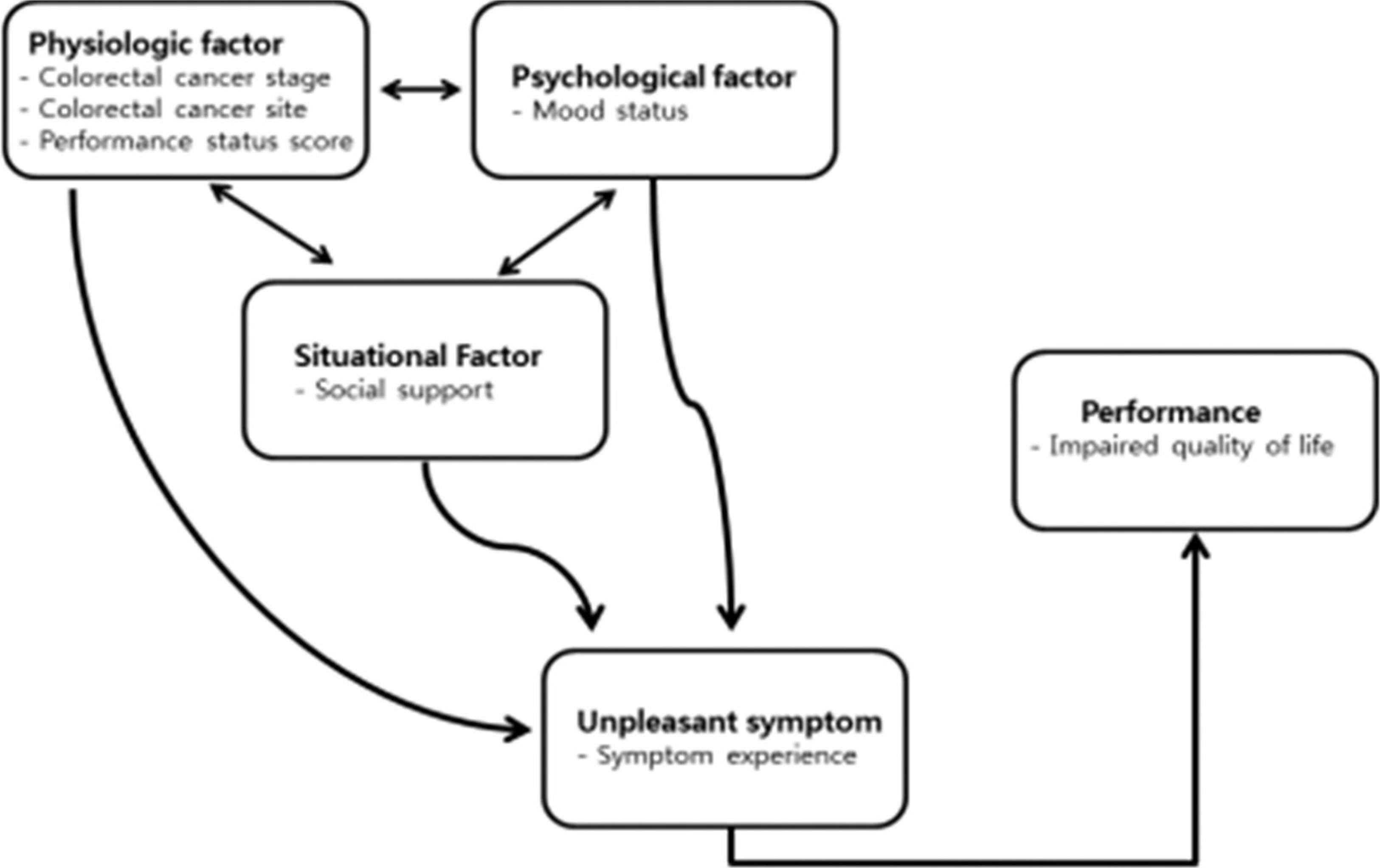
Relationships among Mood Status, Social Support, Symptom Experience and Quality of Life in Colorectal Cancer Patients - based on the Theory of Unpleasant Symptoms
- Affiliations
-
- 1Department of Nursing, Inha University Hospital, Incheon, Korea.
- 2Department of Nursing, Chung-Ang University, Seoul, Korea. go2ryu@cau.ac.kr
- 3Department of Nursing, Kyungmin University, Ujeongbu-si, Korea.
- KMID: 2429028
- DOI: http://doi.org/10.5388/aon.2018.18.2.104
Abstract
- PURPOSE
This study is to determine the effects of Colorectal Neoplasms patients' stage, location of disease, functional status (physiological factor), mood (psychological factor), and social support (situational factor) on their symptom experience, and to verify the relationship between symptom experience and the quality of life.
METHODS
The Theory of Unpleasant Symptoms was the framework for the study. A descriptive correlational design was used in analysis of data obtained from a sample of 113 Colorectal Neoplasms patients who were undergoing chemotherapy.
RESULTS
Total mood disturbance and symptom experiences were negatively correlated with physical component score (PCS) and mental component score (MCS) of quality of life (r −.33 to r=−.51, p<.001; r=.40 to r=.50, p<.001). Multiple regression analysis revealed that the functional status and symptoms interference variables explained 29.2% of the variance in PCS of quality of life. Symptoms interference and age explained 30.6% of the variance in MCS of quality of life.
CONCLUSION
Although overall depression levels were low in this sample, these findings suggest that insomnia and fatigue are related to depression and that depression is more closely associated with quality of life than are insomnia and fatigue.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Factors influencing the health-related quality of life in Korean menopausal women: a cross-sectional study based on the theory of unpleasant symptoms
Ji-Hyun Kang, Moon-Jeong Kim
Korean J Women Health Nurs. 2022;28(2):100-111. doi: 10.4069/kjwhn.2022.05.29.
Reference
-
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–86.
Article2. National Cancer Information Center (KR). Annual report of cancer statistics in Korean: cancer incidence [Internet]. Available from. https://www.cancer.go.kr/lay1/S1T639C640/contents.do. [Accessed January 9, 2018].3. Jung KW, Won YJ, Oh CM, Kong HJ, Lee DH, Lee KH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017; 49:292–305.
Article4. National Cancer Information Center (KR). Annual report of cancer statistics in Korean: 5-year relative survival rate [Internet]. Available from. https://www.cancer.go.kr/lay1/S1T648C650/contents.do. [Accessed May 4, 2018].5. Jeong G, Kim K, Kwak Y. Quality of life in colorectal cancer patients according to the severity of symptom clusters classification. Asian Oncol Nurs. 2014; 14:74–83.
Article6. Ali WG, Ayoub NS. Nurses' attitudes toward caring for dying patient in Mansoura university hospitals. J Med Biomed Sci. 2010; 1:16–23.7. Wong P, Reker G, Gesser G. Death attitude profile-revised: a multidimensional measure of attitudes toward death. Washington, DC: Taylor & Francis;1994.8. Kim SH, Choi YS, Shin SW, Chong MK, Lee SN, Lee SW, et al. Development of education program for physicians based on the 2004 hos-pice palliative model project for terminal cancer. Korean J Hosp Palliat Care. 2006; 9:67–76.9. Lenz ER, Pugh LC, Milligan RA, Gift A, Suppe F. The middle-range theory of unpleasant symptoms: an update. ANS Adv Nurs Sci. 1997; 19:14–27.
Article10. Kim HJ, Kim SH, Lee HK, Oh SE. Factors affecting symptom experiences of breast cancer patients - based on the theory of unpleasant symptoms. Asian Oncol Nurs. 2014; 14:7–14.11. Keum KS, Yi M, Bang KS, Cho YA, Lee JL, Lee E. Relationships among activity status, anxiety, depression, social support, symptom experience, and functional status in lung cancer patients based on the theory of unpleasant symptoms. Perspect Nurs Sci. 2013; 10:87–96.12. Kim JS, Seo YS. Factors influencing on quality of life in patients with liver cirrhosis: convergence on the theory of unpleasant symptoms. J Digit Converg. 2015; 13:271–81.
Article13. Lee HJ. Functional status, symptom experience and influential factors in gastric cancer patients with gastrectomy based on the theory of unpleasant symptoms [dissertation]. Seoul: Yonsei Univ.;2015.14. Zubrod CG, Schneiderman M, Frei E 3rd, Brindley C, Lennard Gold G, Shnider B, et al. Appraisal of methods for the study of chemotherapy of cancer in man: comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J Chronic Dis. 1960; 11:7–33.
Article15. Cohen J. A power primer. Psychol Bull. 1992; 112:155–9.
Article16. Yeun EJ, Shin-Park KK. Verification of the profile of mood states-brief: cross-cultural analysis. J Clin Psychol. 2006; 62:1173–80.
Article17. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988; 52:30–41.
Article18. Shin JS, Lee YB. The effects of social supports on psychosocial well-being of the unemployed. Korean J Soc Welf. 1999; 37:241–69.19. Baek Y. The correlation among symptoms, anxiety, depression and quality of life in patients with colorectal cancer undergoing chemotherapy [dissertation]. Seoul: Seoul National Univ.;2013.20. Yun YH, Mendoza TR, Kang IO, You CH, Roh JW, Lee CG, et al. Validation study of the Korean version of the M. D. Anderson Symptom Inventory. J Pain Symptom Manage. 2006; 31:345–52.
Article21. Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34:220–33.22. Lee I. The effect of communication on marital adjustment of cancer patients and their spouses - focusing on the actor effect and partner effect -. Korean J Soc Welf. 2011; 63:179–205.23. Park EJ, Jeon YW, Han SI, Oh SJ. A preliminary study on the quality of life for patients who had breast cancer operations. J Korean Breast Cancer Soc. 2004; 7:299–305.
Article24. Cha K, Kim K. Impact of uncertainty on resilience in cancer patients. Asian Oncol Nurs. 2012; 12:139–46.
Article25. Kwon EJ, Yi M. Distress and quality of life in breast cancer survivors in Korea. Asian Oncol Nurs. 2012; 12:289–96.
Article26. Cho OH, Yoo YS. Psychosocial adjustment, marital intimacy and family support of post-mastectomy patients. J Korean Oncol Nurs. 2009; 9:129–35.27. Kim HJ, Kwon JH, Kim JN, Lee R, Lee KS. Posttraumatic growth and related factors in breast cancer survivors. Korean J Health Psychol. 2008; 13:781–99.28. Jo H, Kim B, Lee H, Lee B. Perceived social support as influencing factors on quality of life among cancer patients. Korean J Health Educ Promot. 2010; 27:51–9.29. Kim HJ, Chu SH, Yoo JS, Kim NK. Nutritional risk and physical activity on quality of life in patients with colorectal cancer. Asian Oncol Nurs. 2014; 14:66–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationships of Mood Disturbance, Symptom Experience, and Attentional Function in Women with Breast Cancer Based upon the Theory of Unpleasant Symptoms
- Moderating Effect of Inner Strength between Mood Status and Quality of Life in Female Patients with Lung Cancer
- Analysis and Evaluation of the Theory of Unpleasant Symptoms
- Factors influencing the health-related quality of life in Korean menopausal women: a cross-sectional study based on the theory of unpleasant symptoms
- Self-care in Patients with Atrial Fibrillation Based on the Theory of Unpleasant Symptoms