J Korean Ophthalmol Soc.
2018 Dec;59(12):1114-1121. 10.3341/jkos.2018.59.12.1114.
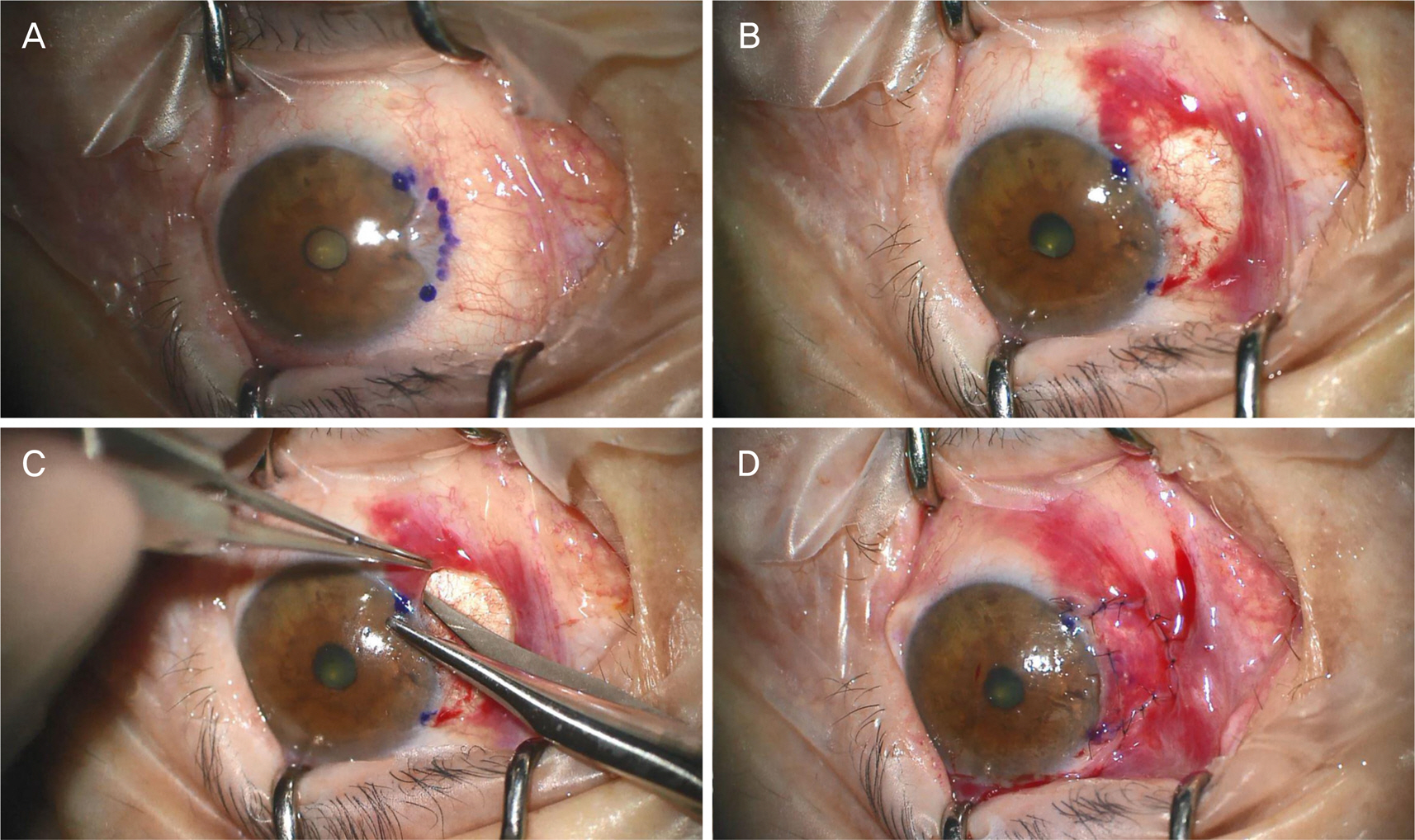
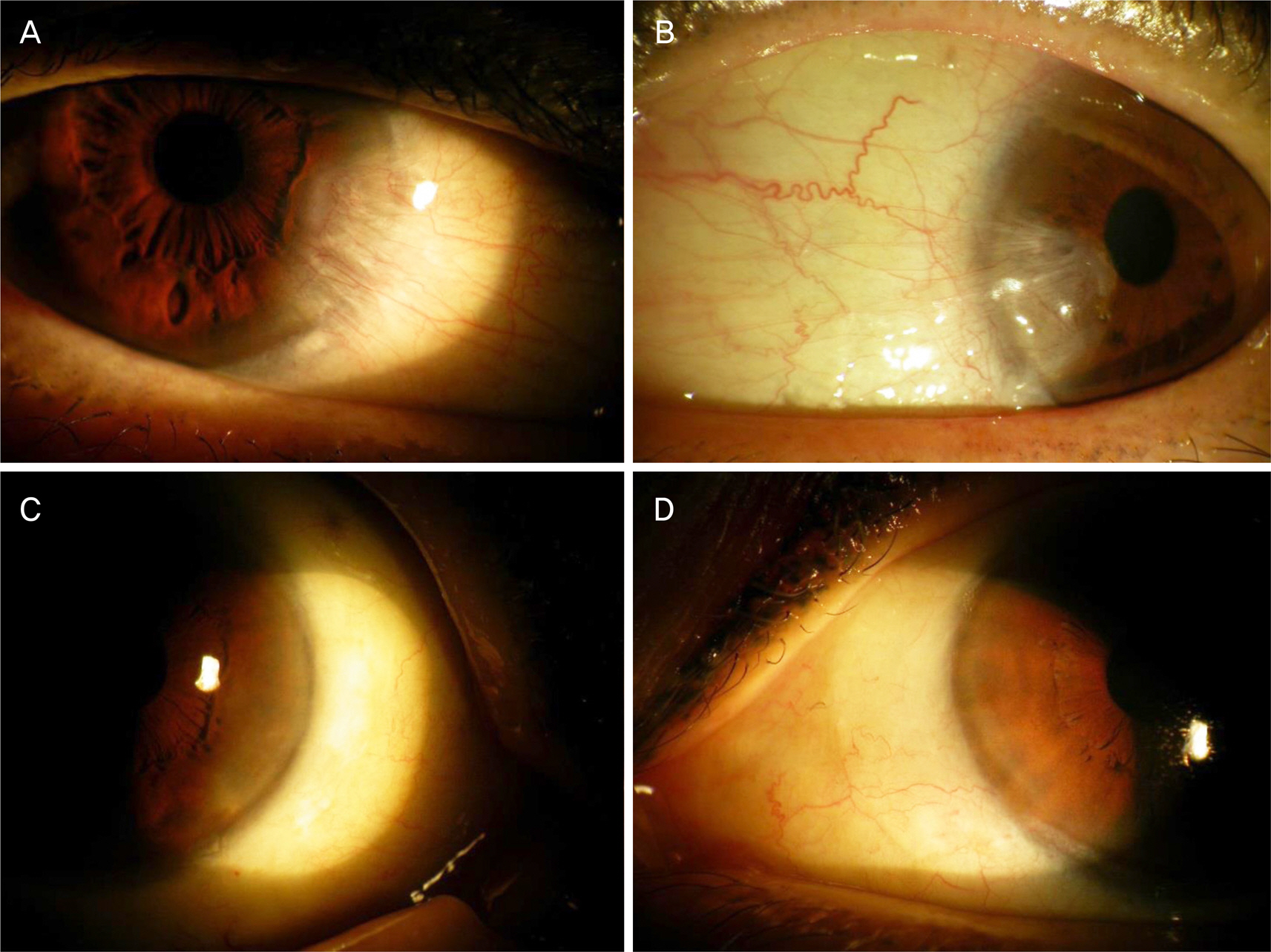
Long-term Outcomes of Conjunctivo-limbal Autograft Alone and Additional Widening of Limbal Incision in Recurrent Pterygia
- Affiliations
-
- 1Department of Ophthalmology, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea. eyedr0823@hotmail.com
- KMID: 2428682
- DOI: http://doi.org/10.3341/jkos.2018.59.12.1114
Abstract
- PURPOSE
We report the clinical outcomes of patients undergoing additional widening of the limbal incision to prevent disease recurrence after conjunctivo-limbal autograft combined with pterygial excision.
METHODS
We retrospectively compared 95 eyes with primary and 12 eyes with recurrent pterygia randomized to treatment via two surgical methods: conjunctivo-limbal autograft alone and combined with widening of the limbal incision to allow for pterygial removal. We widened the limbal incisions by 1 mm on both the superior and inferior limbal margins and removed the pterygia. The outcomes were compared between 39 eyes undergoing conjunctivo-limbal autograft alone and 68 eyes undergoing conjunctivo- limbal autograft with widening of the limbal incision.
RESULTS
The mean overall postoperative follow-up period was 29.6 ± 10.5 months and conjunctivo-limbal autograft alone group was 27.4 ± 11.5 months, combined with widening of the limbal incision group was 30.7 ± 9.7 months. Six pterygia (15.4%; four primary and two recurrent) developed in those undergoing conjunctivo-limbal autograft alone and two (2.9%; one primary and one recurrent) in those undergoing additional widening of the limbal incision; the recurrence rate differed significantly between the two groups (p < 0.05). In the group treated with conjunctivo-limbal autograft alone, the mean time to development of a new primary pterygium was 6.3 ± 3.4 months and that to development of a recurrent pterygium 4.3 ± 2.5 months; the respective values for the group undergoing additional widening of the limbal incision were 12.1 ± 2.6 and 8.4 ± 4.6 months; the recurrence rates differed significantly (p < 0.05).
CONCLUSIONS
Conjunctivo-limbal autograft with additional widening of the limbal incision used to treat both new primary and recurrent pterygia was more effective in terms of reducing pterygial recurrence than conjunctivo-limbal aAutograft alone.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Taylor HR, West S, Muñoz B, et al. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992; 110:99–104.
Article2. Di Girolamo N, Chui J, Coroneo MT, Wakefield D. Pathogenesis of pterygia: role of cytokines, growth factors, and matrix metalloproteinases. Prog Retin Eye Res. 2004; 23:195–228.
Article3. Chui J, Coroneo MT, Tat LT, et al. Ophthalmic pterygium: a stem cell disorder with premalignant features. Am J Pathol. 2011; 178:817–27.4. Kim YJ, Yoo SH, Chung JK. Reconstruction of the limbal vasculature after limbal-conjunctival autograft transplantation in abdominal surgery: an angiography study. Invest Ophthalmol Vis Sci. 2014; 55:7925–33.5. Rim H, Kang MJ, Choi M, et al. The incidence and prevalence of pterygium in South Korea: a 10-year population-based Korean abdominal study. PLoS One. 2017; 12:e0171954.6. Kim DI, Kim MK, Wee WR, Oh JY. Surgical outcome of primary pterygium excision with conjunctival autograft. J Korean Ophthalmol Soc. 2015; 56:856–62.
Article7. Ang LP, Chua JL, Tan DT. Current concepts and techniques in pterygium treatment. Curr Opin Ophthalmol. 2007; 18:308–13.
Article8. Hong SM, Ko SJ, Kim SD. Effect of inferior conjunctival abdominal flap surgery for primary pterygium. J Korean Ophthalmol Soc. 2009; 50:1774–9.9. Gris O, Güell JL, del Campo Z. Limbal-conjunctival autograft abdominal for the treatment of recurrent pterygium. Ophthalmology. 2000; 107:270–3.10. Zheng K, Cai J, Jhanji V, Chen H. Comparison of pterygium abdominal rates after limbal conjunctival autograft transplantation and other techniques: meta-analysis. Cornea. 2012; 31:1422–7.11. Tan DT, Chee SP, Dear KB, Lim AS. Effect of pterygium abdominal on pterygium recurrence in a controlled trial comparing abdominal autografting with bare sclera excision. Arch Ophthalmol. 1997; 115:1235–40.12. Allan BD, Short P, Crawford GJ, et al. Pterygium excision with conjunctival autografting: an effective and safe technique. Br J Ophthalmol. 1993; 77:698–701.
Article13. Kwon SH, Kim HK. Analysis of recurrence patterns following pterygium surgery with conjunctival autografts. Medicine (Baltimore). 2015; 94:e518.
Article14. KEEDS. Cornea. 3rd ed.Seoul: Ilchokak Publishing Co., Ltd.;2013. p. 771–5.15. Tseng SC. Concept and application of limbal stem cells. Eye (Lond). 1989; 3(Pt 2):141–57.
Article16. Anquria P, Carmichael T, Ntuli S, Kitinya J. Chronic inflammatory cells and damaged limbal cells in pterygium. Afr Health Sci. 2013; 13:725–30.
Article17. Sebban A, Hirst LW. Pterygium recurrence rate at the Princess Alexandra Hospital. Aust N Z J Ophthalmol. 1991; 19:203–6.
Article18. Han HC, Kim JH, Lee DH. The changes of corneal higher-order aberrations after surgery according to pterygium size. J Korean Ophthalmol Soc. 2014; 55:32–9.
Article19. Hirst LW, Axelsen RA, Schwab I. Pterygium and associated ocular surface squamous neoplasia. Arch ophthalmol. 2009; 127:31–2.
Article20. Hacı oğ lu D1, Erdöl H. Developments and current approaches in the treatment of pterygium. Int Ophthalmol. 2017; 37:1073–81.
Article21. Young AL, Ho M, Jhanji V, Cheng LL. Ten-year results of a randomized controlled trial comparing 0.02% mitomycin C and limbal conjunctival autograft in pterygium surgery. Ophthalmology. 2013; 120:2390–5.
Article22. Murube J. Pterygium: its treatment with beta therapy. Ocul Surf. 2009; 7:3–9.
Article23. Khan MS, Malik S, Basit I. Effect of intralesional 5 fluorouracil abdominal in primary pterygium. Pak J med Sci. 2016; 32:130–3.
Article24. Rúa O, Larráyoz IM, Barajas MT, et al. Oral doxycycline reduces pterygium lesions; results from a double blind, randomized, abdominal controlled clinical trial. PLoS One. 2012; 7:e52696.25. Chen KH, Hsu WM. Intraoperative ethanol treatment as an adjuvant therapy of pterygium excision. Int J Biomed Sci. 2006; 2:414–21.26. Kim YI, Lee GY, Kim EJ, et al. The Effect of subconjunctival abdominal Injection before conjunctival autograft for pterygium. J Korean Ophthalmol Soc. 2015; 56:847–55.27. Besharati Manaviat, Souzani A. Subconjunctival bevacizumab abdominal in treatment of pterygium. Acta Med Iran. 2011; 49:179–83.28. Kim CH, Lee JK, Park DJ. Recurrence rates of amniotic membrane transplantation, conjunctival autograft and conjunctivolimbal abdominal in primary pterygium. J Korean Ophthalmol Soc. 2009; 50:1780–8.29. Gazzard G, Saw SM, Farook M, et al. Pterygium in Indonesia: prevalence, severity and risk factors. Br J Ophthalmol. 2002; 86:1341–6.
Article30. Kim KW, Kim JC. The clinical effect of micro-multiporous abdominal polyeterafluoroethylene insertion for recurrent pterygium. J Korean Ophthalmol Soc. 2013; 54:416–26.31. Kenyon KR, Tseng SC. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989; 96:709–22.
Article32. Hirst LW. Prospective study of primary pterygium surgery using pterygium extended removal followed by extended conjunctival transplantation. Ophthalmology. 2008; 115:1663–72.
Article33. Hirst LW. Recurrence and complications after 1,000 surgeries abdominal pterygium extended removal followed by extended abdominal transplant. Ophthalmology. 2012; 119:2205–10.34. Lee JS, Ha SW, Yu S, et al. Efficacy and safety of a large abdominal autograft for recurrent pterygium. J Korean Ophthalmol Soc. 2017; 31:469–78.35. Barraquer JI. Etiology, pathogenesis, and treatment of the pterygium. Trans New Orleans Acad Ophthalmol. 1980; 28:167–78.36. Kria L, Ohira A, Amemiya T. Growth factors in cultured pterygium fibroblasts: immunohistochemical and ELISA analysis. Graefes Arch Clin Exp Ophthalmol. 1998; 236:702–8.
Article37. Kria L, Ohira A, Amemiya T. TNP-470 (a fungus-derived inhibitor of angiogenesis) reduces proliferation of cultured fibroblasts abdominal from primary pterygia: a possible drug therapy for pterygia. Curr Eye Res. 1998; 17:986–93.38. John T. Pterygium excision and conjunctival mini-autograft: preliminary report. Eye (Lond). 2001; 15(Pt 3):292–6.
Article39. Hwang HS, Cho KJ, Rand G, et al. Optimal size of pterygium abdominal for limbal conjunctival autograft using fibrin glue in primary pterygia. BMC Ophthalmol. 2018; 18:135.
Article40. Bazzazi N, Ramezani A, Rabiee MA. A comparative study of abdominal autograft and minimally invasive pterygium surgery in primary pterygia. Pak J Biol Sci. 2010; 13:409–12.41. Masters JS, Harris DJ. Low recurrence rate of pterygium after abdominal with conjunctival Limbal autograft: a retrospective study with long-term follow-up. Cornea. 2015; 34:1569–72.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pterygium Surgery: Wide Excision with Conjunctivo-Limbal Autograft
- Analysis of Donor-site Complications after Conjunctivo-limbal Autograft to Treat Pterygium
- Effectiveness of Wide Excision of Subconjucntival Fibrovascular Tissue with Conjunctivo-Limbal Autograft in Pterygium Surgery
- Changes in Eye Movement Amplitude after Conjunctivo-Limbal Autograft in Patients with Recurrent Pterygium, Ocular Motility Restriction
- Limbal-Conjunctival Autograft Transplantation for the Treatment of Primary Pterygium