Arch Hand Microsurg.
2018 Dec;23(4):313-318. 10.12790/ahm.2018.23.4.313.
Two Cases of Pneumatic Tourniquet Paralysis: Points for Prevention
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Dankook University College of Medicine, Cheonan, Korea. kruezel@gmail.com
- KMID: 2427401
- DOI: http://doi.org/10.12790/ahm.2018.23.4.313
Abstract
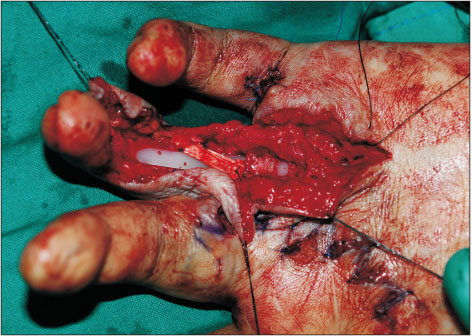
- Although nerve injury is the most common complication of pneumatic tourniquets, it is said to be rare, with few case reports. We describe two cases of paralysis after upper extremity surgery to highlight this risk. Ulnar, median and radial neuropathies were diagnosed after surgery was performed on a man for left hand reconstruction, presumably due to a prolonged total inflation time of 14 hours despite conventional break times. A woman who received surgery for a crushed hand presented with radial neuropathy, the most probable cause being malfunction and automatic inflation of the tourniquet. These cases illustrate the diversity of tourniquet paralysis, with symptomatic progress not necessarily following electromyography results. The considerable discomfort to patients warrants careful use of tourniquets for neuropathy prevention.
MeSH Terms
Figure
Reference
-
1. Wakai A, Winter DC, Street JT, Redmond PH. Pneumatic tourniquets in extremity surgery. J Am Acad Orthop Surg. 2001; 9:345–351.
Article2. Sharma JP, Salhotra R. Tourniquets in orthopedic surgery. Indian J Orthop. 2012; 46:377–383.
Article3. Van der Spuy L. Complications of the arterial tourniquet. South Afr J Anaesth Analg. 2012; 18:14–18.
Article4. Rudge P. Tourniquet paralysis with prolonged conduction block. An electro-physiological study. J Bone Joint Surg Br. 1974; 56:716–720.5. Aho K, Sainio K, Kianta M, Varpanen E. Pneumatic tourniquet paralysis. Case report. J Bone Joint Surg Br. 1983; 65:441–443.
Article6. Estebe JP, Davies JM, Richebe P. The pneumatic tourniquet: mechanical, ischaemia-reperfusion and systemic effects. Eur J Anaesthesiol. 2011; 28:404–411.
Article7. Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, León Alonso-Cortés JM, Monge-Casares E. Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: case report and review of the literature. Case Rep Orthop. 2013; 2013:368290.
Article8. Horlocker TT, Hebl JR, Gali B, et al. Anesthetic, patient, and surgical risk factors for neurologic complications after prolonged total tourniquet time during total knee arthroplasty. Anesth Analg. 2006; 102:950–955.
Article9. Feinberg J. EMG: myths and facts. HSS J. 2006; 2:19–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Measurement of the Soft Tissue Pressure beneath a Tourniquet in the Arm
- Tourniquet-induced Tibial Nerve Palsy Complicating Partial Lateral Meniscectomy: A case report
- Change in the effect of rocuronium after pneumatic tourniquet release in patients undergoing unilateral total knee arthroplasty
- Changes of Serum Myoglobin at Tourniquet Application
- A Case of Rhabdomyolysis Associated with Use of a Pneumatic Tourniquet during Arthroscopic Knee Surgery