Arch Hand Microsurg.
2018 Dec;23(4):248-253. 10.12790/ahm.2018.23.4.248.
Anatomical Direct Reduction of Bony Mallet Finger Using Modified-Intrafocal Pinning Technique
- Affiliations
-
- 1Department of Orthopaedic Surgery, Chungbuk National University Hospital, Cheongju, Korea. carm0916@hanmail.net
- KMID: 2427390
- DOI: http://doi.org/10.12790/ahm.2018.23.4.248
Abstract
- PURPOSE
The purpose of this study was to evaluate the clinical results of anatomic reduction of bony mallet finger using modified-intrafocal pinning technique.
METHODS
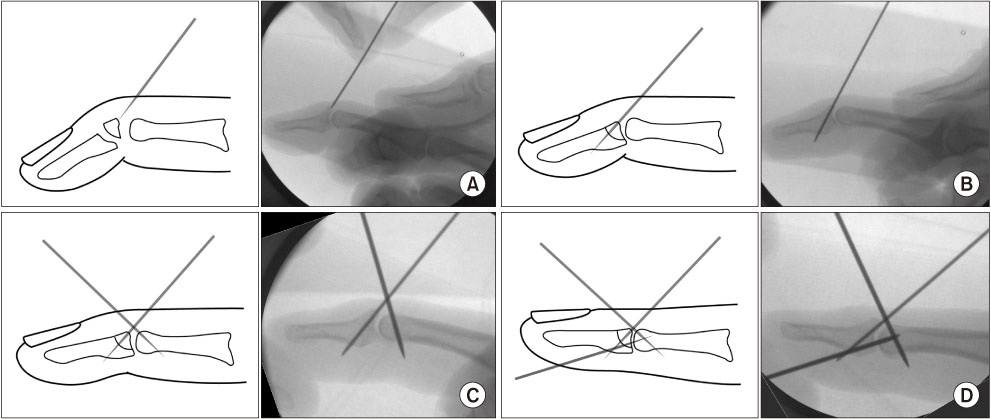
From March 2014 to October 2017, 18 patients with bony mallet finger were treated with modified-intrafocal pinning technique. Kirschner-wire was used to directly reduction the bony fragment, and extension block pinning and distal interphalangeal joint fixation were additionally performed to minimize the loss of reduction. Postoperative pain, range of motion, and radiological evaluation were performed. Duration of bone healing, functional recovery and complication rate were evaluated and Crawford's criteria was used to determine functional outcome after surgery.
RESULTS
Bone union was achieved in all cases after a postoperative mean of 6 weeks (5-7 weeks). An average of 2.8° (0°-10°) extension loss occurred in all patients. All patients showed satisfactory joint congruency and reformation of the joint surface, the mean flexion angle of the distal interphalangeal joint at the final follow-up was 72.2° (70°-75°). According to Crawford's classification, 12 patients (66.7%) were excellent and 6 patients (33.3%) were good.
CONCLUSION
Modified-intrafocal pinning technique is a method of obtaining anatomical bone healing by directly reduction and fixation of the bony fragment. Combined with other conventional percutaneous pinning procedures, it is expected that good results can be obtained if applied to appropriate indications.
MeSH Terms
Figure
Reference
-
1. Salazar Botero S, Hidalgo Diaz JJ, Benaïda A, Collon S, Facca S, Liverneaux PA. Review of acute traumatic closed mallet finger injuries in adults. Arch Plast Surg. 2016; 43:134–144.
Article2. Wehbé MA, Schneider LH. Mallet fractures. J Bone Joint Surg Am. 1984; 66:658–669.
Article3. Stark HH, Gainor BJ, Ashworth CR, Zemel NP, Rickard TA. Operative treatment of intra-articular fractures of the dorsal aspect of the distal phalanx of digits. J Bone Joint Surg Am. 1987; 69:892–896.
Article4. Ishiguro T, Itoh Y, Yabe Y, Hashizume N. Extension block with Kirschner wire for fracture dislocation of the distal interphalangeal joint. Tech Hand Up Extrem Surg. 1997; 1:95–102.
Article5. Chung DW, Lee JH. Anatomic reduction of mallet fractures using extension block and additional intrafocal pinning techniques. Clin Orthop Surg. 2012; 4:72–76.
Article6. Crawford GP. The molded polythene splint for mallet finger deformities. J Hand Surg Am. 1984; 9:231–237.
Article7. Garberman SF, Diao E, Peimer CA. Mallet finger: results of early versus delayed closed treatment. J Hand Surg Am. 1994; 19:850–852.
Article8. McFarlane RM, Hampole MK. Treatment of extensor tendon injuries of the hand. Can J Surg. 1973; 16:366–375.9. Warren RA, Norris SH, Ferguson DG. Mallet finger: a trial of two splints. J Hand Surg Br. 1988; 13:151–153.
Article10. Bendre AA, Hartigan BJ, Kalainov DM. Mallet finger. J Am Acad Orthop Surg. 2005; 13:336–344.
Article11. Shimura H, Wakabayashi Y, Nimura A. A novel closed reduction with extension block and flexion block using Kirschner wires and microscrew fixation for mallet fractures. J Orthop Sci. 2014; 19:308–312.
Article12. Toker S, Türkmen F, Pekince O, Korucu I, Karalezli N. Extension block pinning versus hook plate fixation for treatment of mallet fractures. J Hand Surg Am. 2015; 40:1591–1596.
Article13. Handoll HH, Vaghela MV. Interventions for treating mallet finger injuries. Cochrane Database Syst Rev. 2004; (3):CD004574.
Article14. Kim JY, Lee SH. Factors related to distal interphalangeal joint extension loss after extension block pinning of mallet finger fractures. J Hand Surg Am. 2016; 41:414–419.
Article15. Hofmeister EP, Mazurek MT, Shin AY, Bishop AT. Extension block pinning for large mallet fractures. J Hand Surg Am. 2003; 28:453–459.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anatomic Reduction of Mallet Fractures Using Extension Block and Additional Intrafocal Pinning Techniques
- Current concepts in traumatic mallet finger management
- Tension Wire Fixation of bony Mallet Finger
- The Result of the Modified Extension Block Technique in Bony Mallet Finger
- Evaluation of Fragment Reduction Feasibility When Treating Bony Mallet Finger Using Extension Block K-Wire Technique