Arch Hand Microsurg.
2018 Dec;23(4):223-229. 10.12790/ahm.2018.23.4.223.
Outcome of Suture Suspension Arthroplasty for Thumb Carpometacarpal Joint Arthritis
- Affiliations
-
- 1Department of Orthopaedic Surgery, Seoul National University College of Medicine, Seoul, Korea. hsgong@snu.ac.kr
- KMID: 2427387
- DOI: http://doi.org/10.12790/ahm.2018.23.4.223
Abstract
- PURPOSE
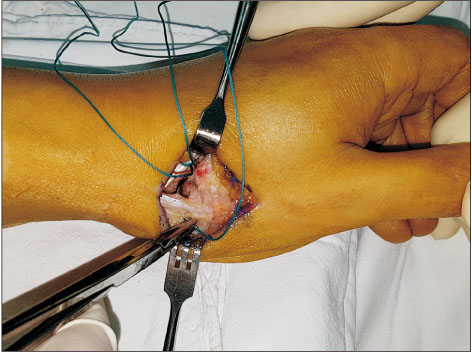
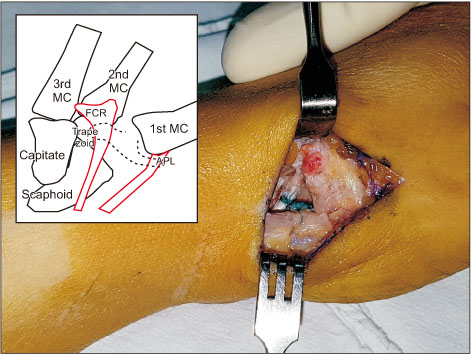
A number of procedures were introduced to stabilize the 1st metacarpal bone after resection of the trapezium in the thumb carpometacarpal joint (CMCJ) arthroplasty. However, some surgical procedures may inevitably damage normal structures, such as harvesting tendons or drilling of a bone for tendon passage. Suture suspension arthroplasty is relatively less invasive and easier to perform than the previously described surgical methods. The purpose of this study was to report the therapeutic efficiency of the suture suspension arthroplasty.
METHODS
We retrospectively reviewed 12 patients who underwent suture suspension arthroplasty for the treatment of thumb CMCJ arthritis. Pain visual analogue scale (VAS), satisfaction about surgical outcomes, and the disabilities of the arm, shoulder and hand (DASH) scores were measured to evaluate the functional outcomes and the Trapezial Space Ratios were measured. Satisfaction was measured in the range of "very dissatisfied" (0) to "very satisfied" (10).
RESULTS
The mean follow-up period was 23 months. Pain VAS score improved significantly from 7.0 to 2.9 (p < 0.05). And mean satisfaction scale was 6.9. However, there was no significant difference in DASH scores between before and after surgery (p=0.06). The mean trapezial space ratio was calculated to be 0.45 before surgery, 0.33 immediately after surgery, 0.23 at the last follow-up.
CONCLUSION
Suture suspension arthroplasty is a satisfactory surgical procedure. And compared with other procedures, there is no significant difference in the reduction of the trapezial space. It may be useful in advanced thumb CMCJ arthritis.
MeSH Terms
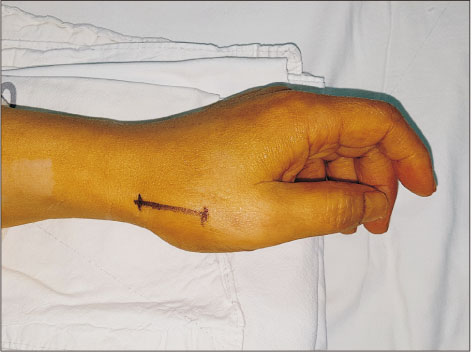
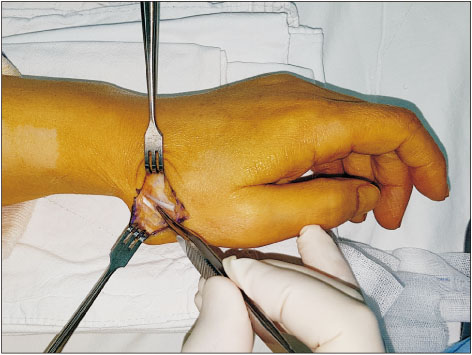
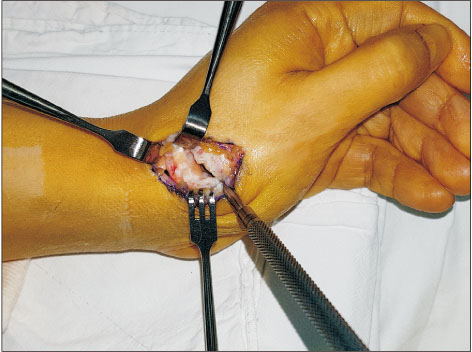
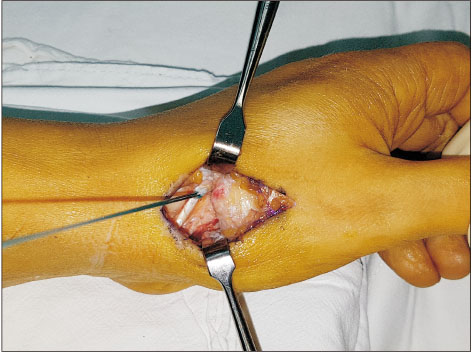
Figure
Reference
-
1. Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in postmenopausal women. J Hand Surg Br. 1994; 19:340–341.
Article2. Sodha S, Ring D, Zurakowski D, Jupiter JB. Prevalence of osteoarthrosis of the trapeziometacarpal joint. J Bone Joint Surg Am. 2005; 87:2614–2618.
Article3. Stevens-Lapsley JE, Kohrt WM. Osteoarthritis in women: effects of estrogen, obesity and physical activity. Womens Health (Lond). 2010; 6:601–615.
Article4. Wolf JM, Delaronde S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of US hand surgeons. J Hand Surg Am. 2012; 37:77–82.
Article5. Berger AJ, Meals RA. Management of osteoarthrosis of the thumb joints. J Hand Surg Am. 2015; 40:843–850.
Article6. Davis TR, Brady O, Barton NJ, Lunn PG, Burke FD. Trapeziectomy alone, with tendon interposition or with ligament reconstruction? J Hand Surg Br. 1997; 22:689–694.
Article7. Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011; 36:157–169.
Article8. Putnam MD, Meyer NJ, Baker D, Brehmer J, Carlson BD. Trapezium excision and suture suspensionplasty (TESS) for the treatment of thumb carpometacarpal arthritis. Tech Hand Up Extrem Surg. 2014; 18:102–108.
Article9. Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973; 55:1655–1666.
Article10. Kadiyala RK, Gelberman RH, Kwon B. Radiographic assessment of the trapezial space before and after ligament reconstruction and tendon interposition arthroplasty. J Hand Surg Br. 1996; 21:177–181.11. Kuhns CA, Meals RA. Hematoma and distraction arthroplasty for basal thumb osteoarthritis. Tech Hand Up Extrem Surg. 2004; 8:2–6.
Article12. Gray KV, Meals RA. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am. 2007; 32:23–29.
Article13. Bernstein RA. Arthritis of the thumb and digits: current concepts. Instr Course Lect. 2015; 64:281–294.14. DelSignore JL, Accardi KZ. Suture suspension arthroplasty technique for basal joint arthritis reconstruction. Tech Hand Up Extrem Surg. 2009; 13:166–172.
Article15. Yao J, Cheah AE. Mean 5-year follow-up for suture button suspensionplasty in the treatment of thumb carpometacarpal joint osteoarthritis. J Hand Surg Am. 2017; 42:569.e1–569.e11.
Article16. Downing ND, Davis TR. Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am. 2001; 26:862–868.
Article17. Iyer KM. The results of excision of the trapezium. Hand. 1981; 13:246–250.
Article18. Anwar R, Cohen A, Nicholl JE. The gap after trapeziectomy: a prospective study. J Hand Surg Br. 2006; 31:566–568.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fourth and Fifth Metacarpal Base Arthrodesis for Posttraumatic Arthritis of Fifth Carpometacarpal Joint
- Arthroplasty for Neglected Dislocation of the Carpometacarpal Joint of the Thumb: A Case Report
- Chronic Instability of the Carpometacarpal Joint of the Thumb after Trauma: A Report of 3 Cases
- Bilateral Carpometacarpal Joint Dislocations of the Thumb
- Surgical Outcomes of Suspension Arthroplasty with Dermal Allograft Interposition after Trapeziectomy: Comparison with Ligament Reconstruction and Interposition Using the Flexor Carpi Radialis Tendon