Korean J Radiol.
2017 ;18(4):632-642. 10.3348/kjr.2017.18.4.632.
Estimation of Diastolic Filling Pressure with Cardiac CT in Comparison with Echocardiography Using Tissue Doppler Imaging: Determination of Optimal CT Reconstruction Parameters
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital Bucheon, Bucheon 14584, Korea. acarad@naver.com
- 2Department of Biostatistics, Soonchunhyang University College of Medicine, Seoul 04401, Korea.
- 3Terarecon Korea, Seoul 04919, Korea.
- 4Department of Radiology, Soonchunhyang University Hospital Cheonan, Cheonan 31151, Korea.
- 5Department of Radiology, Soonchunhyang University Hospital Seoul, Seoul 04401, Korea.
- 6Department of Cardiology, Soonchunhyang University Hospital Bucheon, Bucheon 14584, Korea.
- KMID: 2427232
- DOI: http://doi.org/10.3348/kjr.2017.18.4.632
Abstract
OBJECTIVE
To determine the optimal CT image reconstruction parameters for the measurement of early transmitral peak velocity (E), early peak mitral septal tissue velocity (E"²), and E / E"².
MATERIALS AND METHODS
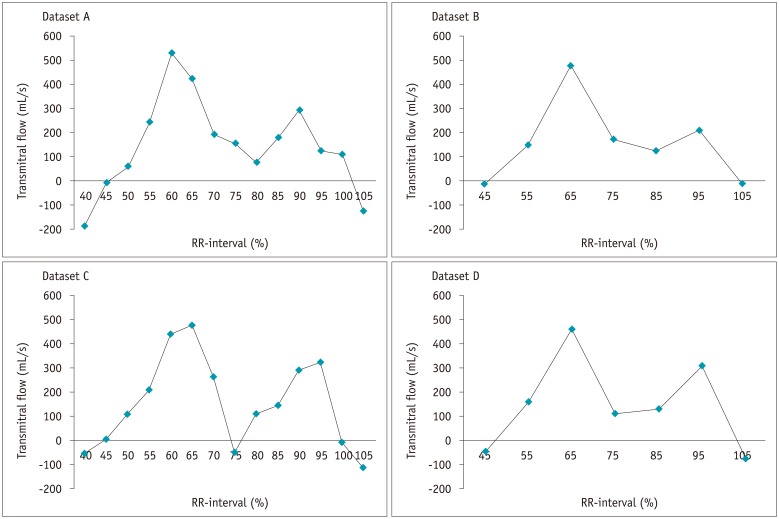
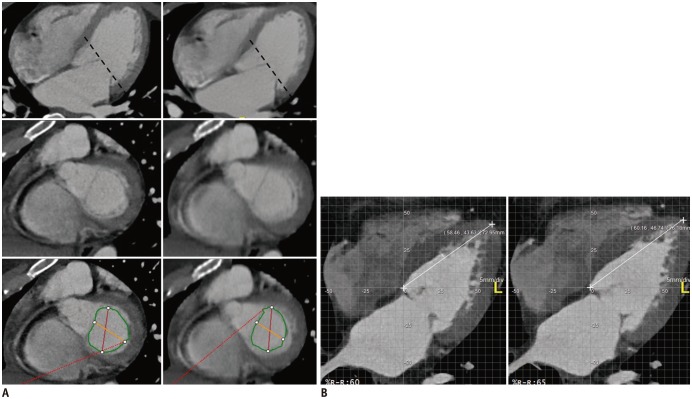
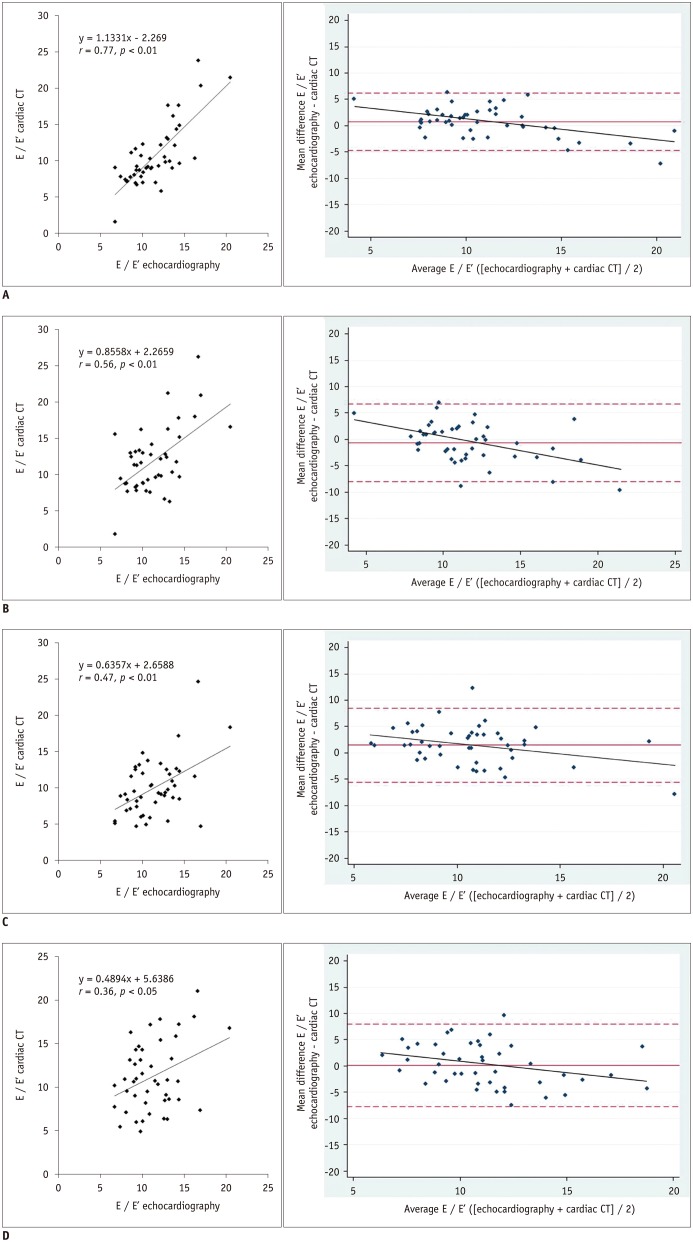
Forty-six patients underwent simultaneous cardiac CT and echocardiography on the same day. Four CT datasets were reconstructed with a slice thickness/interval of 0.9/0.9 mm or 3/3 mm at 10 (10% RR-interval) or 20 (5% RR-interval) RR-intervals. The E was calculated by dividing the peak transmitral flow (mL/s) by the corresponding mitral valve area (cm²). E"² was calculated from the changes in the left ventricular length per cardiac phase. E / E"² was then estimated and compared with that from echocardiography.
RESULTS
For assessment of E / E"², CT and echocardiography were more strongly correlated (p < 0.05) with a slice thickness of 0.9 mm and 5% RR-interval (r = 0.77) than with 3 mm or 10% RR-interval. The diagnostic accuracy of predicting elevated filling pressure (E / E"²â‰¥ 13, n = 14) was better with a slice thickness of 0.9 mm and 5% RR-interval (87.0%) than with 0.9 mm and 10% RR-interval (71.7%) (p = 0.123) and significantly higher than that with a slice thickness of 3 mm with 5% (67.4%) and 10% RR-interval (63.0%), (p < 0.05), respectively.
CONCLUSION
Data reconstruction with a slice thickness of 0.9 mm at 5% RR-interval is superior to that with a slice thickness of 3 mm or 10% RR-interval in terms of the correlation of E / E"² between CT and echocardiography. Thin slices and frequent sampling also allow for more accurate prediction of elevated filling pressure.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Age of Data in Contemporary Research Articles Published in Representative General Radiology Journals
Ji Hun Kang, Dong Hwan Kim, Seong Ho Park, Jung Hwan Baek
Korean J Radiol. 2018;19(6):1172-1178. doi: 10.3348/kjr.2018.19.6.1172.Reliability in Using Routine Coronary CT Angiography with Retrospective Electrocardiographic Gating for the Comprehensive Functional Evaluation of the Left Ventricle
Eun-Ju Kang, Jihoon Hong, Jongmin Park, Jongmin Lee
J Korean Soc Radiol. 2019;80(1):69-80. doi: 10.3348/jksr.2019.80.1.69.
Reference
-
1. Gaasch WH, Little WC. Assessment of left ventricular diastolic function and recognition of diastolic heart failure. Circulation. 2007; 116:591–593. PMID: 17679627.
Article2. Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–259. PMID: 16855265.
Article3. Bhuiyan T, Maurer MS. Heart failure with preserved ejection fraction: persistent diagnosis, therapeutic enigma. Curr Cardiovasc Risk Rep. 2011; 5:440–449. PMID: 22081782.
Article4. Paulus WJ, Tschöpe C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers FE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J. 2007; 28:2539–2550. PMID: 17428822.5. Meta-Analysis Research Group in Echocardiography (MeRGE) AMI Collaborators. Møller JE, Whalley GA, Dini FL, Doughty RN, Gamble GD, et al. Independent prognostic importance of a restrictive left ventricular filling pattern after myocardial infarction: an individual patient meta-analysis: meta-analysis research group in echocardiography acute myocardial infarction. Circulation. 2008; 117:2591–2598. PMID: 18474816.6. Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, et al. Clinical utility of Doppler echocardiography and tissue doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation. 2000; 102:1788–1794. PMID: 11023933.7. Yamamoto K, Nishimura RA, Chaliki HP, Appleton CP, Holmes DR Jr, Redfield MM. Determination of left ventricular filling pressure by Doppler echocardiography in patients with coronary artery disease: critical role of left ventricular systolic function. J Am Coll Cardiol. 1997; 30:1819–1826. PMID: 9385913.
Article8. Hamon M, Biondi-Zoccai GG, Malagutti P, Agostoni P, Morello R, Valgimigli M, et al. Diagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: a meta-analysis. J Am Coll Cardiol. 2006; 48:1896–1910. PMID: 17084268.9. Asferg C, Usinger L, Kristensen TS, Abdulla J. Accuracy of multi-slice computed tomography for measurement of left ventricular ejection fraction compared with cardiac magnetic resonance imaging and two-dimensional transthoracic echocardiography: a systematic review and meta-analysis. Eur J Radiol. 2012; 81:e757–e762. PMID: 22381439.10. Dewey M, Müller M, Eddicks S, Schnapauff D, Teige F, Rutsch W, et al. Evaluation of global and regional left ventricular function with 16-slice computed tomography, biplane cineventriculography, and two-dimensional transthoracic echocardiography: comparison with magnetic resonance imaging. J Am Coll Cardiol. 2006; 48:2034–2044. PMID: 17112993.11. Henneman MM, Bax JJ, Schuijf JD, Jukema JW, Holman ER, Stokkel MP, et al. Global and regional left ventricular function: a comparison between gated SPECT, 2D echocardiography and multi-slice computed tomography. Eur J Nucl Med Mol Imaging. 2006; 33:1452–1460. PMID: 16865394.
Article12. Arraiza M, Azcárate PM, Arias J, de Cecco CN, Pueyo JC, Rábago G, et al. Accuracy of different reconstruction intervals to quantify left ventricular function and mass in cardiac computed tomography examinations. Radiologia. 2012; 54:432–441. PMID: 21920566.
Article13. Butler J, Shapiro MD, Jassal DS, Neilan TG, Nichols J, Ferencik M, et al. Comparison of multidetector computed tomography and two-dimensional transthoracic echocardiography for left ventricular assessment in patients with heart failure. Am J Cardiol. 2007; 99:247–249. PMID: 17223427.
Article14. Maffei E, Messalli G, Martini C, Nieman K, Catalano O, Rossi A, et al. Left and right ventricle assessment with cardiac CT: validation study vs. cardiac MR. Eur Radiol. 2012; 22:1041–1049. PMID: 22270140.
Article15. Vural M, Uçar O, Selvi NA, Paşaoğlu L, Gürbüz MO, Ciçekçiogğlu H, et al. Assessment of global left ventricular systolic function with multidetector CT and 2D echocardiography: a comparison between reconstructions of 1-mm and 2-mm slice thickness at multidetector CT. Diagn Interv Radiol. 2010; 16:236–240. PMID: 20635319.16. Robb RA, Ritman EL. High speed synchronous volume computed tomography of the heart. Radiology. 1979; 133(3 Pt 1):655–661. PMID: 504645.
Article17. Nakahara T, Jinzaki M, Fukuda N, Takahashi Y, Ishihara T, Takada A, et al. Estimation of the left ventricular diastolic function with cardiac MDCT: correlation of the slope of the time-enhancement-curve with the mitral annulus diastolic velocity. Eur J Radiol. 2012; 81:234–238. PMID: 21239129.
Article18. Boogers MJ, van Werkhoven JM, Schuijf JD, Delgado V, El-Naggar HM, Boersma E, et al. Feasibility of diastolic function assessment with cardiac CT: feasibility study in comparison with tissue Doppler imaging. JACC Cardiovasc Imaging. 2011; 4:246–256. PMID: 21414572.19. Lee H, Kim SY, Gebregziabher M, Hanna EL, Schoepf UJ. Impact of ventricular contrast medium attenuation on the accuracy of left and right ventricular function analysis at cardiac multi detector-row CT compared with cardiac MRI. Acad Radiol. 2012; 19:395–405. PMID: 22225726.
Article20. Lim S, Lee H, Lee SJ, Kim JK, Suh J, Lee EH, et al. CT signs of right ventricular dysfunction correlated with echocardiography-derived pulmonary arterial systolic pressure: incremental value of the pulmonary arterial diameter index. Int J Cardiovasc Imaging. 2013; 29(Suppl 2):109–118. PMID: 24194372.
Article21. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165–193.
Article22. Arques S, Roux E, Luccioni R. Current clinical applications of spectral tissue Doppler echocardiography (E/E′ ratio) as a noninvasive surrogate for left ventricular diastolic pressures in the diagnosis of heart failure with preserved left ventricular systolic function. Cardiovasc Ultrasound. 2007; 5:16. PMID: 17386087.
Article23. Evans JD. Straightforward statistics for the behavioral sciences. Pacific Grove: Brooks/Cole Publishing;1996.24. Alkadhi H, Wildermuth S, Bettex DA, Plass A, Baumert B, Leschka S, et al. Mitral regurgitation: quantification with 16-detector row CT--initial experience. Radiology. 2006; 238:454–463. PMID: 16371578.
Article25. Delgado V, Tops LF, Schuijf JD, de Roos A, Brugada J, Schalij MJ, et al. Assessment of mitral valve anatomy and geometry with multislice computed tomography. JACC Cardiovasc Imaging. 2009; 2:556–565. PMID: 19442940.
Article26. Kim YJ, Yong HS, Kim SM, Kim JA, Yang DH, Hong YJ. Korean guidelines for the appropriate use of cardiac CT. Korean J Radiol. 2015; 16:251–285. PMID: 25741189.
Article27. Arques S, Roux E, Sbragia P, Pieri B, Gelisse R, Ambrosi P, et al. Accuracy of tissue Doppler echocardiography in the diagnosis of new-onset congestive heart failure in patients with levels of B-type natriuretic peptide in the midrange and normal left ventricular ejection fraction. Echocardiography. 2006; 23:627–634. PMID: 16970713.
Article28. Huang CH, Tsai MS, Hsieh CC, Wang TD, Chang WT, Chen WJ. Diagnostic accuracy of tissue Doppler echocardiography for patients with acute heart failure. Heart. 2006; 92:1790–1794. PMID: 16803936.
Article29. Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure--abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med. 2004; 350:1953–1959. PMID: 15128895.
Article30. Mo YH, Jaw FS, Wang YC, Jeng CM, Peng SF. Effects of propranolol on the left ventricular volume of normal subjects during CT coronary angiography. Korean J Radiol. 2011; 12:319–326. PMID: 21603291.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use and Limitations of E/e' to Assess Left Ventricular Filling Pressure by Echocardiography
- Reconstruction of the Transmitral Flow Rate Curve with M-Mode,2-Dimensional and Doppler Echocardiography -Validation Study-
- Doppler Flow Patterns of Constrictive Pericarditis
- Evaluation of the Left Atrial Size and Function in Addition to Analysis of the Mitral and Pulmonary Venous Flow Velocity in the Estimation of Left Ventricular Filling Pressures
- Usefulness of Pressure Half Time by Pulse Doppler Ultrasound in Evaluation of the Severity of Mitral Stenosis