Yonsei Med J.
2016 Nov;57(6):1500-1507. 10.3349/ymj.2016.57.6.1500.
Clinical Signs and Subjective Symptoms of Temporomandibular Disorders in Instrumentalists
- Affiliations
-
- 1Department of Orofacial Pain & Oral Medicine, Yonsei University College of Dentistry, Seoul, Korea. k8756050@yuhs.ac
- 2School of Medicine, University of California-Irvine, Irvine, CA, USA.
- 3Division in Anatomy and Developmental Biology, Department of Oral Biology, Human Identification Research Center, Yonsei University College of Dentistry, Seoul, Korea.
- KMID: 2427171
- DOI: http://doi.org/10.3349/ymj.2016.57.6.1500
Abstract
- PURPOSE
Most of the reports on instrumentalists' experiences of temporomandibular disorders (TMD) have been reported not by clinical examinations but by subjective questionnaires. The aim of this study was to investigate the clinical signs and subjective symptoms of TMD in a large number of instrumentalists objectively.
MATERIALS AND METHODS
A total of 739 musicians from a diverse range of instrument groups completed a TMD questionnaire. Among those who reported at least one symptom of TMD, 71 volunteers underwent clinical examinations and radiography for diag-nosis.
RESULTS
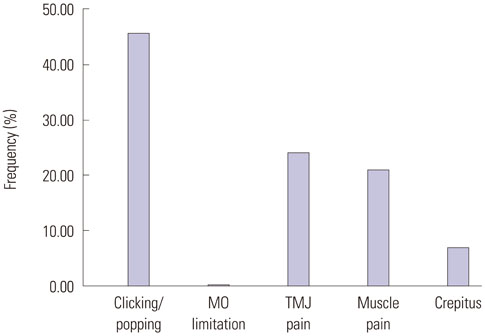
Overall, 453 participants (61.3%) reported having one or more symptoms of TMD. The most frequently reported symptom was a clicking or popping sound, followed by temporomandibular joint (TMJ) pain, muscle pain, crepitus, and mouth opening limitations. Compared with lower-string instrumentalists, a clicking or popping sound was about 1.8 and 2 times more frequent in woodwind and brass instrumentalists, respectively. TMJ pain was about 3.2, 2.8, and 3.2 times more frequent in upper-string, woodwind, and brass instrumentalists, respectively. Muscle pain was about 1.5 times more frequent in instrumentalists with an elevated arm position than in those with a neutral arm position. The most frequent diagnosis was myalgia or myofascial pain (MFP), followed by disc displacement with reduction. Myalgia or MFP was 4.6 times more frequent in those practicing for no less than 3.5 hours daily than in those practicing for less than 3.5 hours.
CONCLUSION
The results indicate that playing instruments can play a contributory role in the development of TMD.
Keyword
MeSH Terms
-
Adult
Facial Pain/etiology
Female
Humans
Magnetic Resonance Imaging/methods
Male
*Music
Occupational Diseases/*etiology/physiopathology
Physical Examination
Range of Motion, Articular/*physiology
Sound/*adverse effects
Temporomandibular Joint/*physiopathology
Temporomandibular Joint Disorders/*diagnosis/etiology/physiopathology
Figure
Reference
-
1. Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008; 72:930–947.
Article2. Leeuw Rd. Orofacial pain: guidelines for assessment, diagnosis, and management. 4th ed. Chicago, London: Quintessence Books;2008.3. Goulet JP, Lavigne GJ, Lund JP. Jaw pain prevalence among French-speaking Canadians in Québec and related symptoms of temporomandibular disorders. J Dent Res. 1995; 74:1738–1744.
Article4. Pow EH, Leung KC, McMillan AS. Prevalence of symptoms associated with temporomandibular disorders in Hong Kong Chinese. J Orofac Pain. 2001; 15:228–234.5. Nekora-Azak A, Evlioglu G, Ordulu M, Is¸sever H. Prevalence of symptoms associated with temporomandibular disorders in a Turkish population. J Oral Rehabil. 2006; 33:81–84.
Article6. GonÇalves DA, Dal Fabbro AL, Campos JA, Bigal ME, Speciali JG. Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain. 2010; 24:270–278.7. Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005; 9:613–633.
Article8. Winocur E, Gavish A, Finkelshtein T, Halachmi M, Gazit E. Oral habits among adolescent girls and their association with symptoms of temporomandibular disorders. J Oral Rehabil. 2001; 28:624–629.
Article9. Karibe H, Goddard G, Gear RW. Sex differences in masticatory muscle pain after chewing. J Dent Res. 2003; 82:112–116.
Article10. Miyake R, Ohkubo R, Takehara J, Morita M. Oral parafunctions and association with symptoms of temporomandibular disorders in Japanese university students. J Oral Rehabil. 2004; 31:518–523.
Article11. Rossetti LM, Pereira de Araujo Cdos R, Rossetti PH, Conti PC. Association between rhythmic masticatory muscle activity during sleep and masticatory myofascial pain: a polysomnographic study. J Orofac Pain. 2008; 22:190–200.12. Foxman I, Burgel BJ. Musician health and safety: preventing playing-related musculoskeletal disorders. AAOHN J. 2006; 54:309–316.13. Głowacka A, Matthews-Kozanecka M, Kawala M, Kawala B. The impact of the long-term playing of musical instruments on the stomatognathic system - review. Adv Clin Exp Med. 2014; 23:143–146.
Article14. Steinmetz A, Zeh A, Delank KS, Peroz I. Symptoms of craniomandibular dysfunction in professional orchestra musicians. Occup Med (Lond). 2014; 64:17–22.
Article15. Heikkilä J, Hamberg L, Meurman JH. Temporomandibular disorders: symptoms and facial pain in orchestra musicians in Finland. Music Med. 2012; 4:171–176.
Article16. Zuskin E, Schachter EN, Kolcić I, Polasek O, Mustajbegović J, Arumugam U. Health problems in musicians--a review. Acta Dermatovenerol Croat. 2005; 13:247–251.17. Attallah MM, Visscher CM, van Selms MK, Lobbezoo F. Is there an association between temporomandibular disorders and playing a musical instrument? A review of literature. J Oral Rehabil. 2014; 41:532–541.
Article18. Hirsch JA, McCall WD Jr, Bishop B. Jaw dysfunction in viola and violin players. J Am Dent Assoc. 1982; 104:838–843.
Article19. Kovero O, Könönen M. Signs and symptoms of temporomandibular disorders and radiologically observed abnormalities in the condyles of the temporomandibular joints of professional violin and viola players. Acta Odontol Scand. 1995; 53:81–84.
Article20. Rodríguez-Lozano FJ, Sáez-Yuguero MR, Bermejo-Fenoll A. Prevalence of temporomandibular disorder-related findings in violinists compared with control subjects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e15–e19.
Article21. Gualtieri PA. May Johnny or Janie play the clarinet? The Eastman Study: a report on the orthodontic evaluations of college-level and professional musicians who play brass and woodwind instruments. Am J Orthod. 1979; 76:260–276.22. Prensky HD, Shapiro GI, Silverman SI. Dental diagnosis and treatment for musicians. Spec Care Dentist. 1986; 6:198–202.
Article23. Howard JA, Lovrovich AT. Wind instruments: their interplay with orofacial structures. Med Probl Perform Art. 1989; 4:59–72.24. Sayegh Ghoussoub M, Ghoussoub K, Chaaya A, Sleilaty G, Joubrel I, Rifaï K. [Orofacial and hearing specific problems among 340 wind instrumentalists in Lebanon]. J Med Liban. 2008; 56:159–167.25. Nyman T, Wiktorin C, Mulder M, Johansson YL. Work postures and neck-shoulder pain among orchestra musicians. Am J Ind Med. 2007; 50:370–376.
Article26. LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997; 8:291–305.
Article27. Taddey JJ. Musicians and temporomandibular disorders: prevalence and occupational etiologic considerations. Cranio. 1992; 10:241–244.
Article28. Kovero O, Könönen M. Signs and symptoms of temporomandibular disorders in adolescent violin players. Acta Odontol Scand. 1996; 54:271–274.
Article29. Steinmetz A, Ridder PH, Methfessel G, Muche B. Professional musicians with craniomandibular dysfunctions treated with oral splints. Cranio. 2009; 27:221–230.
Article30. Herman E. Orthodontic aspects of musical instrument selection. Am J Orthod. 1974; 65:519–530.
Article31. Okner M, Kernozek T. Chinrest pressure in violin playing: type of music, chin rest, and shoulder pad as possible mediators. Clin Biomech (Bristol, Avon). 1997; 12:S12–S13.
Article32. Steinmetz A, Ridder PH, Reichelt A. Craniomandibular dysfunction and violin playing: prevalence and the influence of oral splints on head and neck muscles in violinists. Med Probl Perform Art. 2006; 21:183–189.
Article33. Kovero O. Degenerative temporomandibular joint disease in a young violinist. Dentomaxillofac Radiol. 1989; 18:133–135.
Article34. Kovero O, Könönen M, Pirinen S. The effect of professional violin and viola playing on the bony facial structures. Eur J Orthod. 1997; 19:39–45.
Article35. Kovero O, Könönen M, Pirinen S. The effect of violin playing on the bony facial structures in adolescents. Eur J Orthod. 1997; 19:369–375.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The prevalence of temporomandibular disorders in 16~18 aged subjects at Yongin, Kyungkido, Korea
- Considerations in the Diagnosis and Treatment of Temporomandibular Disorders in Children and Adolescents: A Review
- A comparison of clinical symptoms and magnetic resonance images in temporomandibular joint disorders
- Effectiveness of Temporomandibular Joint Disorder Follow-Up Using Bone Scans
- Effect on explanation of pathogenesis and stress management as primary care of tmj disorder