Yonsei Med J.
2016 Nov;57(6):1488-1493. 10.3349/ymj.2016.57.6.1488.
A Comparison of Cough Assistance Techniques in Patients with Respiratory Muscle Weakness
- Affiliations
-
- 1Department of Rehabilitation Medicine, Incheon Workers' Compensation Hospital, Incheon, Korea.
- 2Department of Medicine, The Graduate School of Yonsei University, Seoul, Korea.
- 3Department of Rehabilitation Medicine, Gangnam Severance Hospital, Rehabilitation Institute of Neuromuscular Disease, Yonsei University College of Medicine, Seoul, Korea. kswoong@yuhs.ac
- 4Department of Physical Medicine and Rehabilitation, Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Jeonju, Korea.
- KMID: 2427169
- DOI: http://doi.org/10.3349/ymj.2016.57.6.1488
Abstract
- PURPOSE
To assess the ability of a mechanical in-exsufflator (MI-E), either alone or in combination with manual thrust, to augment cough in patients with neuromuscular disease (NMD) and respiratory muscle dysfunction.
MATERIALS AND METHODS
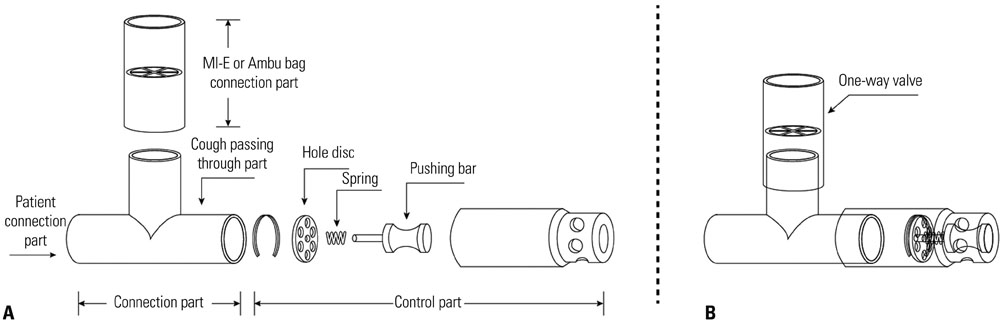
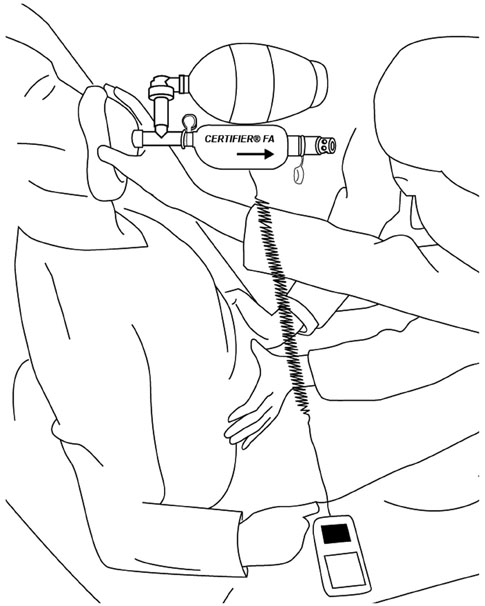
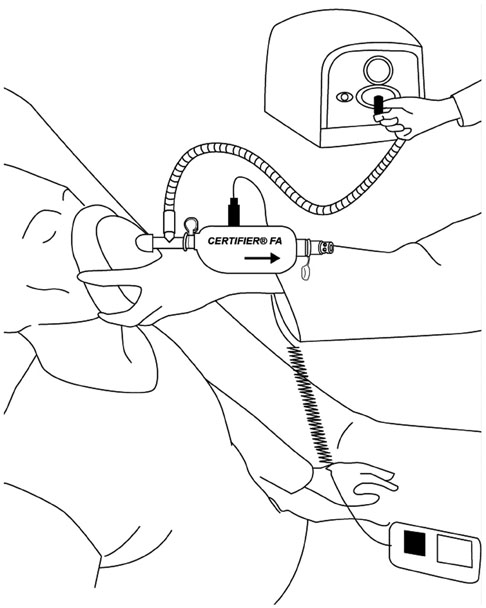
For this randomized crossover single-center controlled trial, patients with noninvasive ventilator-dependent NMD were recruited. The primary outcome was peak cough flow (PCF), which was measured in each patient after a cough that was unassisted, manually assisted following a maximum insufflation capacity (MIC) maneuver, assisted by MI-E, or assisted by manual thrust plus MI-E. The cough augmentation techniques were provided in random order. PCF was measured using a new device, the Cough Aid.
RESULTS
All 40 enrolled participants (37 males, three females; average age, 20.9±7.2 years) completed the study. The mean (standard deviation) PCFs in the unassisted, manually assisted following an MIC maneuver, MI-E-assisted, and manual thrust plus MI-E-assisted conditions were 95.7 (40.5), 155.9 (53.1), 177.2 (33.9), and 202.4 (46.6) L/min, respectively. All three interventions significantly improved PCF. However, manual assistance following an MIC maneuver was significantly less effective than MI-E alone. Manual thrust plus MI-E was significantly more effective than both of these interventions.
CONCLUSION
In patients with NMD and respiratory muscle dysfunction, MI-E alone was more effective than manual assistance following an MIC maneuver. However, MI-E used in conjunction with manual thrust improved PCF even further.
MeSH Terms
-
Adolescent
Adult
Aged
*Cough
Cross-Over Studies
Female
Humans
Insufflation/*instrumentation/methods/statistics & numerical data
Male
Middle Aged
Neuromuscular Diseases/*physiopathology
Peak Expiratory Flow Rate/physiology
Pressure
Respiratory Function Tests/instrumentation/methods
Respiratory Muscles/*physiopathology
Respiratory Therapy/*methods
Treatment Outcome
Vital Capacity/physiology
Figure
Reference
-
1. Kang SW, Kang YS, Moon JH, Yoo TW. Assisted cough and pulmonary compliance in patients with Duchenne muscular dystrophy. Yonsei Med J. 2005; 46:233–238.
Article2. Finder JD. Airway clearance modalities in neuromuscular disease. Paediatr Respir Rev. 2010; 11:31–34.
Article3. Homnick DN. Mechanical insufflation-exsufflation for airway mucus clearance. Respir Care. 2007; 52:1296–1305.4. Bach JR. Mechanical insufflation-exsufflation. Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest. 1993; 104:1553–1562.5. Morrow B, Zampoli M, van Aswegen H, Argent A. Mechanical insufflation-exsufflation for people with neuromuscular disorders. Cochrane Database Syst Rev. 2013; (12):CD010044.
Article6. Senent C, Golmard JL, Salachas F, Chiner E, Morelot-Panzini C, Meninger V, et al. A comparison of assisted cough techniques in stable patients with severe respiratory insufficiency due to amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2011; 12:26–32.
Article7. Lacombe M, Del Amo Castrillo L, Boré A, Chapeau D, Horvat E, Vaugier I, et al. Comparison of three cough-augmentation techniques in neuromuscular patients: mechanical insufflation combined with manually assisted cough, insufflation-exsufflation alone and insufflation-exsufflation combined with manually assisted cough. Respiration. 2014; 88:215–222.
Article8. Choi WA, Park JH, Kim DH, Kang SW. Cough assistance device for patients with glottis dysfunction and/or tracheostomy. J Rehabil Med. 2012; 44:351–354.
Article9. Park JH, Kang SW, Lee SC, Choi WA, Kim DH. How respiratory muscle strength correlates with cough capacity in patients with respiratory muscle weakness. Yonsei Med J. 2010; 51:392–397.
Article10. Sancho J, Servera E, Marín J, Vergara P, Belda FJ, Bach JR. Effect of lung mechanics on mechanically assisted flows and volumes. Am J Phys Med Rehabil. 2004; 83:698–703.
Article11. Boitano LJ. Management of airway clearance in neuromuscular disease. Respir Care. 2006; 51:913–922.12. Sivasothy P, Brown L, Smith IE, Shneerson JM. Effect of manually assisted cough and mechanical insufflation on cough flow of normal subjects, patients with chronic obstructive pulmonary disease (COPD), and patients with respiratory muscle weakness. Thorax. 2001; 56:438–444.
Article13. Chatwin M, Ross E, Hart N, Nickol AH, Polkey MI, Simonds AK. Cough augmentation with mechanical insufflation/exsufflation in patients with neuromuscular weakness. Eur Respir J. 2003; 21:502–508.
Article14. Mustfa N, Aiello M, Lyall RA, Nikoletou D, Olivieri D, Leigh PN, et al. Cough augmentation in amyotrophic lateral sclerosis. Neurology. 2003; 61:1285–1287.
Article15. Bach JR, Niranjan V, Weaver B. Spinal muscular atrophy type 1: a noninvasive respiratory management approach. Chest. 2000; 117:1100–1105.16. Gómez-Merino E, Sancho J, Marín J, Servera E, Blasco ML, Belda FJ, et al. Mechanical insufflation-exsufflation: pressure, volume, and flow relationships and the adequacy of the manufacturer's guidelines. Am J Phys Med Rehabil. 2002; 81:579–583.17. Tzeng AC, Bach JR. Prevention of pulmonary morbidity for patients with neuromuscular disease. Chest. 2000; 118:1390–1396.
Article18. Miske LJ, Hickey EM, Kolb SM, Weiner DJ, Panitch HB. Use of the mechanical in-exsufflator in pediatric patients with neuromuscular disease and impaired cough. Chest. 2004; 125:1406–1412.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Respiratory Muscle Strength and Cough Capacity in Patients with Duchenne Muscular Dystrophy
- How Respiratory Muscle Strength Correlates with Cough Capacity in Patients with Respiratory Muscle Weakness
- Pulmonary Rehabilitation in Patients with Neuromuscular Disease
- The Relationships of Coughing to the Respiratory Muscle Strength and Pulmonary Compliance in Tetraplegic Patients
- Excitability of the muscle spindle of the steroid induced muscle weakness in the cat