Yonsei Med J.
2017 Mar;58(2):432-438. 10.3349/ymj.2017.58.2.432.
Correlations between Preoperative Angle Parameters and Postoperative Unpredicted Refractive Errors after Cataract Surgery in Open Angle Glaucoma (AOD 500)
- Affiliations
-
- 1Department of Ophthalmology, International St. Mary's Hospital, Catholic Kwandong University College of Medicine, Incheon, Korea.
- 2Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. gjseong@yuhs.ac
- 3Department of Ophthalmology, Eulji University Hospital, Daejeon, Korea.
- KMID: 2427134
- DOI: http://doi.org/10.3349/ymj.2017.58.2.432
Abstract
- PURPOSE
To assess the accuracy of intraocular lens (IOL) power prediction for cataract surgery with open angle glaucoma (OAG) and to identify preoperative angle parameters correlated with postoperative unpredicted refractive errors.
MATERIALS AND METHODS
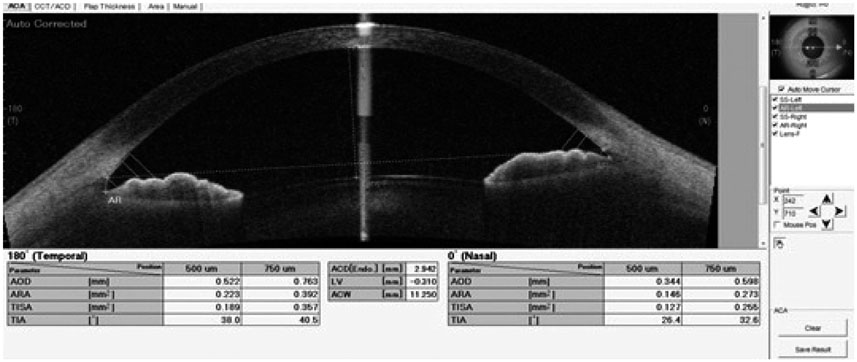
This study comprised 45 eyes from 45 OAG subjects and 63 eyes from 63 non-glaucomatous cataract subjects (controls). We investigated differences in preoperative predicted refractive errors and postoperative refractive errors for each group. Preoperative predicted refractive errors were obtained by biometry (IOL-master) and compared to postoperative refractive errors measured by auto-refractometer 2 months postoperatively. Anterior angle parameters were determined using swept source optical coherence tomography. We investigated correlations between preoperative angle parameters [angle open distance (AOD); trabecular iris surface area (TISA); angle recess area (ARA); trabecular iris angle (TIA)] and postoperative unpredicted refractive errors.
RESULTS
In patients with OAG, significant differences were noted between preoperative predicted and postoperative real refractive errors, with more myopia than predicted. No significant differences were recorded in controls. Angle parameters (AOD, ARA, TISA, and TIA) at the superior and inferior quadrant were significantly correlated with differences between predicted and postoperative refractive errors in OAG patients (-0.321 to -0.408, p<0.05). Superior quadrant AOD 500 was significantly correlated with postoperative refractive differences in multivariate linear regression analysis (β=-2.925, R²=0.404).
CONCLUSION
Clinically unpredicted refractive errors after cataract surgery were more common in OAG than in controls. Certain preoperative angle parameters, especially AOD 500 at the superior quadrant, were significantly correlated with these unpredicted errors.
MeSH Terms
Figure
Reference
-
1. Kronberg BP, Rhee DJ. Anterior segment imaging and the intraocular pressure lowering effect of cataract surgery for open and narrow angle glaucoma. Semin Ophthalmol. 2012; 27:149–154.
Article2. Rim TH, Kim DW, Kim SE, Kim SS. Factors associated with cataract in Korea: a community health survey 2008-2012. Yonsei Med J. 2015; 56:1663–1670.
Article3. Olawoye O, Ashaye A, Bekibele C, Ajuwon AJ. Quality-of-life and visual function after manual small incision cataract surgery in South Western Nigeria. West Afr J Med. 2012; 31:114–119.4. Kang SY, Hong S, Won JB, Seong GJ, Kim CY. Inaccuracy of intraocular lens power prediction for cataract surgery in angle-closure glaucoma. Yonsei Med J. 2009; 50:206–210.
Article5. Dean WH. Quality of small incision cataract surgery. Community Eye Health. 2015; 28:30–31.6. Steinhart MR, Cone-Kimball E, Nguyen C, Nguyen TD, Pease ME, Chakravarti S, et al. Susceptibility to glaucoma damage related to age and connective tissue mutations in mice. Exp Eye Res. 2014; 119:54–60.
Article7. Wang J, Freeman EE, Descovich D, Harasymowycz PJ, Kamdeu Fansi A, Li G, et al. Estimation of ocular rigidity in glaucoma using ocular pulse amplitude and pulsatile choroidal blood flow. Invest Ophthalmol Vis Sci. 2013; 54:1706–1711.
Article8. Yao K, Tang X, Ye P. Corneal astigmatism, high order aberrations, and optical quality after cataract surgery: microincision versus small incision. J Refract Surg. 2006; 22:9 Suppl. S1079–S1082.
Article9. Nutheti R, Shamanna BR, Nirmalan PK, Keeffe JE, Krishnaiah S, Rao GN, et al. Impact of impaired vision and eye disease on quality of life in Andhra Pradesh. Invest Ophthalmol Vis Sci. 2006; 47:4742–4748.
Article10. Contestabile MT, Perdicchi A, Amodeo S, Paffetti L, Iester M, Recupero SM. Effect of refractive correction on the accuracy of frequency-doubling technology Matrix. J Glaucoma. 2013; 22:413–415.
Article11. Fukuda R, Usui T, Tomidokoro A, Mishima K, Matagi N, Miyai T, et al. Noninvasive observations of peripheral angle in eyes after penetrating keratoplasty using anterior segment fourier-domain optical coherence tomography. Cornea. 2012; 31:259–263.
Article12. Zhou AW, Giroux J, Mao AJ, Hutnik CM. Can preoperative anterior chamber angle width predict magnitude of intraocular pressure change after cataract surgery? Can J Ophthalmol. 2010; 45:149–153.
Article13. Guan H, Mick A, Porco T, Dolan BJ. Preoperative factors associated with IOP reduction after cataract surgery. Optom Vis Sci. 2013; 90:179–184.
Article14. Acott TS, Kelley MJ. Extracellular matrix in the trabecular meshwork. Exp Eye Res. 2008; 86:543–561.
Article15. Visse R, Nagase H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res. 2003; 92:827–839.16. De Groef L, Van Hove I, Dekeyster E, Stalmans I, Moons L. MMPs in the trabecular meshwork: promising targets for future glaucoma therapies? Invest Ophthalmol Vis Sci. 2013; 54:7756–7763.
Article17. Fountoulakis N, Labiris G, Aristeidou A, Katsanos A, Tentes I, Kortsaris A, et al. Tissue inhibitor of metalloproteinase 4 in aqueous humor of patients with primary open angle glaucoma, pseudoexfoliation syndrome and pseudoexfoliative glaucoma and its role in proteolysis imbalance. BMC Ophthalmol. 2013; 13:69.
Article18. Nga AD, Yap SL, Samsudin A, Abdul-Rahman PS, Hashim OH, Mimiwati Z. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in the aqueous humour of patients with primary angle closure glaucoma - a quantitative study. BMC Ophthalmol. 2014; 14:33.
Article19. Ashworth Briggs EL, Toh T, Eri R, Hewitt AW, Cook AL. TIMP1, TIMP2, and TIMP4 are increased in aqueous humor from primary open angle glaucoma patients. Mol Vis. 2015; 21:1162–1172.20. Rönkkö S, Rekonen P, Kaarniranta K, Puustjärvi T, Teräsvirta M, Uusitalo H. Matrix metalloproteinases and their inhibitors in the chamber angle of normal eyes and patients with primary open-angle glaucoma and exfoliation glaucoma. Graefes Arch Clin Exp Ophthalmol. 2007; 245:697–704.
Article21. Yamada H, Yoneda M, Gosho M, Kato T, Zako M. Bimatoprost, latanoprost, and tafluprost induce differential expression of matrix metalloproteinases and tissue inhibitor of metalloproteinases. BMC Ophthalmol. 2016; 16:26.
Article22. Ooi YH, Oh DJ, Rhee DJ. Effect of bimatoprost, latanoprost, and unoprostone on matrix metalloproteinases and their inhibitors in human ciliary body smooth muscle cells. Invest Ophthalmol Vis Sci. 2009; 50:5259–5265.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Outcome of Triple Procedure in Open-Angle Glaucoma and Angle-Closure Glaucoma
- Factors Affecting Post-Cataract OCT Parameters in Open-Angle and Angle-Closure Glaucoma Eyes: Optic Disc Head Analysis
- Clinical Factors that Influence Intraocular Pressure Change after Cataract Surgery in Primary Open-Angle Glaucoma and Angle-Closure Glaucoma
- The Relationship between Open Angle Glaucoma and Refractive Errors
- The Effect of Intraoperative Factors on Intraocular Pressure Reduction after Phacoemulsification in Open-angle Glaucoma