J Neurocrit Care.
2018 Jun;11(1):7-12. 10.18700/jnc.180050.
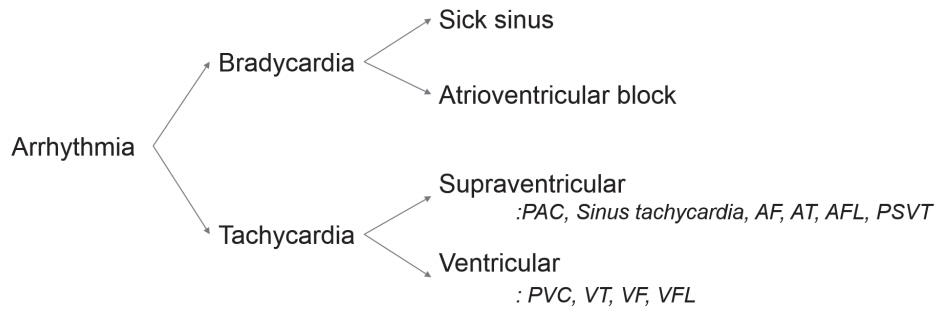
Management of Common Arrhythmia in the Neurological Intensive Care Unit
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. sunghwan@catholic.ac.kr
- KMID: 2426208
- DOI: http://doi.org/10.18700/jnc.180050
Abstract
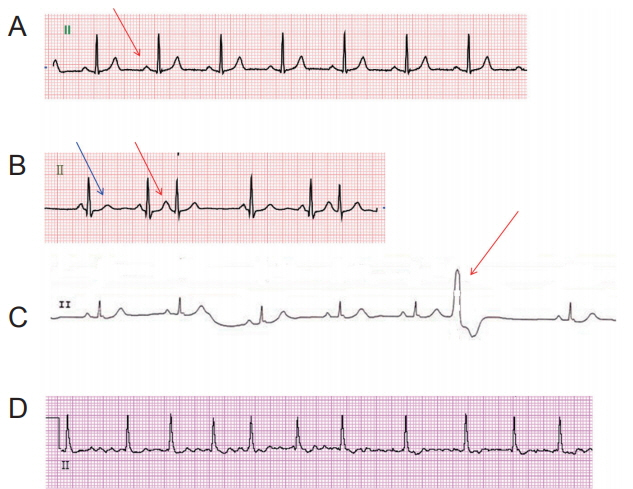
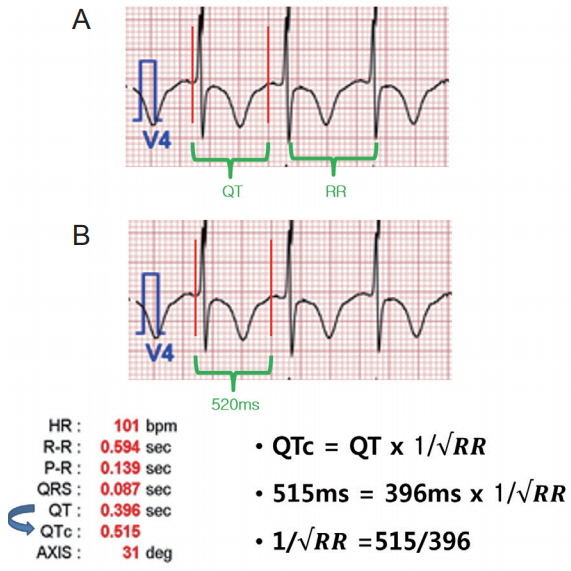
- Cardiac arrhythmias are a common problem in the neurological intensive care unit and represent a major cause of ischemic stroke. Significant arrhythmias are most likely to occur in elderly patients. In this review, we focus on three arrhythmias: premature beats, atrial fibrillation, and QT prolongation. The goal of this review is to provide a current concept of diagnosis and acute management of arrhythmias in the neurological intensive care unit.
MeSH Terms
Figure
Reference
-
1. Conen D, Adam M, Roche F, Barthelemy JC, Felber Dietrich D, Imboden M, et al. Premature atrial contractions in the general population: frequency and risk factors. Circulation. 2012; 126:2302–8.2. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–962.
Article3. Weber-Krüger M, Gröschel K, Mende M, Seegers J, Lahno R, Haase B, et al. Excessive supraventricular ectopic activity is indicative of paroxysmal atrial fibrillation in patients with cerebral ischemia. PLoS One. 2013; 8:e67602.
Article4. Prystowsky EN, Padanilam BJ, Joshi S, Fogel RI. Ventricular arrhythmias in the absence of structural heart disease. J Am Coll Cardiol. 2012; 59:1733–44.
Article5. Maggioni AP, Zuanetti G, Franzosi MG, Rovelli F, Santoro E, Staszewsky L, et al. Prevalence and prognostic significance of ventricular arrhythmias after acute myocardial infarction in the fibrinolytic era. GISSI-2 results. Circulation. 1993; 87:312–22.
Article6. Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996; 335:1933–40.7. Badhwar N, Scheinman MM. Idiopathic ventricular tachycardia: diagnosis and management. Curr Probl Cardiol. 2007; 32:7–43.
Article8. Ling Z, Liu Z, Su L, Zipunnikov V, Wu J, Du H, et al. Radio-frequency ablation versus antiarrhythmic medication for treatment of ventricular premature beats from the right ventricular outflow tract: prospective randomized study. Circ Arrhythm Electrophysiol. 2014; 7:237–43.9. Krittayaphong R, Bhuripanyo K, Punlee K, Kangkagate C, Chaithiraphan S. Effect of atenolol on symptomatic ventricular arrhythmia without structural heart disease: a randomized placebo-controlled study. Am Heart J. 2002; 144:e10.
Article10. Gill JS, Blaszyk K, Ward DE, Camm AJ. Verapamil for the suppression of idiopathic ventricular tachycardia of left bundle branch block-like morphology. Am Heart J. 1993; 126:1126–33.
Article11. Zipes DP, Foster PR, Troup PJ, Pedersen DH. Atrial induction of ventricular tachycardia: reentry versus triggered automaticity. Am J Cardiol. 1979; 44:1–8.
Article12. Haim M, Hoshen M, Reges O, Rabi Y, Balicer R, Leibowitz M. Prospective national study of the prevalence, incidence, management and outcome of a large contemporary cohort of patients with incident non-valvular atrial fibrillation. J Am Heart Assoc. 2015; 4:e001486.
Article13. Son MK, Lim NK, Cho MC, Park HY. Incidence and risk factors for atrial fibrillation in Korea: the National Health Insurance Service Database (2002-2010). Korean Circ J. 2016; 46:515–21.
Article14. Psaty BM, Manolio TA, Kuller LH, Kronmal RA, Cushman M, Fried LP, et al. Incidence of and risk factors for atrial fibrillation in older adults. Circulation. 1997; 96:2455–61.
Article15. Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006; 114:119–25.
Article16. Salman S, Bajwa A, Gajic O, Afessa B. Paroxysmal atrial fibrillation in critically ill patients with sepsis. J Intensive Care Med. 2008; 23:178–83.17. Kanji S, Williamson DR, Yaghchi BM, Albert M, McIntyre L. Epidemiology and management of atrial fibrillation in medical and noncardiac surgical adult intensive care unit patients. J Crit Care. 2012; 27:326.e1–326.e8.
Article18. Lee DH. Cardiac complications in patients admitted to the neuro-intensive care unit. J Neurocrit Care. 2017; 10:7–12.
Article19. Nam GB. Cardiac arrhythmias in the intensive care units. J Neurocrit Care. 2014; 7:25–32.
Article20. Andrew NE, Thrift AG, Cadilhac DA. The prevalence, impact and economic implications of atrial fibrillation in stroke: what progress has been made? Neuroepidemiology. 2013; 40:227–39.
Article21. Baek MS, Kim JH, Song D, Ahn SJ, Suh KD, Lee KY. Two cases of superior mesenteric artery occlusion in acute cerebral infarction patients with atrial fibrillation. J Neurocrit Care. 2016; 9:178–82.
Article22. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014; 130:2071–104.
Article23. Kim T, Jung SW, Lee KS, Park HJ, Kim JS, Koo J, et al. CHA2DS2-VASc scores are proportionally associated with left atrial enlargement and serum D-dimer levels in patients with non-valvular atrial fibrillation. J Neurocrit Care. 2016; 9:139–43.24. Sato H, Ishikawa K, Kitabatake A, Ogawa S, Maruyama Y, Yokota Y, et al. Low-dose aspirin for prevention of stroke in low-risk patients with atrial fibrillation: Japan Atrial Fibrillation Stroke Trial. Stroke. 2006; 37:447–51.25. Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. 2011; 306:2248–54.
Article26. Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, et al. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002; 347:1825–33.
Article27. Sherman DG, Kim SG, Boop BS, Corley SD, Dimarco JP, Hart RG, et al. Occurrence and characteristics of stroke events in the Atrial Fibrillation Follow-up Investigation of Sinus Rhythm Management (AFFIRM) study. Arch Intern Med. 2005; 165:1185–91.
Article28. Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, et al. Relationships between sinus rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) study. Circulation. 2004; 109:1509–13.
Article29. Wijffels MC, Kirchhof CJ, Dorland R, Allessie MA. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995; 92:1954–68.30. CredibleMeds®. List of QT Clinical Factors Launched - QTFactors.org; Free Smartphone App for QTdrugs Lists [online]. Available at: https://crediblemeds.org/. Accessed January 1, 2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Supraventricular Arrhythmias in the Surgical Intensive Care Unit
- Cardiac Complications in Patients Admitted to the Neuro-Intensive Care Unit
- Glucose Control in Intensive Care Unit Patients: Recent Updates
- Risk Factors for Cognitive Impairment in Intensive Care Unit Survivors
- Effects of Radiation Safety Management Education with the Use of a Booklet for Intensive Care Unit Nurses