Intest Res.
2017 Apr;15(2):215-220. 10.5217/ir.2017.15.2.215.
Clinical outcomes of sigmoid colon volvulus: identification of the factors associated with successful endoscopic detorsion
- Affiliations
-
- 1Department of Gastroenterology, Muroran City General Hospital, Muroran, Japan.
- 2Department of Gastroenterology and Hepatology, Sapporo Medical University School of Medicine, Sapporo, Japan. hiropynakase@gmail.com
- KMID: 2425164
- DOI: http://doi.org/10.5217/ir.2017.15.2.215
Abstract
- BACKGROUND/AIMS
Although multiple treatment options exist for the management of sigmoid colon volvulus, no study has examined the factors associated with successful endoscopic detorsion. This study aimed to examine the clinical course of patients with sigmoid colon volvulus and to identify factors related to successful endoscopic detorsion.
METHODS
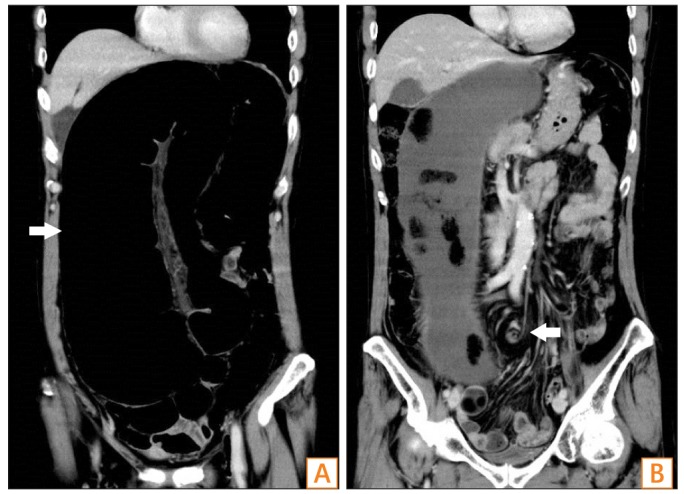
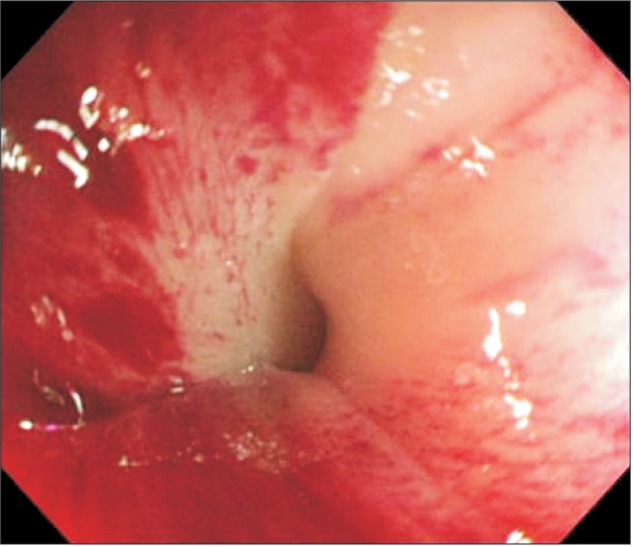
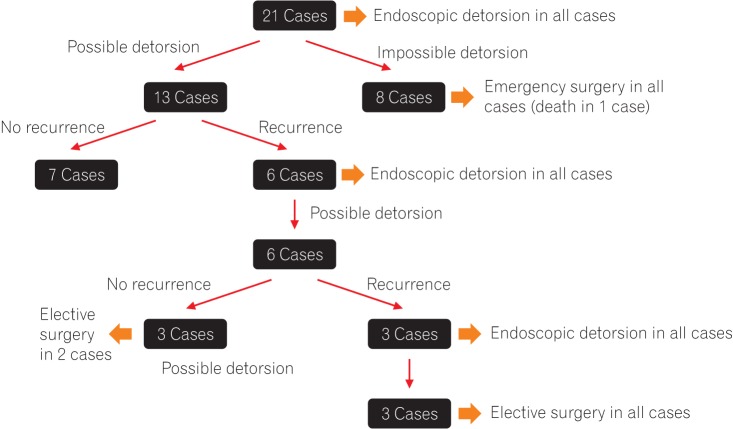
This study included 30 cases (21 patients) of sigmoid volvulus from among 545 cases of intestinal obstruction at a single center. We retrospectively examined the clinical course and the factors associated with the possibility of endoscopic detorsion of sigmoid colon volvulus.
RESULTS
The rate of laxative use among the study participants was 76.2%; the rate of comorbid neuropsychiatric disorders was 61.9%; and 57.1% of patients had a history of open abdominal surgery. All patients were initially treated with endoscopic detorsion, and this procedure had a 61.9% success rate. The recurrence rate after detorsion was as high as 46.2%, but detorsion during revision endoscopy was possible in all cases. Statistical analysis revealed that the absence of abdominal tenderness (P=0.027), the use of laxatives (P=0.027), and a history of open abdominal surgery (P=0.032) were factors predictive of successful endoscopic detorsion.
CONCLUSIONS
The results of our study are consistent with previous reports with respect to the success rate of endoscopic detorsion, the subsequent recurrence rate, and the proportion of patients requiring surgical treatment. In addition, we identified the absence of abdominal tenderness, the use of laxatives, and history of open abdominal surgery as factors predicting successful endoscopic detorsion of sigmoid colon volvulus.
MeSH Terms
Figure
Cited by 2 articles
-
Author's Reply
Tomoya Iida, Hiroyuki Kaneto, Hiroshi Nakase
Intest Res. 2017;15(4):554-554. doi: 10.5217/ir.2017.15.4.554.Comments on clinical outcomes of sigmoid colon volvulus: identification of the factors associated with successful endoscopic detorsion
Sabri Selcuk Atamanalp
Intest Res. 2017;15(4):552-553. doi: 10.5217/ir.2017.15.4.552.
Reference
-
1. Påhlman L, Enblad P, Rudberg C, Krog M. Volvulus of the colon: a review of 93 cases and current aspects of treatment. Acta Chir Scand. 1989; 155:53–56. PMID: 2929205.2. Oncü M, Pískín B, Calik A, Yandi M, Alhan E. Volvulus of the sigmoid colon. S Afr J Surg. 1991; 29:48–49. PMID: 1882313.3. Halabi WJ, Jafari MD, Kang CY, et al. Colonic volvulus in the United States: trends, outcomes, and predictors of mortality. Ann Surg. 2014; 259:293–301. PMID: 23511842.4. Kasten KR, Marcello PW, Roberts PL, et al. What are the results of colonic volvulus surgery? Dis Colon Rectum. 2015; 58:502–507. PMID: 25850837.
Article5. Brothers TE, Strodel WE, Eckhauser FE. Endoscopy in colonic volvulus. Ann Surg. 1987; 206:1–4. PMID: 3606228.
Article6. Hiltunen KM, Syrjä H, Matikainen M. Colonic volvulus: diagnosis and results of treatment in 82 patients. Eur J Surg. 1992; 158:607–611. PMID: 1363066.7. Oren D, Atamanalp SS, Aydinli B, et al. An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Dis Colon Rectum. 2007; 50:489–497. PMID: 17205203.
Article8. Akinkuotu A, Samuel JC, Msiska N, Mvula C, Charles AG. The role of the anatomy of the sigmoid colon in developing sigmoid volvulus: a case-control study. Clin Anat. 2011; 24:634–637. PMID: 21322064.
Article9. Asbun HJ, Castellanos H, Balderrama B, et al. Sigmoid volvulus in the high altitude of the Andes: review of 230 cases. Dis Colon Rectum. 1992; 35:350–353. PMID: 1582356.11. Safioleas M, Chatziconstantinou C, Felekouras E, et al. Clinical considerations and therapeutic strategy for sigmoid volvulus in the elderly: a study of 33 cases. World J Gastroenterol. 2007; 13:921–924. PMID: 17352024.
Article12. Tan KK, Chong CS, Sim R. Management of acute sigmoid volvulus: an institution's experience over 9 years. World J Surg. 2010; 34:1943–1948. PMID: 20372894.
Article13. Atamanalp SS. Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Tech Coloproctol. 2013; 17:561–569. PMID: 23636444.
Article14. Larkin JO, Thekiso TB, Waldron R, Barry K, Eustace PW. Recurrent sigmoid volvulus: early resection may obviate later emergency surgery and reduce morbidity and mortality. Ann R Coll Surg Engl. 2009; 91:205–209. PMID: 19335969.
Article15. Dülger M, Cantürk NZ, Utkan NZ, Gonullu NN. Management of sigmoid colon volvulus. Hepatogastroenterology. 2000; 47:1280–1283. PMID: 11100333.16. Khanna AK, Kumar P, Khanna R. Sigmoid volvulus: study from a north Indian hospital. Dis Colon Rectum. 1999; 42:1081–1084. PMID: 10458135.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comments on clinical outcomes of sigmoid colon volvulus: identification of the factors associated with successful endoscopic detorsion
- Laparoscopic Management of Sigmoid Volvulus for Which Endoscopic Reduction had Failed
- A Case of Emergency Endoscopic Treatment of Sigmoid Volvulus
- Chronic Constipation Led to Sigmoid Volvulus in a Child
- A Case of Sigmoid Volvulus Treated by Emergency Endoscopic Reduction and Surgical Colonic Resection