Hip Pelvis.
2017 Jun;29(2):104-112. 10.5371/hp.2017.29.2.104.
Radiographic Outcomes of Osteosynthesis Using Proximal Femoral Nail Antirotation (PFNA) System in Intertrochanteric Femoral Fracture: Has PFNA II Solved All the Problems?
- Affiliations
-
- 1Department of Orthopaedic Surgery, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea. kuentak@pusan.ac.kr
- 2Department of Orthopaedic Surgery, Pusan National University Hospital, Busan, Korea.
- KMID: 2424238
- DOI: http://doi.org/10.5371/hp.2017.29.2.104
Abstract
- PURPOSE
We evaluated the geometric discrepancies between the proximal femur in Koreans and two types of proximal femoral nail using plain radiographs.
MATERIALS AND METHODS
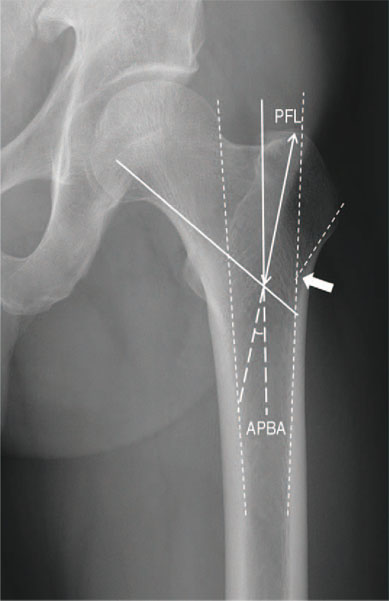
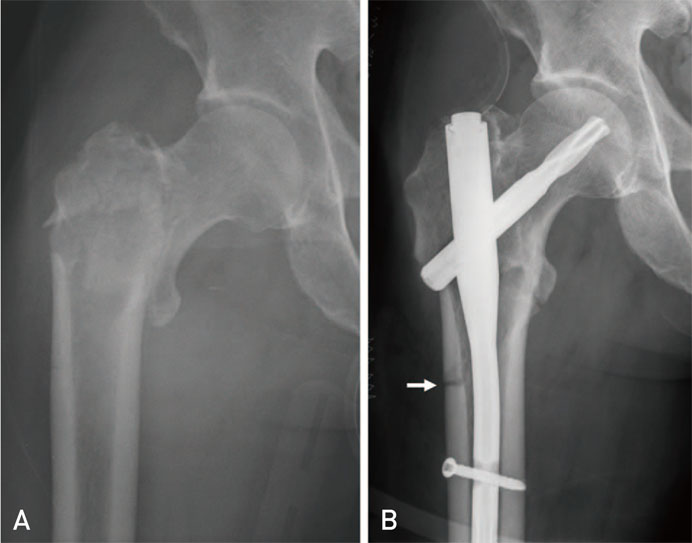
A total of 100 consecutive patients (38 treated with proximal femoral nail antirotation [PFNA], 62 PFNA II) with intertrochanteric fracture were retrospectively identified. The minimum follow up period was 32 months. The geometric analysis of the proximal femur was performed using preoperative true hip antero-posterior radiographs of the unaffected side, and the data were compared with the PFNA and PFNA II dimensions. Postoperative assessments were performed using postoperative radiographs for the proximal protruding length of nail tip, quality of reduction, implant position and the presence of lateral cortical impingement.
RESULTS
The geometric dimensions of the proximal femur were different between the two proximal femoral nail types. No impingement was detected in patients treated with PFNA II, whereas 13 cases of lateral impingement were observed in patients treated with PFNA. A significant association was observed between the short proximal femur and the presence of lateral cortical impingement (P=0.032) and between impingement and intraoperative reduction loss (P=0.012). Proximal protrusion of the nail tip was seen in 71 patients and no difference was observed between two groups.
CONCLUSION
Our study demonstrates that the flat lateral surface of PFNA II can avoid lateral cortical impingement, which provide better fixation for intertrochanteric fracture. However, there was still a problem associated with longer proximal end of PFNA II compared with the proximal femoral length in Korean.
Keyword
Figure
Reference
-
1. Gardenbroek TJ, Segers MJ, Simmermacher RK, Hammacher ER. The proximal femur nail antirotation: an identifiable improvement in the treatment of unstable pertrochanteric fractures? J Trauma. 2011; 71:169–174.
Article2. Garg B, Marimuthu K, Kumar V, Malhotra R, Kotwal PP. Outcome of short proximal femoral nail antirotation and dynamic hip screw for fixation of unstable trochanteric fractures. A randomised prospective comparative trial. Hip Int. 2011; 21:531–536.
Article3. Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006; 37:984–989.
Article4. Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010; 38:1266–1275.
Article5. Verettas DA, Ifantidis P, Chatzipapas CN, et al. Systematic effects of surgical treatment of hip fractures: gliding screw-plating vs intramedullary nailing. Injury. 2010; 41:279–284.
Article6. Macheras GA, Koutsostathis SD, Galanakos S, Kateros K, Papadakis SA. Does PFNA II avoid lateral cortex impingement for unstable peritrochanteric fractures? Clin Orthop Relat Res. 2012; 470:3067–3076.
Article7. Tao YL, Ma Z, Chang SM. Does PFNA II avoid lateral cortex impingement for unstable peritrochanteric fractures? Clin Orthop Relat Res. 2013; 471:1393–1394.
Article8. Tyagi V, Yang JH, Oh KJ. A computed tomography-based analysis of proximal femoral geometry for lateral impingement with two types of proximal femoral nail anterotation in subtrochanteric fractures. Injury. 2010; 41:857–861.
Article9. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992; 2:285–289.
Article10. Kim DS, Shon HC, Kim YM, Choi ES, Park KJ, Im SH. Postoperative mortality and the associated factors for senile hip fracture patients. J Korean Orthop Assoc. 2008; 43:488–494.
Article11. Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Berlin, Heidelberg, New York: Spinger-Verlag;1990.12. Boldin C, Seibert FJ, Fankhauser F, Peicha G, Grechenig W, Szyszkowitz R. The proximal femoral nail (PFN)--a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow-up of 15 months. Acta Orthop Scand. 2003; 74:53–58.
Article13. Baumgaertner MR. The pertrochanteric external fixator reduced pain, hospital stay, and mechanical complications in comparison with the sliding hip screw. J Bone Joint Surg Am. 2002; 84-A:1488.14. Clevenland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959; 41-A:1399–1408.15. AO Synthes. The manual of PFNA and PFNA II. Paoli, Switzerland: AO Synthes;2011.16. Hwang JH, Oh JK, Han SH, Shon WY, Oh CW. Mismatch between PFNa and medullary canal causing difficulty in nailing of the pertrochanteric fractures. Arch Orthop Trauma Surg. 2008; 128:1443–1446.
Article17. Khang G, Choi K, Kim CS, Yang JS, Bae TS. A study of Korean femoral geometry. Clin Orthop Relat Res. 2003; (406):116–122.
Article18. Sommers MB, Roth C, Hall H, et al. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma. 2004; 18:361–368.
Article19. Lee KB, Lee BT. Complications of femoral pertrochanteric fractures treated with proximal femoral nail (PFN). J Korean Fract Soc. 2007; 20:33–39.
Article20. Boopalan PR, Oh JK, Kim TY, Oh CW, Cho JW, Shon WY. Incidence and radiologic outcome of intraoperative lateral wall fractures in OTA 31A1 and A2 fractures treated with cephalomedullary nailing. J Orthop Trauma. 2012; 26:638–642.
Article21. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P. Hip Fracture Study Group. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007; 89:470–475.
Article22. Hsu CE, Shih CM, Wang CC, Huang KC. Lateral femoral wall thickness. A reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. Bone Joint J. 2013; 95-B:1134–1138.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the Clinical and Radiological Outcomes of TFNA (Trochanteric Fixation Nail-Advanced) and PFNA-II (Proximal Femoral Nail Antirotation-II) Treatment in Elderly Patients with Intertrochanteric Fractures
- Comparison of the Compression Hip Screw (CHS) and the Proximal Femoral Nail Antirotation (PFNA) for Intertrochanteric Femoral Fracture
- Excessive Sliding of the Helical Blade and the Femoral Neck Fracture after Insertion of Proximal Femoral Nail Anti-Rotation for Type A2 Intertrochanteric Fractures - A Case Report -
- Treatment of the Proximal Femoral Extracapsular Fracture with Proximal Femoral Nail Antirotation (PFNA): Comparison with Proximal Femoral Nail (PFN)
- Comparative Study of Proximal Femoral Nail Antirotation and Zimmer Natural Nail for the Treatment of Stable Intertrochanteric Fractures