Korean J Gastroenterol.
2018 Oct;72(4):209-212. 10.4166/kjg.2018.72.4.209.
Asymptomatic Splenic Cysts in an Immunocompromised Patient: Should They Be Investigated
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Catholic Kwandong University, International St. Mary's Hospital, College of Medicine, Catholic Kwandong University, Incheon, Korea. baegmk@gmail.com
- KMID: 2424113
- DOI: http://doi.org/10.4166/kjg.2018.72.4.209
Abstract
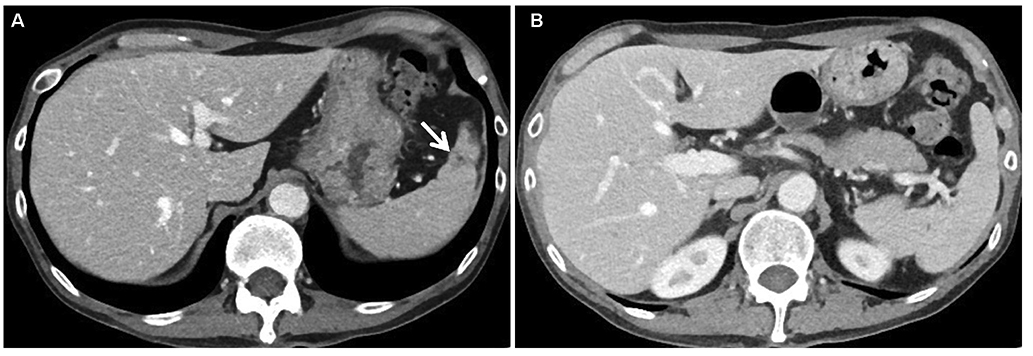
- Splenic abscess is a rare disease that generally occurs in immunocompromised patients. It is difficult to distinguish between splenic abscesses and cysts using imaging studies, especially if they are asymptomatic. A 50-year-old asymptomatic man who had received steroid therapy for underlying rheumatoid arthritis was referred to a university hospital due to presence of several splenic cysts, with the largest being 3.5 cm in diameter. Percutaneous aspiration was performed, and fluid analysis showed cysts infected by extended-spectrum, beta-lactamase-producing Escherichia coli. The patient was treated with ertapenem for four weeks, and the lesion disappeared on follow-up imaging studies. Splenic abscess should be included as a differential diagnosis of splenic cystic lesions in immunocompromised patients.
MeSH Terms
Figure
Reference
-
1. Chou YH, Hsu CC, Tiu CM, Chang T. Splenic abscess: sonographic diagnosis and percutaneous drainage or aspiration. Gastrointest Radiol. 1992; 17:262–266.
Article2. Ng KK, Lee TY, Wan YL, et al. Splenic abscess: diagnosis and management. Hepatogastroenterology. 2002; 49:567–571.3. Green BT. Splenic abscess: report of six cases and review of the literature. Am Surg. 2001; 67:80–85.4. de Bree E, Tsiftsis D, Christodoulakis M, Harocopos G, Schoretsanitis G, Melissas J. Splenic abscess: a diagnostic and therapeutic challenge. Acta Chir Belg. 1998; 98:199–202.5. Schiavo L, Scalera G, De Sena G, Ciorra FR, Pagliano P, Barbarisi A. Nonsurgical management of multiple splenic abscesses in an obese patient that underwent laparoscopic sleeve gastrectomy: case report and review of literature. Clin Case Rep. 2015; 3:870–874.
Article6. Tung CC, Chen FC, Lo CJ. Splenic abscess: an easily overlooked disease? Am Surg. 2006; 72:322–325.
Article7. Heller MT, Harisinghani M, Neitlich JD, Yeghiayan P, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, part 3: white paper of the ACR incidental findings committee II on splenic and nodal findings. J Am Coll Radiol. 2013; 10:833–839.
Article8. Keogan MT, Freed KS, Paulson EK, Nelson RC, Dodd LG. Imaging-guided percutaneous biopsy of focal splenic lesions: update on safety and effectiveness. AJR Am J Roentgenol. 1999; 172:933–937.
Article9. Gaetke-Udager K, Wasnik AP, Kaza RK, et al. Multimodality imaging of splenic lesions and the role of non-vascular, image-guided intervention. Abdom Imaging. 2014; 39:570–587.
Article10. Ricci ZJ, Oh SK, Chernyak V, et al. Improving diagnosis of atraumatic splenic lesions, part I: nonneoplastic lesions. Clin Imaging. 2016; 40:769–779.
Article11. Urrutia M, Mergo PJ, Ros LH, Torres GM, Ros PR. Cystic masses of the spleen: radiologic-pathologic correlation. Radiographics. 1996; 16:107–129.
Article12. Lee WS, Choi ST, Kim KK. Splenic abscess: a single institution study and review of the literature. Yonsei Med J. 2011; 52:288–292.
Article13. Shakya P, Shrestha D, Maharjan E, Sharma VK, Paudyal R. ESBL production among E. coli and klebsiella spp. Causing urinary tract infection: a hospital based study. Open Microbiol J. 2017; 11:23–30.
Article14. Richter A, Listing J, Schneider M, et al. Impact of treatment with biologic DMARDs on the risk of sepsis or mortality after serious infection in patients with rheumatoid arthritis. Ann Rheum Dis. 2016; 75:1667–1673.
Article