Neurointervention.
2018 Sep;13(2):133-137. 10.5469/neuroint.2018.00934.
Internal Carotid Artery Reconstruction with a “Mega Flow Diverterâ€: First Experience with the 6×50 mm DERIVO Embolization Device
- Affiliations
-
- 1Department of Interventional Neuroradiology, Fundación Jiménez-Diaz Hospital, Madrid, Spain. mariomgaldamez@hotmail.com
- KMID: 2424064
- DOI: http://doi.org/10.5469/neuroint.2018.00934
Abstract
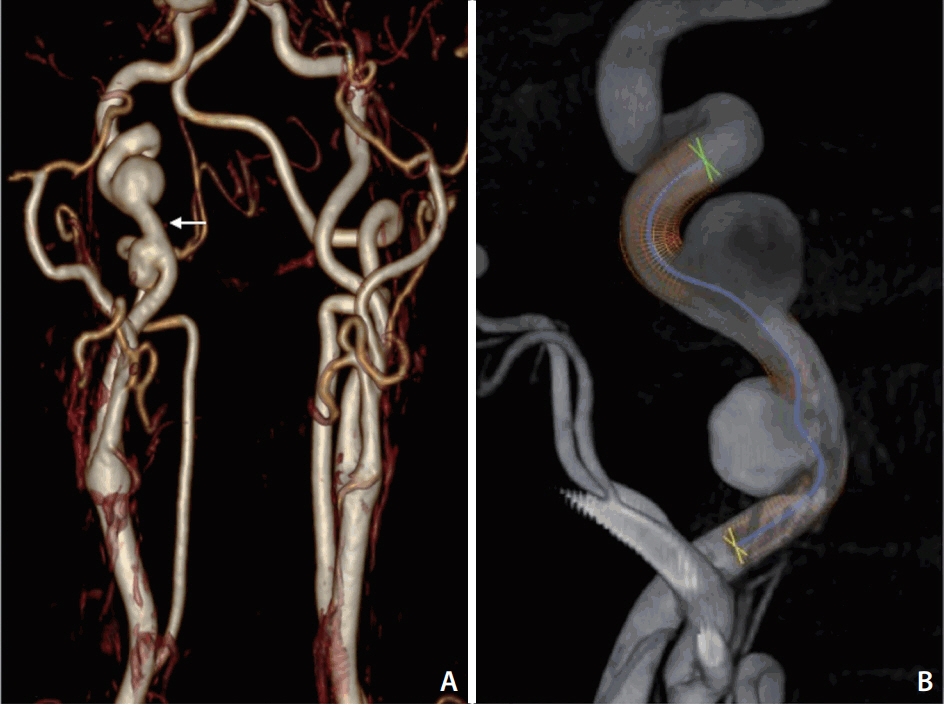
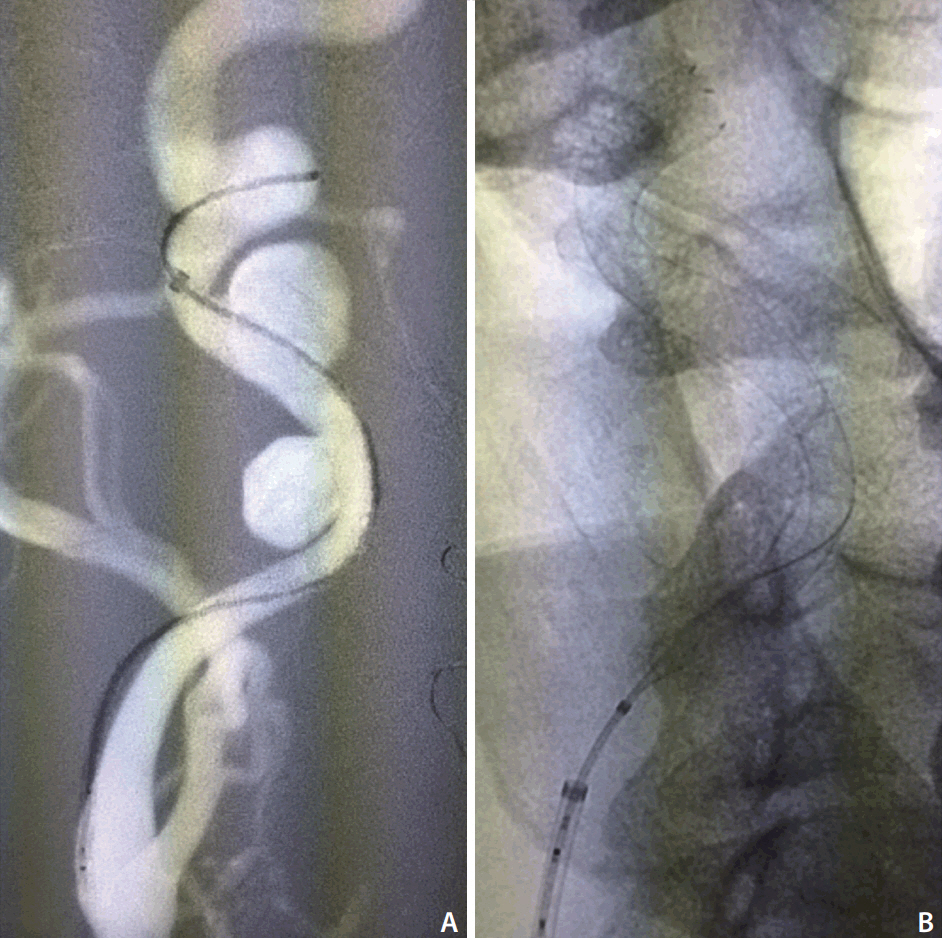
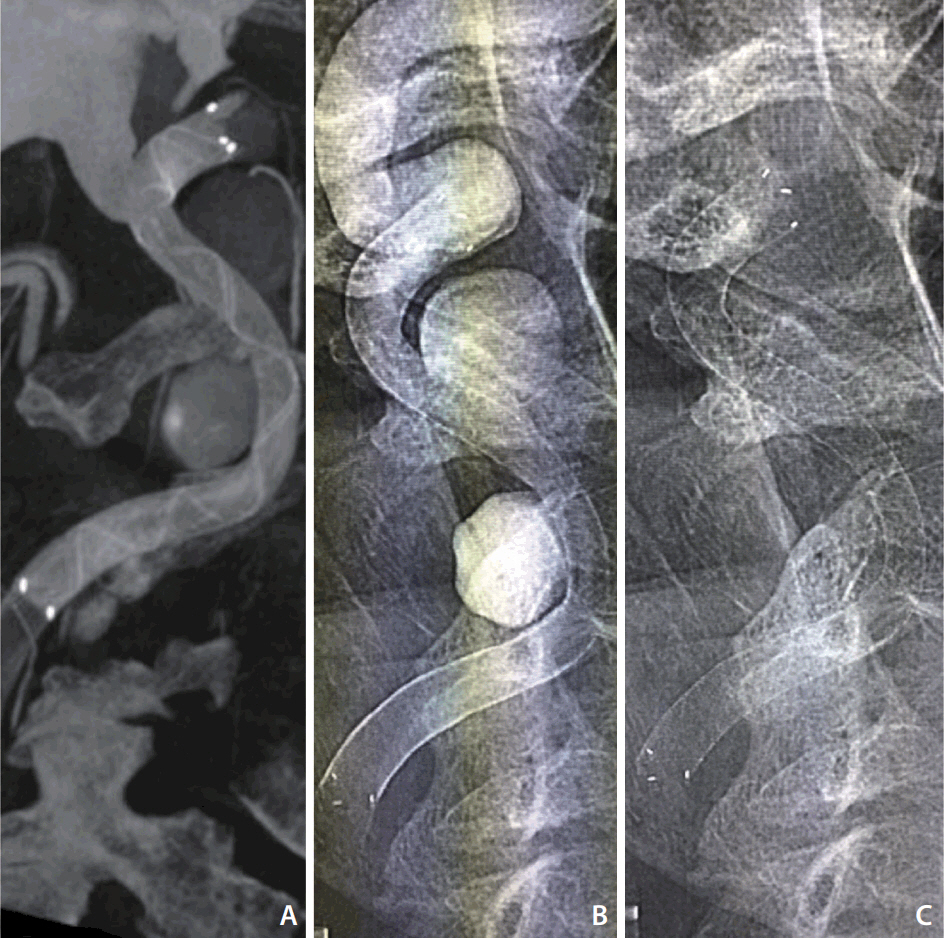
- Endoluminal reconstruction with a flow diverter device has emerged as a viable and often preferable alternative to traditional techniques for the treatment of intracranial aneurysms. Precise measurement and device selection are mandatory steps when considering flow diverters usage in order to avoid potential complications. In this sense, incomplete wall-apposition has been described as a predictive factor for immediate in-stent and delayed thrombosis after stent use. One significant usage limitation of flow diverter devices is the parent artery diameter, since the maximum opening of the sizes available are recommended for vessel diameters between 5.2-5.75 mm. Here we present the first clinical use of the largest flow diverter available, the 6×50 mm DERIVO embolization device (Acandis GmbH & Co. KG, Pforzheim, Germany), into the arterial circulation for a cervical internal carotid artery endovascular reconstruction. This is a new device for large or fusiform aneurysms requiring flow diversion, especially located in the vertebrobasilar system or extracranial segments.
MeSH Terms
Figure
Reference
-
1. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; 44:442–447.
Article2. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 267:858–868.
Article3. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International retrospective study of the Pipeline 705 embolization device: a multicenter aneurysm treatment study. AJNR Am J Neuroradiol. 2015; 36:108–115.4. Becske T, Brinjikji W, Potts MB, Kallmes DF, Shapiro M, Moran CJ, et al. long-term clinical and angiographic outcomes following pipeline embolization device treatment of complex internal carotid artery aneurysms: five-year results of the pipeline for uncoilable or failed aneurysms trial. Neurosurgery. 2017; 80:40–48.
Article5. Martínez-Galdámez M, Pérez S, Vega A, Ruiz P, Caniego JL, Bárcena E, et al. Endovascular treatment of intracranial aneurysms using the pipeline flex embolization device: a case series of 30 consecutive patients. J Neurointerv Surg. 2016; 8:396–401.
Article6. Ong DS, Jang IK. Causes, assessment, and treatment of stent thrombosis--intravascular imaging insights. Nat Rev Cardiol. 2015; 12:325–336.
Article7. Park MS, Albuquerque FC, Nanaszko M, Sanborn MR, Moon K, Abla AA, et al. Critical assessment of complications associated with use of the pipeline embolization device. J Neurointerv Surg. 2015; 7:652–659.
Article8. Martínez-Galdámez M, Ortega-Quintanilla J, Hermosín A, Crespo-Vallejo E, Ailagas JJ, Pérez S. Novel balloon application for rescue and realignment of a proximal-end migrated pipeline flex embolization device into the aneurysmal sac: complication management. J Neurointerv Surg. 2017; 9:e4.9. Roszelle BN, Gonzalez LF, Babiker MH, Ryan J, Albuquerque FC, Frakes DH. Flow diverter effect on cerebral aneurysm hemodynamics: an in vitro comparison of telescoping stents and the pipeline. Neuroradiology. 2013; 55:751–758.
Article10. Tan LA, Keigher KM, Munich SA, Moftakhar R, Lopes DK. Thromboembolic complications with pipeline embolization device placement: impact of procedure time, number of stents and pre-procedure P2Y12 reaction unit (PRU) value. J Neurointerv Surg. 2015; 7:217–221.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Preoperative Embolization of Hypervascular Brain Tumor Fed by Branches of the Internal Carotid Artery
- Embolization of carotid-cavernous fistula using a silicone balloon and a tracker catheter system
- Preoperative Balloon Occlusion Test of the Carotid Artery and Preoperative Tumor Embolization on Paraganglioma of Carotid Body: 20-Year Experience in a Single Institute and Literature Review
- Subacute, Silent Embolization of Amplatzer Atrial Septal Defect Closure Device to the Pulmonary Artery