Neurointervention.
2018 Mar;13(1):20-31. 10.5469/neuroint.2018.13.1.20.
The Combined Use of Intraluminal and Intrasaccular Flow Diversion for the Treatment of Intracranial Aneurysms: Report of 25 Cases
- Affiliations
-
- 1Neuroradiological Clinic, Neurocenter, Klinikum Stuttgart, Germany. bhogalweb@aol.com
- 2Neurological Clinic, Neurocenter, Klinikum Stuttgart, Germany.
- 3Neurosurgical Clinic, Neurocenter, Klinikum Stuttgart, Germany.
- 4Medical Faculty, University Duisburg-Essen, Germany.
- KMID: 2424046
- DOI: http://doi.org/10.5469/neuroint.2018.13.1.20
Abstract
- PURPOSE
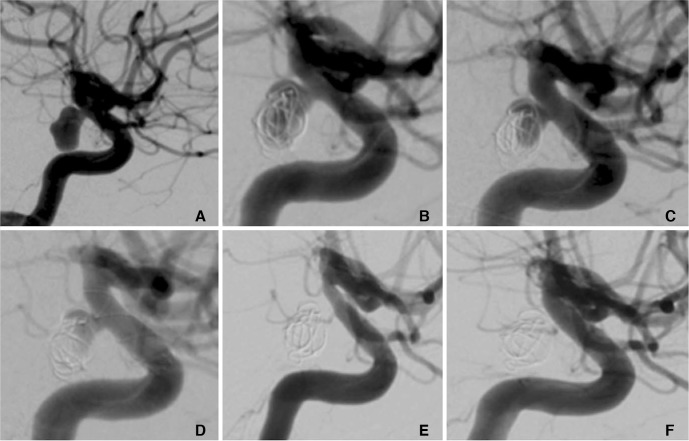
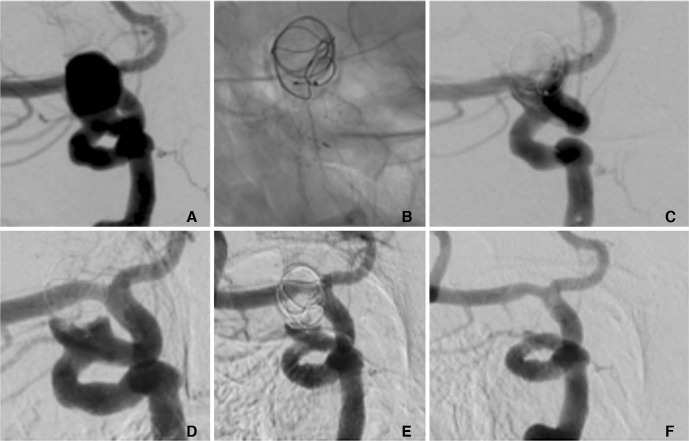
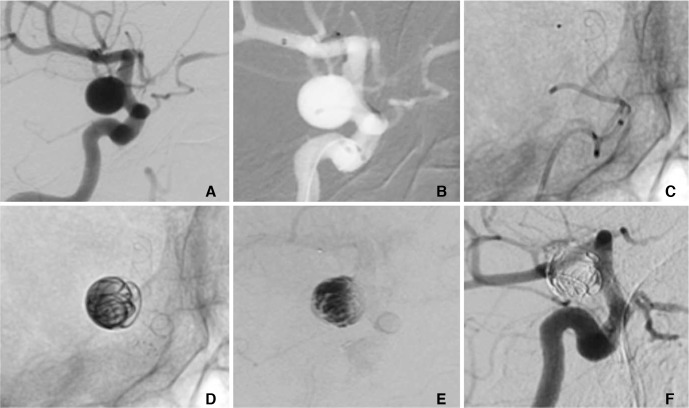
The Medina Embolic Device (MED) is a new intrasaccular device with promising early results. Previously we documented our initial experience of this device both alone and in combination with other devices including flow diverter stents (FDS). We sought to determine the effect of the MED + FDS strategy for the treatment of selected aneurysms.
MATERIALS AND METHODS
We performed a retrospective analysis of prospectively collected data to identify all patients with aneurysms treated using both the MED and intraluminal FDS. We present our technical success rate, early and mid-term angiographic follow-up, and clinical outcome data.
RESULTS
We identified 25 non-consecutive patients. The treatment was staged in 9 patients and in a single session 16 patients. The average age was 61±12.8 years (range 40-82). The average fundus height was 11±3.6 mm and average fundus width was 10.1±3.4 mm. In the staged cohort (n=9) at delayed angiography (mean 10 mths) 8 aneurysms (89%) showed complete exclusion (mRRC 1) and in one patient there was a parent vessel occlusion. In the simultaneous cohort delayed angiography (n=10, mean 8.1 months) demonstrated complete occlusion (mRRC 1) in 6 aneurysms (60%), 3 neck remnants (mRRC 2) (30%) and 1 patient (10%) showed persistent aneurysmal filling (mRRC 3a). There were 5 complications with permanent morbidity (mRS >2) in two patients. There were no mortalities.
CONCLUSION
The MED can be successfully used in combination with intraluminal FDS and in selected aneurysms this may represent an alternative to FDS and adjunctive coiling.
MeSH Terms
Figure
Cited by 1 articles
-
The Combined Use of Intraluminal and Intrasaccular Flow Diversion for the Treatment of Intracranial Aneurysms: Report of 25 Cases
Pervinder Bhogal, Muhammad AlMatter, Victoria Hellstern, Oliver Ganslandt, Hansjörg Bäzner, Hans Henkes, Marta Aguilar-Pérez
Neurointervention. 2018;13(1):20-31. doi: 10.5469/neuroint.2018.13.1.20.
Reference
-
1. Sourour NA, Vande Perre S, Maria FD, Papagiannaki C, Gabrieli J, Pistocchi S, et al. Medina® Embolization Device for the Treatment of Intracranial Aneurysms: Safety and Angiographic Effectiveness at 6 Months. Neurosurgery. 2018; 82:155–162. PMID: 28402453.
Article2. Turk AS, Maia O, Ferreira CC, Freitas D, Mocco J, Hanel R. Periprocedural safety of aneurysm embolization with the Medina Coil System: the early human experience. J Neurointerv Surg. 2016; 8:168–172. PMID: 25628374.
Article3. Aguilar Perez M, Bhogal P, Martinez Moreno R, Bäzner H, Ganslandt O, Henkes H. The Medina Embolic Device: early clinical experience from a single center. J Neurointerv Surg. 2017; 9:77–87. PMID: 27484746.
Article4. Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, et al. An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 2015; 7:496–502. PMID: 24898735.
Article5. You SH, Kong D-S, Kim J-S, Jeon P, Kim KH, Roh HK, et al. Characteristic features of unruptured intracranial aneurysms: predictive risk factors for aneurysm rupture. J Neurol Neurosurg Psychiatry. 2010; 81:479–484. PMID: 19726404.
Article6. Szikora I, Berentei Z, Kulcsar Z, Marosfoi M, Vajda ZS, Lee W, et al. Treatment of intracranial aneurysms by functional reconstruction of the parent artery: the Budapest experience with the pipeline embolization device. AJNR Am J Neuroradiol. 2010; 31:1139–1147. PMID: 20150304.
Article7. Kadirvel R, Ding Y-H, Dai D, Rezek I, Lewis DA, Kallmes DF. Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology. 2014; 270:394–399. PMID: 24086073.
Article8. Fiorella D, Lylyk P, Szikora I, Kelly ME, Albuquerque FC, McDougall CG, et al. Curative cerebrovascular reconstruction with the Pipeline embolization device: the emergence of definitive endovascular therapy for intracranial aneurysms. J Neurointerv Surg. 2009; 1:56–65. PMID: 21994109.
Article9. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A new endoluminal, flow-disrupting device for treatment of saccular aneurysms. Stroke. 2007; 38:2346–2352. PMID: 17615366.10. Kallmes DF, Ding YH, Dai D, Kadirvel R, Lewis DA, Cloft HJ. A second-generation, endoluminal, flow-disrupting device for treatment of saccular aneurysms. AJNR Am J Neuroradiol. 2009; 30:1153–1158. PMID: 19369609.
Article11. Pereira VM, Bonnefous O, Ouared R, Brina O, Stawiaski J, Aerts H, et al. A DSA-based method using contrast-motion estimation for the assessment of the intra-aneurysmal flow changes induced by flow-diverter stents. AJNR Am J Neuroradiol. 2013; 34:808–815. PMID: 23124641.
Article12. Zhang Y, Chong W, Qian Y. Investigation of intracranial aneurysm hemodynamics following flow diverter stent treatment. Med Eng Phys. 2013; 35:608–615. PMID: 22884174.
Article13. Huang Q, Xu J, Cheng J, Wang S, Wang K, Liu J-M. Hemodynamic changes by flow diverters in rabbit aneurysm models: a computational fluid dynamic study based on microcomputed tomography reconstruction. Stroke. 2013; 44:1936–1941. PMID: 23640830.
Article14. Mut F, Raschi M, Scrivano E, Bleise C, Chudyk J, Ceratto R, et al. Association between hemodynamic conditions and occlusion times after flow diversion in cerebral aneurysms. J Neurointerv Surg. 2015; 7:286–290. PMID: 24696500.
Article15. Larrabide I, Geers AJ, Morales HG, Aguilar ML, Rüfenacht DA. Effect of aneurysm and ICA morphology on hemodynamics before and after flow diverter treatment. J Neurointerv Surg. 2015; 7:272–280. PMID: 24692666.
Article16. Kulcsár Z, Augsburger L, Reymond P, Pereira VM, Hirsch S, Mallik AS, et al. Flow diversion treatment: intra-aneurismal blood flow velocity and WSS reduction are parameters to predict aneurysm thrombosis. Acta Neurochir (Wien). 2012; 154:1827–1834. PMID: 22926629.
Article17. Ouared R, Larrabide I, Brina O, Bouillot P, Erceg G, Yilmaz H, et al. Computational fluid dynamics analysis of flow reduction induced by flow-diverting stents in intracranial aneurysms: a patient-unspecific hemodynamics change perspective. J Neurointerv Surg. 2016; [published online ahead of print Feb 15, 2016].
Article18. Jing L, Zhong J, Liu J, Yang X, Paliwal N, Meng H, et al. Hemodynamic Effect of Flow Diverter and Coils in Treatment of Large and Giant Intracranial Aneurysms. World Neurosurg. 2016; 89:199–207. PMID: 26852712.
Article19. Kojima M, Irie K, Fukuda T, Arai F, Hirose Y, Negoro M. The study of flow diversion effects on aneurysm using multiple enterprise stents and two flow diverters. Asian J Neurosurg. 2012; 7:159–165. PMID: 23559981.
Article20. Janiga G, Daróczy L, Berg P, Thévenin D, Skalej M, Beuing O. An automatic CFD-based flow diverter optimization principle for patient-specific intracranial aneurysms. J Biomech. 2015; 48:3846–3852. PMID: 26472308.
Article21. Shobayashi Y, Tateshima S, Kakizaki R, Sudo R, Tanishita K, Viñuela F. Intra-aneurysmal hemodynamic alterations by a self-expandable intracranial stent and flow diversion stent: high intra-aneurysmal pressure remains regardless of flow velocity reduction. J Neurointerv Surg. 2013; 5(Suppl 3):iii38–iii42. PMID: 23048176.
Article22. Augsburger L, Farhat M, Reymond P, Fonck E, Kulcsar Z, Stergiopulos N, et al. Effect of flow diverter porosity on intraaneurysmal blood flow. Klin Neuroradiol. 2009; 19:204–214. PMID: 19705075.
Article23. Frölich AM, Nawka MT, Ernst M, Frischmuth I, Fiehler J, Buhk J-H. Intra-aneurysmal flow disruption after implantation of the Medina® Embolization Device depends on aneurysm neck coverage. PloS One. 2018; 13:e0191975. PMID: 29408857.
Article24. Aguilar Perez M, Bhogal P, Martinez Moreno R, Bäzner H, Ganslandt O, Henkes H. The Medina Embolic Device: early clinical experience from a single center. J Neurointerv Surg. 2017; 9:77–87. PMID: 27484746.25. Bhogal P, Brouwer PA, Yeo L, Svensson M, Söderman M. The Medina Embolic Device: Karolinska experience. Interv Neuroradiol. 2018; 24:4–13. PMID: 28956513.
Article26. Brinjikji W, Murad MH, Lanzino G, Cloft HJ, Kallmes DF. Endovascular treatment of intracranial aneurysms with flow diverters: a meta-analysis. Stroke. 2013; 44:442–447. PMID: 23321438.
Article27. Zhou G, Su M, Zhu Y-Q, Li M-H. Efficacy of Flow-Diverting Devices for Cerebral Aneurysms: A Systematic Review and Meta-analysis. World Neurosurg. 2016; 85:252–262. PMID: 26434569.
Article28. Turowski B, Macht S, Kulcsár Z, Hänggi D, Stummer W. Early fatal hemorrhage after endovascular cerebral aneurysm treatment with a flow diverter (SILK-Stent): do we need to rethink our concepts? Neuroradiology. 2011; 53:37–41. PMID: 20339842.
Article29. Briganti F, Leone G, Napoli M, Lauriola W, Florio F, Maiuri F. Early Fatal Hemorrhage After Endovascular Treatment of a Giant Aneurysm with Flow Diverter Device and Coils. Clin Neuroradiol. 2015; 25:201–205. PMID: 24838287.
Article30. Rouchaud A, Brinjikji W, Lanzino G, Cloft HJ, Kadirvel R, Kallmes DF. Delayed hemorrhagic complications after flow diversion for intracranial aneurysms: a literature overview. Neuroradiology. 2016; 58:171–177. PMID: 26553302.
Article31. Kallmes DF, Hanel R, Lopes D, Boccardi E, Bonafé A, Cekirge S, et al. International Retrospective Study of the Pipeline Embolization Device: A Multicenter Aneurysm Treatment Study. AJNR Am J Neuroradiol. 2015; 36:108–115. PMID: 25355814.
Article32. Cebral JR, Mut F, Raschi M, Scrivano E, Ceratto R, Lylyk P, et al. Aneurysm rupture following treatment with flow-diverting stents: computational hemodynamics analysis of treatment. AJNR Am J Neuroradiol. 2011; 32:27–33. PMID: 21071533.
Article33. Kulcsár Z, Houdart E, Bonafé A, Parker G, Millar J, Goddard AJP, et al. Intra-aneurysmal thrombosis as a possible cause of delayed aneurysm rupture after flow-diversion treatment. AJNR Am J Neuroradiol. 2011; 32:20–25. PMID: 21071538.34. Cebral J, Ollikainen E, Chung BJ, Mut F, Sippola V, Jahromi BR, et al. Flow Conditions in the Intracranial Aneurysm Lumen Are Associated with Inflammation and Degenerative Changes of the Aneurysm Wall. AJNR Am J Neuroradiol. 2017; 38:119–126. PMID: 27686488.
Article35. Velioglu M, Kizilkilic O, Selcuk H, Kocak B, Tureci E, Islak C, et al. Early and midterm results of complex cerebral aneurysms treated with Silk stent. Neuroradiology. 2012; 54:1355–1365. PMID: 22695740.
Article36. Berge J, Biondi A, Machi P, Brunel H, Pierot L, Gabrillargues J, et al. Flow-diverter silk stent for the treatment of intracranial aneurysms: 1-year follow-up in a multicenter study. AJNR Am J Neuroradiol. 2012; 33:1150–1155. PMID: 22300924.
Article37. Damiano RJ, Ma D, Xiang J, Siddiqui AH, Snyder KV, Meng H. Finite Element Modeling of Endovascular Intervention Enables Hemodynamic Prediction of Complex Treatment Strategies for Coiling and Flow Diversion. J Biomech. 2015; 48:3332–3340. PMID: 26169778.
Article38. Lin N, Brouillard AM, Krishna C, Mokin M, Natarajan SK, Sonig A, et al. Use of coils in conjunction with the pipeline embolization device for treatment of intracranial aneurysms. Neurosurgery. 2015; 76:142–149. PMID: 25255261.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Flow diverter stenting for intracranial aneurysms in the pediatric population: Two case reports and literature review
- The Woven EndoBridge Device for the Treatment of Intracranial Aneurysms: Initial Clinical Experience within an Australian Population
- Physiologic Flow Diversion Coiling Technique for Wide-Necked Aneurysms with an Asymmetric Bidirectional Flow at the Aneurysm Neck
- Treatment of In-Stent Stenosis Following Flow Diversion of Intracranial Aneurysms with Cilostazol and Clopidogrel
- Ten Years of Clinical Evaluation of the Woven EndoBridge: A Safe and Effective Treatment for Wide-Neck Bifurcation Aneurysms