J Korean Orthop Assoc.
2017 Dec;52(6):476-483. 10.4055/jkoa.2017.52.6.476.
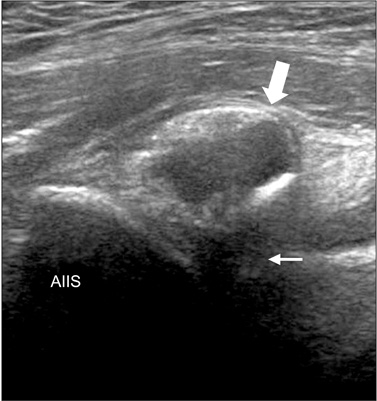
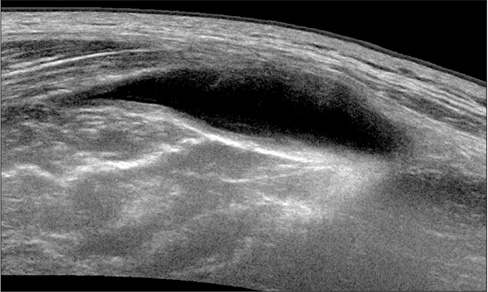
Clinical Usage of Ultrasonography for the Hip Joint
- Affiliations
-
- 1Department of Orthopedic Surgery, Keimyung University School of Medicine, Daegu, Korea. oslee@dsmc.or.kr
- KMID: 2421341
- DOI: http://doi.org/10.4055/jkoa.2017.52.6.476
Abstract
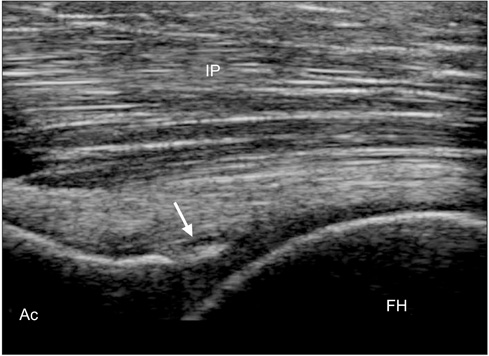
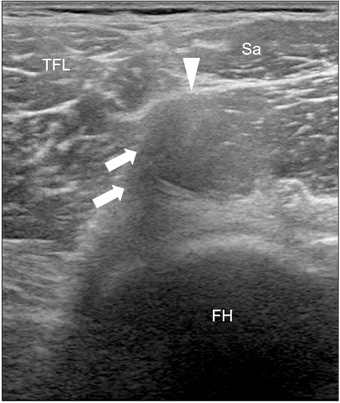
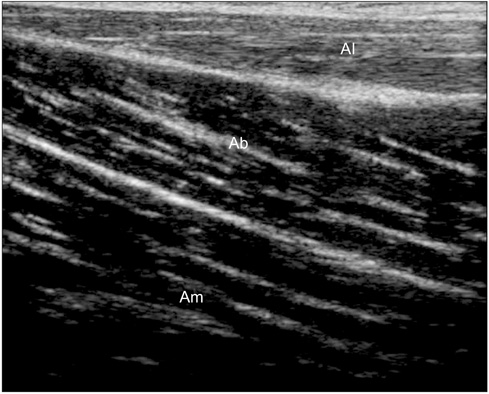
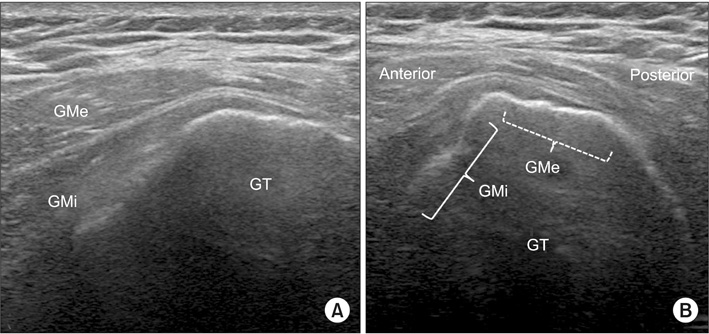
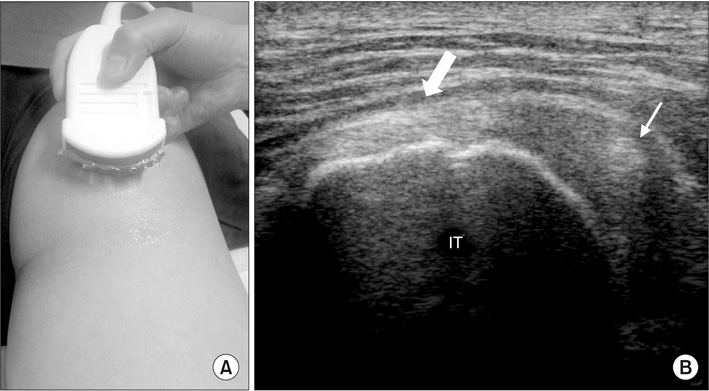
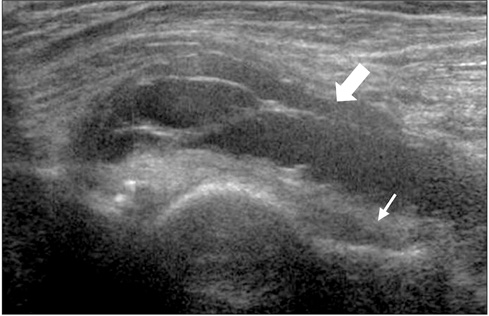
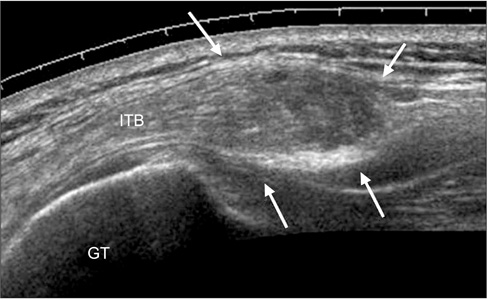
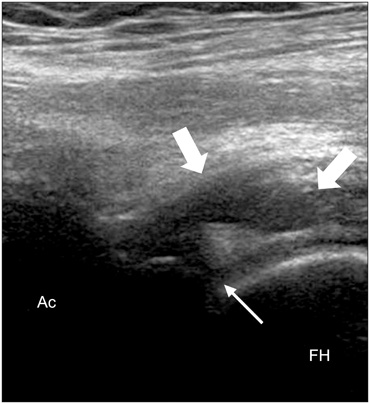
- Thorough history taking and physical examination are highly important for the correct diagnosis of hip disease, and several diagnostic imaging tools are available depending on suspected diseases. Recently, the clinical use of ultrasonography has been increasing due to its relatively low cost, less invasiveness, and the possibility for dynamic evaluation. The purpose of this article was to review the basic technique and normal anatomic images for the clinical usage of ultrasonography around the hip joint and describe typical ultrasonographic findings of several hip diseases.
Keyword
Figure
Reference
-
1. Cardinal E, Beauregard CG, Chhem RK. Interventional musculoskeletal ultrasound. Semin Musculoskelet Radiol. 1997; 1:311–318.
Article2. Dodd GD 3rd, Esola CC, Memel DS, et al. Sonography: the undiscovered jewel of interventional radiology. Radiographics. 1996; 16:1271–1288.
Article3. Rubens DJ, Fultz PJ, Gottlieb RH, Rubin SJ. Effective ultrasonographically guided intervention for diagnosis of musculoskeletal lesions. J Ultrasound Med. 1997; 16:831–842.
Article4. Baffroy-Fayard N. Groupe de travail du CCLIN Paris-Nord. Infection control in interventional radiology: good practice guideline. J Radiol. 2002; 83:351–359.5. Nam WD, Nam SW, Han KY. Ultrasonographic findings of normal hip joint and painful hip due to soft tissue problem. J Korean Orthop Ultrasound Soc. 2010; 3:38–46.6. Louis LJ. Musculoskeletal ultrasound intervention: principles and advances. Radiol Clin North Am. 2008; 46:515–533.
Article7. Rowbotham EL, Grainger AJ. Ultrasound-guided intervention around the hip joint. AJR AM J Roentgenol. 2011; 197:122–127.
Article8. Chu CR, Coyle CH, Chu CT, et al. In vivo effects of single intra-articular injection of 0.5% bupivacaine on articular cartilage. J Bone Joint Surg Am. 2010; 92:599–608.
Article9. Saker MB, Kane RA, Matalon TAS. Factors affecting and techniques to improve needle visualization. Semin Interv Radiol. 1997; 14:471–475.
Article10. Chan YL, Cheng JC, Metreweli C. Sonographic evaluation of hip effusion in children. Improved visualization with the hip in extension and abduction. Acta Radiol. 1997; 38:867–869.11. Robben SG, Lequin MH, Diepstraten AF, den Hollander JC, Entius CA, Meradji M. Anterior joint capsule of the normal hip and in children with transient synovitis: US study with anatomic and histologic correlation. Radiology. 1999; 210:499–507.
Article12. Moss SG, Schweitzer ME, Jacobson JA, et al. Hip joint fluid: detection and distribution at MR imaging and US with cadaveric correlation. Radiology. 1998; 208:43–48.
Article13. Han KY. Painful causes around hip joint and evaluation using ultrasonography. J Korean Orthop Ultrasound Soc. 2009; 2:45–52.14. Karpinski MR, Piggott H. Greater trochanteric pain syndrome. A report of 15 cases. J Bone Joint Surg Br. 1985; 67:762–763.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Application of the Ultrasound in Painful Pediatric Hip
- A Case of Gouty Arthritis Involving the Hip Joint Diagnosed Using Ultrasonography
- Clinical Significance of Ultrasonography for Detection of Hip Joint Effusion in Children: Analysis of the 23 Cases of Transient Synovitis of the Hip
- An ultrasonographic study on measurement of normal hip joint in Korean
- Suppurative Arthritis of the Hip Joint in Coma Patient: Two Cases