J Gastric Cancer.
2018 Sep;18(3):253-263. 10.5230/jgc.2018.18.e27.
Impact of Various Types of Comorbidities on the Outcomes of Laparoscopic Total Gastrectomy in Patients with Gastric Carcinoma
- Affiliations
-
- 1Division of Gastroenterologic Surgery, Department of Surgery, Chonnam National University Hwasun Hospital, Hwasun, Korea. drrsy@jnu.ac.kr
- KMID: 2420785
- DOI: http://doi.org/10.5230/jgc.2018.18.e27
Abstract
- PURPOSE
With increasing life expectancy, the presence of comorbidities has become a major concern in elderly patients who require surgery. However, little is known about the impact of different comorbidities on the outcomes of laparoscopic total gastrectomy (LTG). In this study, we investigated the impact of comorbidities on postoperative complications in patients undergoing LTG for gastric carcinoma.
MATERIALS AND METHODS
We retrospectively reviewed the cases of 303 consecutive patients who underwent LTG for gastric carcinoma between 2005 and 2016. The associations between each comorbidity and postoperative complications were assessed using univariate and multivariate analyses.
RESULTS
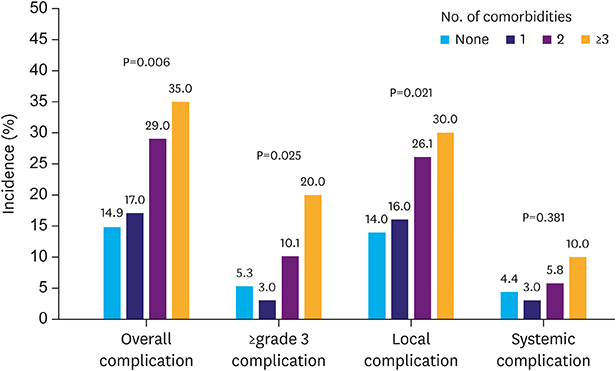
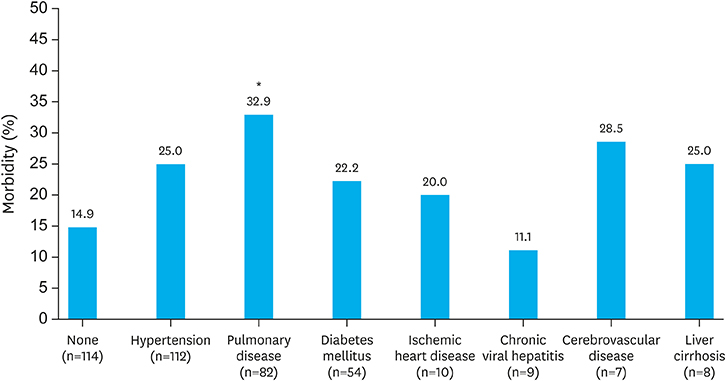
A total of 189 patients (62.4%) had one or more comorbidities. Hypertension was the most common comorbidity (37.0%), followed by diabetes mellitus (17.8%), chronic viral hepatitis (2.6%), liver cirrhosis (2.6%), and pulmonary (27.1%), ischemic heart (3.3%), and cerebrovascular diseases (2.3%). The overall postoperative morbidity and mortality rates were 20.1% and 1.0%, respectively. Patients with pulmonary disease significantly showed higher complication rates than those without comorbidities (32.9% vs. 14.9%, respectively, P=0.003); patient with other comorbidities showed no significant difference in the incidence of LTG-related complications. During univariate and multivariate analyses, pulmonary disease was found to be an independent predictive factor for postoperative complications (odds ratio, 2.14; 95% confidence interval, 1.03-4.64), along with old age and intraoperative bleeding.
CONCLUSIONS
Among the various comorbidities investigated, patients with pulmonary disease had a significantly higher risk of postoperative complications after LTG. Proper perioperative care for optimizing pulmonary function may be required for patients with pulmonary disease.
MeSH Terms
Figure
Reference
-
1. Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012; 255:446–456.2. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008; 248:721–727.3. Information Committee of Korean Gastric Cancer Association. Korean Gastric Cancer Association nationwide survey on gastric cancer in 2014. J Gastric Cancer. 2016; 16:131–140.4. Etoh T, Shiraishi N, Kitano S. Current trends of laparoscopic gastrectomy for gastric cancer in Japan. Asian J Endosc Surg. 2009; 2:18–23.
Article5. Yu J, Hu J, Huang C, Ying M, Peng X, Wei H, et al. The impact of age and comorbidity on postoperative complications in patients with advanced gastric cancer after laparoscopic D2 gastrectomy: results from the Chinese laparoscropic gastrointestinal surgery study (CLASS) group. Eur J Surg Oncol. 2013; 39:1144–1149.
Article6. Park JM, Jin SH, Lee SR, Kim H, Jung IH, Cho YK, et al. Complications with laparoscopically assisted gastrectomy: multivariate analysis of 300 consecutive cases. Surg Endosc. 2008; 22:2133–2139.
Article7. Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, et al. Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale korean multicenter study. Ann Surg Oncol. 2008; 15:2692–2700.
Article8. Inokuchi M, Otsuki S, Ogawa N, Tanioka T, Okuno K, Gokita K, et al. Postoperative complications of laparoscopic total Gastrectomy versus open total gastrectomy for gastric cancer in a meta-analysis of high-quality case-controlled studies. Gastroenterol Res Pract. 2016; 2016:2617903.
Article9. Lin JX, Huang CM, Zheng CH, Li P, Xie JW, Wang JB, et al. Evaluation of laparoscopic total gastrectomy for advanced gastric cancer: results of a comparison with laparoscopic distal gastrectomy. Surg Endosc. 2016; 30:1988–1998.
Article10. Jeong O, Ryu SY, Choi WY, Piao Z, Park YK. Risk factors and learning curve associated with postoperative morbidity of laparoscopic total gastrectomy for gastric carcinoma. Ann Surg Oncol. 2014; 21:2994–3001.
Article11. Kawamura Y, Satoh S, Suda K, Ishida Y, Kanaya S, Uyama I. Critical factors that influence the early outcome of laparoscopic total gastrectomy. Gastric Cancer. 2015; 18:662–668.
Article12. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.13. Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. New York (NY): John Wiley & Sons;2011.14. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.15. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.16. Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014; 23:700–713.
Article17. Tuder RM, Petrache I. Pathogenesis of chronic obstructive pulmonary disease. J Clin Invest. 2012; 122:2749–2755.
Article18. Fields AC, Divino CM. Surgical outcomes in patients with chronic obstructive pulmonary disease undergoing abdominal operations: An analysis of 331,425 patients. Surgery. 2016; 159:1210–1216.
Article19. Kim W, Song KY, Lee HJ, Han SU, Hyung WJ, Cho GS. The impact of comorbidity on surgical outcomes in laparoscopy-assisted distal gastrectomy: a retrospective analysis of multicenter results. Ann Surg. 2008; 248:793–799.20. Cho GS, Kim W, Kim HH, Ryu SW, Kim MC, Ryu SY. Multicentre study of the safety of laparoscopic subtotal gastrectomy for gastric cancer in the elderly. Br J Surg. 2009; 96:1437–1442.
Article21. Wang JB, Zheng CH, Li P, Xie JW, Lin JX, Lu J, et al. Effect of comorbidities on postoperative complications in patients with gastric cancer after laparoscopy-assisted total gastrectomy: results from an 8-year experience at a large-scale single center. Surg Endosc. 2017; 31:2651–2660.
Article22. Hwang SH, Park DJ, Jee YS, Kim HH, Lee HJ, Yang HK, et al. Risk factors for operative complications in elderly patients during laparoscopy-assisted gastrectomy. J Am Coll Surg. 2009; 208:186–192.
Article23. Choi YS, Park DJ, Lee HJ, Kim HH, Yang HK, Lee KU. Laparoscopy-assisted distal gastrectomy for gastric cancer patients with comorbid diseases: is it contraindicated for patients with systemic comorbidity? Surg Laparosc Endosc Percutan Tech. 2011; 21:33–36.24. Inokuchi M, Kato K, Sugita H, Otsuki S, Kojima K. Impact of comorbidities on postoperative complications in patients undergoing laparoscopy-assisted gastrectomy for gastric cancer. BMC Surg. 2014; 14:97.
Article25. Smetana GW, Lawrence VA, Cornell JE. American College of Physicians. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006; 144:581–595.
Article26. Jeong O, Ryu SY, Park YK. The value of preoperative lung spirometry test for predicting the operative risk in patients undergoing gastric cancer surgery. J Korean Surg Soc. 2013; 84:18–26.
Article27. Barisione G, Rovida S, Gazzaniga GM, Fontana L. Upper abdominal surgery: does a lung function test exist to predict early severe postoperative respiratory complications? Eur Respir J. 1997; 10:1301–1308.
Article28. Jacober SJ, Sowers JR. An update on perioperative management of diabetes. Arch Intern Med. 1999; 159:2405–2411.
Article29. Varon J, Marik PE. Perioperative hypertension management. Vasc Health Risk Manag. 2008; 4:615–627.
Article30. Niederman MS, Clemente PH, Fein AM, Feinsilver SH, Robinson DA, Ilowite JS, et al. Benefits of a multidisciplinary pulmonary rehabilitation program. Improvements are independent of lung function. Chest. 1991; 99:798–804.31. Pasquina P, Tramèr MR, Granier JM, Walder B. Respiratory physiotherapy to prevent pulmonary complications after abdominal surgery: a systematic review. Chest. 2006; 130:1887–1899.32. Gracey DR, Divertie MB, Didier EP. Preoperative pulmonary preparation of patients with chronic obstructive pulmonary disease: a prospective study. Chest. 1979; 76:123–129.33. Huang KW, Kuan YC, Chi NF, Huang YH, Luo JC, Chien LN. Chronic obstructive pulmonary disease is associated with increased recurrent peptic ulcer bleeding risk. Eur J Intern Med. 2017; 37:75–82.
Article34. Christensen S, Thomsen RW, Tørring ML, Riis A, Nørgaard M, Sørensen HT. Impact of COPD on outcome among patients with complicated peptic ulcer. Chest. 2008; 133:1360–1366.
Article35. MacNee W. Pulmonary and systemic oxidant/antioxidant imbalance in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2005; 2:50–60.
Article36. Luo JC, Lin HY, Lu CL, Wang LY, Chang FY, Lin HC, et al. Dexamethasone inhibits basic fibroblast growth factor-stimulated gastric epithelial cell proliferation. Biochem Pharmacol. 2008; 76:841–849.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Laparoscopic Total Gastrectomy in Elderly Patients (> or =70 Years) with Gastric Carcinoma: A Retrospective Study
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Current status of robotic gastrectomy for gastric cancer: A review of recent randomized controlled trials
- Laparoscopic Surgery for Gastric Cancer