J Endocr Surg.
2018 Jun;18(2):91-97. 10.16956/jes.2018.18.2.91.
The Consistency of Intraoperative Neural Monitoring in Thyroid Surgery
- Affiliations
-
- 1Division for Endocrine and Minimally Invasive Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy. gdionigi@unime.it
- 2Department of Surgery, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea.
- 3Division of ENT Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy.
- 4Division of Endocrine Surgery, Department of General Surgery, Ege University Hospital, Izmir, Turkey.
- 5Department of Surgery, KUMC Thyroid Center, Korea University Anam Hospital, Seoul, Korea.
- KMID: 2420764
- DOI: http://doi.org/10.16956/jes.2018.18.2.91
Abstract
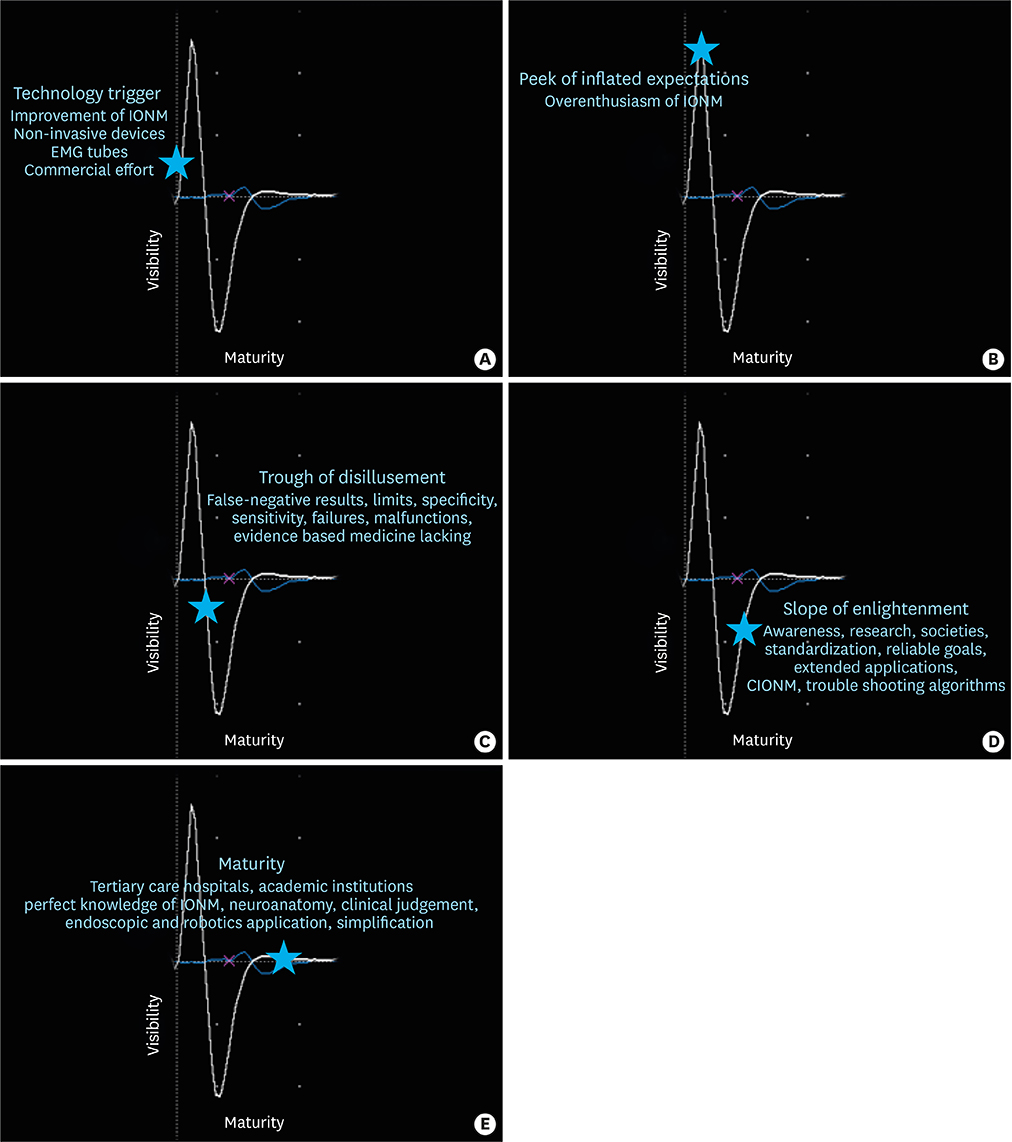
- Numerous operating tools and technology transfers are available for thyroid surgery teams performing open, endoscopic and robotic procedures but none, or very few, of them constitutes a mandatory prerequisite. Over the past decade, the choice of intraoperative neurophysiological monitoring (IONM) of the recurrent laryngeal nerve (RLN), has been reached certain consensus, which must at least be selected on an individual basis. Identification and intraoperative assessment of the RLN seems to be more effectively performed with IONM than solely visually or endoscopically. Today, IONM has evolved sufficiently to increase the likelihood of successful functional outcomes in many patients. The transition from the concept of intermitted neural monitoring of the RLN to that of continuous functions evaluation that must be appreciate requires highly skilled knowledge of IONM. This goal will be more likely achieved in centers highly specialized in thyroid surgery.
Keyword
MeSH Terms
Figure
Reference
-
1. Sala F. Intraoperative neurophysiology is here to stay. Childs Nerv Syst. 2010; 26:413–417.
Article2. Riddell V. Thyroidectomy: prevention of bilateral recurrent nerve palsy. Results of identification of the nerve over 23 consecutive years (1946–69) with a description of an additional safety measure. Br J Surg. 1970; 57:1–11.
Article3. Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg. 2009; 96:240–246.
Article4. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; 121:Suppl 1. S1–S16.
Article5. Schneider R, Sekulla C, Machens A, Lorenz K, Thanh PN, Dralle H. Dynamics of loss and recovery of the nerve monitoring signal during thyroidectomy predict early postoperative vocal fold function. Head Neck. 2016; 38:Suppl 1. E1144–E1151.
Article6. Kim HY, Tufano RP, Randolph G, Barczyński M, Wu CW, Chiang FY, et al. (KINMoS). Impact of positional changes in neural monitoring endotracheal tube on amplitude and latency of electromyographic response in monitored thyroid surgery: results from the porcine experiment. Head Neck. 2016; 38:Suppl 1. E1004–E1008.7. Loch-Wilkinson TJ, Stalberg PL, Sidhu SB, Sywak MS, Wilkinson JF, Delbridge LW. Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg. 2007; 77:377–380.
Article8. Sitges-Serra A, Fontané J, Dueñas JP, Duque CS, Lorente L, Trillo L, et al. Prospective study on loss of signal on the first side during neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy. Br J Surg. 2013; 100:662–666.
Article9. Carlander J, Wagner P, Gimm O, Nordenström E, Jansson S, Bergkvist L, et al. Risk of complications with energy-based surgical devices in thyroid surgery: a national multicenter register study. World J Surg. 2016; 40:117–123.
Article10. Whitfield PC, Kirkpatrick P. Timing of surgery for aneurysmal subarachnoid haemorrhage. Cochrane Database Syst Rev. 2001; CD001697.
Article11. Tator CH. Review of treatment trials in human spinal cord injury: issues, difficulties, and recommendations. Neurosurgery. 2006; 59:957–982.12. Wilson L, Lin E, Lalwani A. Cost-effectiveness of intraoperative facial nerve monitoring in middle ear or mastoid surgery. Laryngoscope. 2003; 113:1736–1745.
Article13. Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A; German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008; 32:1358–1366.
Article14. Kim HY, Liu X, Sun H, Wu CW, Chai YJ, Chung WY, et al. Medico-legal issues of intraoperative neuromonitoring in thyroid surgery. J Endocr Surg. 2017; 17:42–56.
Article15. Dralle H, Schneider R, Lorenz K, Phuong NT, Sekulla C, Machens A. Vocal cord paralysis after thyroid surgery: current medicolegal aspects of intraoperative neuromonitoring. Chirurg. 2015; 86:698–706.16. Dralle H. Surgical assessment of complications after thyroid gland operations. Chirurg. 2015; 86:70–77.17. Dralle H, Lorenz K, Machens A. Verdicts on malpractice claims after thyroid surgery: emerging trends and future directions. Head Neck. 2012; 34:1591–1596.
Article18. Dionigi G, Bartolo V, Rizzo AG, Marullo M, Fabiano V, Catalfamo A, et al. Improving safety of neural monitoring in thyroid surgery: educational considerations in learning new procedure. J Endocr Surg. 2018; 18:21–36.
Article19. Dionigi G, Sun H, Chai YJ, Catalfamo A, Mangraviti A, Rizzo GA, et al. Bilateral vocal palsy after total thyroidectomy: expert opinion on two malpractice claims. J Endocr Surg. 2017; 17:139–148.
Article20. Wang T, Kim HY, Wu CW, Rausei S, Sun H, Pergolizzi FP, et al. Analyzing cost-effectiveness of neural-monitoring in recurrent laryngeal nerve recovery course in thyroid surgery. Int J Surg. 2017; 48:180–188.
Article21. Sanabria Á, Ramírez A. Economic analysis of routine neuromonitoring of recurrent laryngeal nerve in total thyroidectomy. Biomedica. 2015; 35:363–371.22. Rocke DJ, Goldstein DP, de Almeida JR. A cost-utility analysis of recurrent laryngeal nerve monitoring in the setting of total thyroidectomy. JAMA Otolaryngol Head Neck Surg. 2016; 142:1199–1205.
Article23. Al-Qurayshi Z, Kandil E, Randolph GW. Cost-effectiveness of intraoperative nerve monitoring in avoidance of bilateral recurrent laryngeal nerve injury in patients undergoing total thyroidectomy. Br J Surg. 2017; 104:1523–1531.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Technical Instructions for Continuous Intraoperative Neural Monitoring in Thyroid Surgery
- Future Directions of Neural Monitoring in Thyroid Surgery
- Efficacy of Intraoperative Neural Monitoring (IONM) in Thyroid Surgery: the Learning Curve
- Intraoperative Neural Monitoring in Thyroid Surgery: Role and Responsibility of Surgeon
- Surveillance in the Cerebral Aneurysm Surgery