Ann Dermatol.
2018 Oct;30(5):624-626. 10.5021/ad.2018.30.5.624.
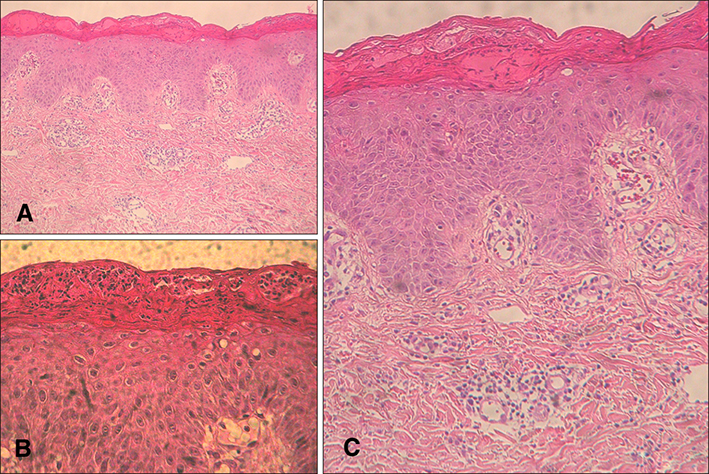
A Case of Abortive Staphylococcal Scalded Skin Syndrome
- Affiliations
-
- 1Department of Dermatology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. dermap@hanmail.net, hyeonekim@gmail.com
- KMID: 2419760
- DOI: http://doi.org/10.5021/ad.2018.30.5.624
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Park AY, Yeon EK, Lee HK, Shin MY. A clinical review of staphylococcal scalded skin syndrome for the last 10 years. Soonchunhyang Med Sci. 2012; 18:32–37.
Article2. Patel GK, Finlay AY. Staphylococcal scalded skin syndrome: diagnosis and management. Am J Clin Dermatol. 2003; 4:165–175.3. Ladhani S, Evans RW. Staphylococcal scalded skin syndrome. Arch Dis Child. 1998; 78:85–88.
Article4. Park JW, Hwang DK, Yu HJ. Staphylococcal scalded skin syndrome, review of 20 cases. Korean J Dermatol. 2002; 40:1051–1057.5. Kang JD, Park SD. Reclassification of staphylococcal scalded skin syndrome by clinical analysis of 25 cases. Korean J Dermatol. 2004; 42:398–405.