J Korean Soc Radiol.
2018 Sep;79(3):114-122. 10.3348/jksr.2018.79.3.114.
Breast Ultrasound Computer-Aided Diagnosis: Analysis of Types of Errors
- Affiliations
-
- 1Department of Radiology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
- 2Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. gmlionmain@gmail.com
- KMID: 2418652
- DOI: http://doi.org/10.3348/jksr.2018.79.3.114
Abstract
- PURPOSE
The aim of this study was to evaluate the diagnostic performance of breast ultrasound (US) computer-aided diagnosis (CAD) to distinguish between benign and malignant lesions and analyze features of lesions interpreted with errors retrospectively.
MATERIALS AND METHODS
Three hundred and sixteen women with 375 breast lesions were enrolled. We assessed the accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV). Additionally, we evaluated the causes and patterns of the misinterpretation in the false positive and negative groups.
RESULTS
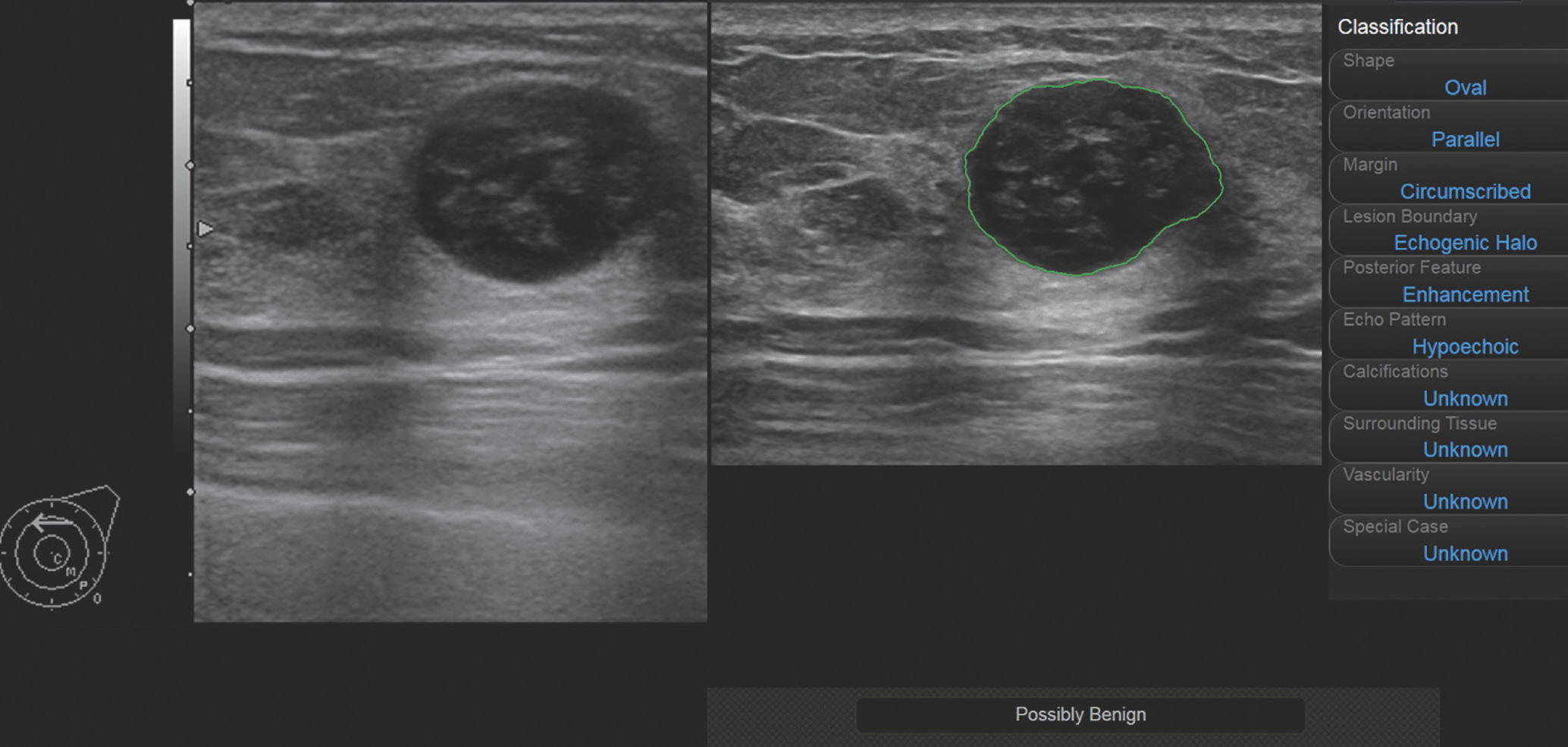
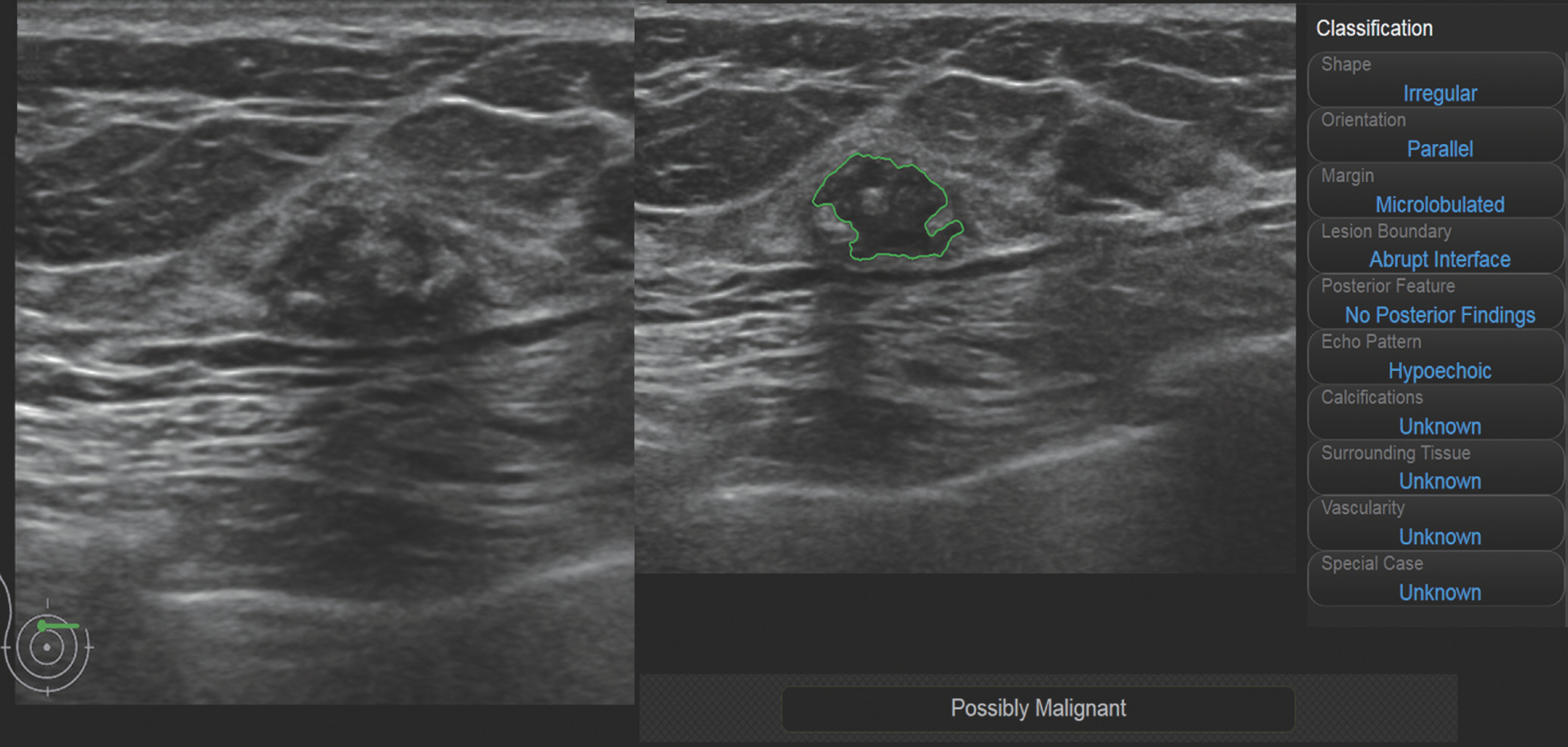
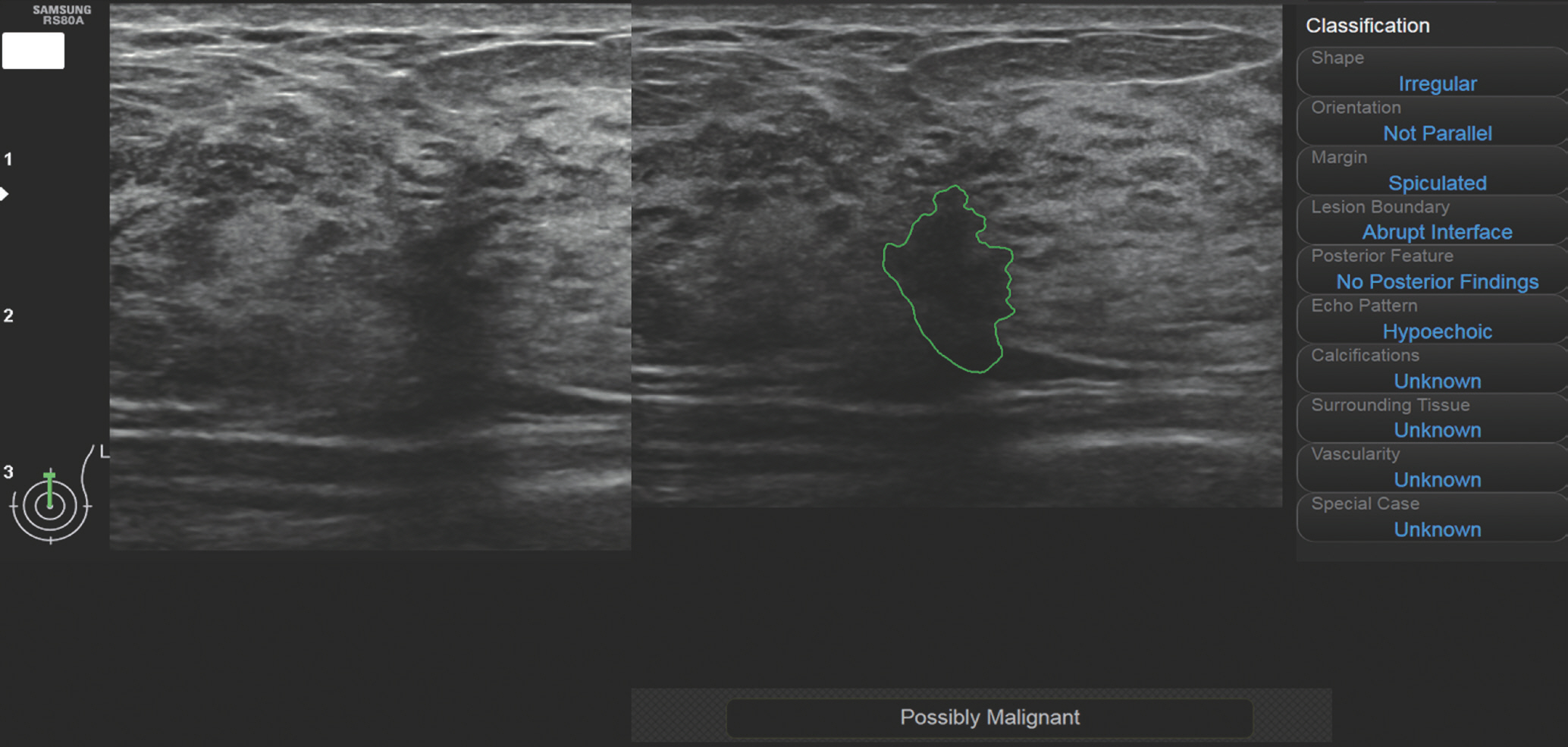
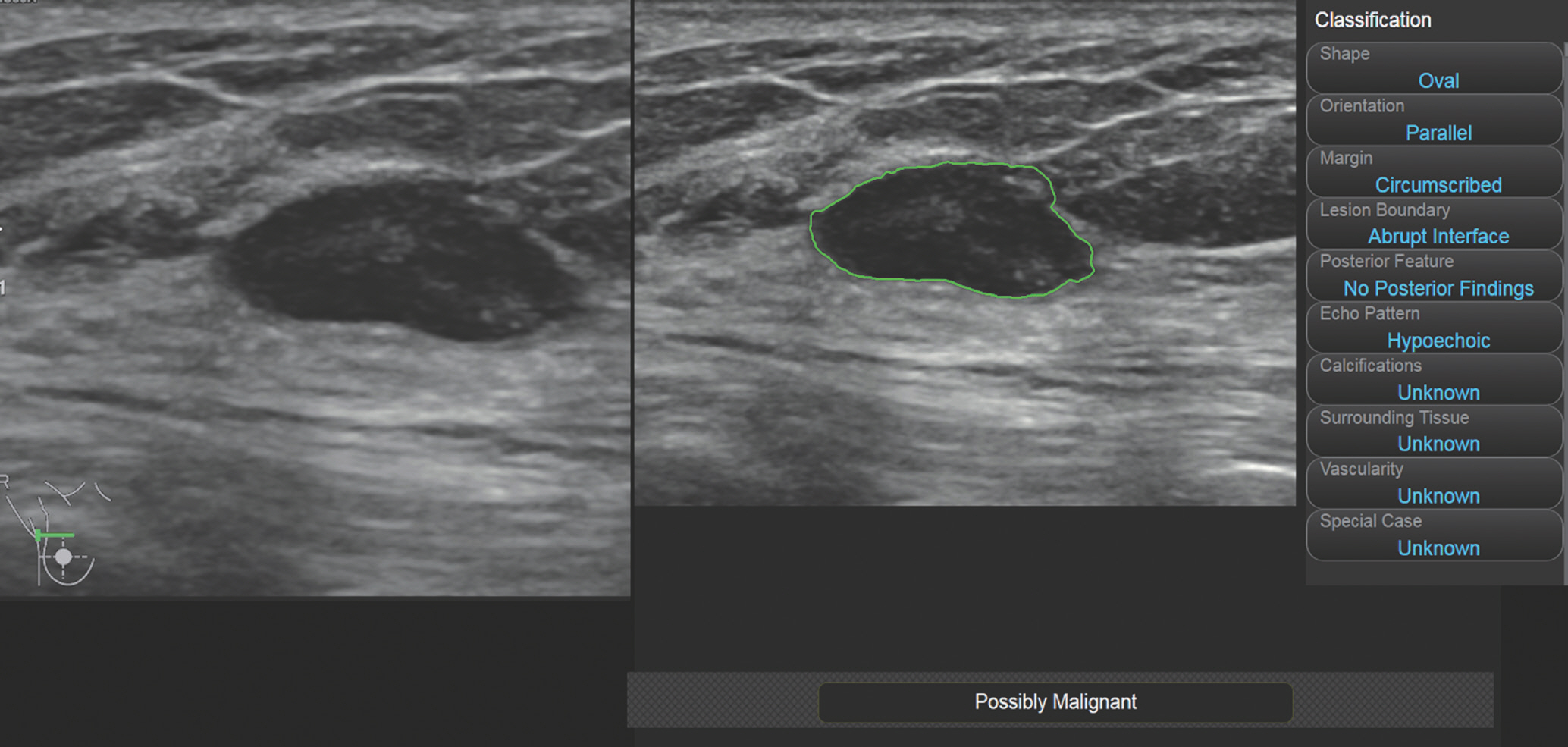
The accuracy, sensitivity, specificity, PPV, and NPV of breast US-CAD were 80.3%, 83.3%, 79.8%, 37.7%, and 97.0%, respectively. There were 8 false negative lesions that were oval in shape and in parallel orientation. There were 66 false positive lesions. The greatest number of errors entailed inappropriate demarcation due to heterogeneous echogenicity, etc. The second exhibited suspicious features with good demarcation and description but were confirmed as benign histologically. The third entailed a benign lesion with suspicious features, such as abscesses. The smallest portion with good demarcations and descriptions indicating benign status exhibited possible malignancy as a final conclusion.
CONCLUSION
Breast US-CAD is expected to be helpful in avoiding unnecessary biopsies due to its high NPV. Therefore, operators need to know the characteristics of lesions prone to misinterpretation.
MeSH Terms
Figure
Reference
-
1.Wang X., Guo Y., Wang Y. Automatic detection of regions of interest in breast ultrasound images based on local phase information. Biomed Mater Eng. 2015. 26(Suppl 1):S1265-S1273.
Article2.Jung KW., Won YJ., Oh CM., Kong HJ., Lee DH., Lee KH. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2014. Cancer Res Treat. 2017. 49:292–305.
Article3.Chabi ML., Borget I., Ardiles R., Aboud G., Boussouar S., Vilar V, et al. Evaluation of the accuracy of a computer-aided diagnosis (CAD) system in breast ultrasound according to the radiologist's experience. Acad Radiol. 2012. 19:311–319.
Article4.Kim K., Song MK., Kim EK., Yoon JH. Clinical application of S-Detect to breast masses on ultrasonography: a study evaluating the diagnostic performance and agreement with a dedicated breast radiologist. Ultrasonography. 2017. 36:3–9.
Article5.Chen DR., Chien CL., Kuo YF. Computer-aided assessment of tumor grade for breast cancer in ultrasound images. Comput Math Methods Med. 2015. 2015:914091.
Article6.Moon WK., Huang YS., Lo CM., Huang CS., Bae MS., Kim WH, et al. Computer-aided diagnosis for distinguishing between triple-negative breast cancer and fibroadenomas based on ultrasound texture features. Med Phys. 2015. 42:3024–3035.
Article7.Song SE., Seo BK., Cho KR., Woo OH., Son GS., Kim C, et al. Computer-aided detection (CAD) system for breast MRI in assessment of local tumor extent, nodal status, and multifo-cality of invasive breast cancers: preliminary study. Cancer Imaging. 2015. 15:1.
Article8.Shan J., Alam SK., Garra B., Zhang Y., Ahmed T. Computer-aided diagnosis for breast ultrasound using computerized BI-RADS features and machine learning methods. Ultrasound Med Biol. 2016. 42:980–988.
Article9.Cho E., Kim EK., Song MK., Yoon JH. Application of computer-aided diagnosis on breast ultrasonography: evaluation of diagnostic performances and agreement of radiologists according to different levels of experience. J Ultrasound Med. 2018. 37:209–216.
Article10.Choi JH., Kang BJ., Baek JE., Lee HS., Kim SH. Application of computer-aided diagnosis in breast ultrasound interpretation: improvements in diagnostic performance according to reader experience. Ultrasonography. 2017. 37:217–225.
Article11.Lee SE., Moon JE., Rho YH., Kim EK., Yoon JH. Which supplementary imaging modality should be used for breast ultrasonography? Comparison of the diagnostic performance of elastography and computer-aided diagnosis. Ultrasonography. 2017. 36:153–159.
Article12.Wang Y., Jiang S., Wang H., Guo YH., Liu B., Hou Y, et al. CAD algorithms for solid breast masses discrimination: evaluation of the accuracy and interobserver variability. Ultrasound Med Biol. 2010. 36:1273–1281.
Article13.Dromain C., Boyer B., Ferré R., Canale S., Delaloge S., Balleygui-er C. Computed-aided diagnosis (CAD) in the detection of breast cancer. Eur J Radiol. 2013. 82:417–423.
Article14.Landis JR., Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33:159-174.
Article15.Tan T., Platel B., Twellmann T., van Schie G., Mus R., Grivegnée A, et al. Evaluation of the effect of computer-aided classification of benign and malignant lesions on reader performance in automated three-dimensional breast ultrasound. Acad Radiol. 2013. 20:1381–1388.16.Lehman CD., Wellman RD., Buist DS., Kerlikowske K., Tosteson AN., Miglioretti DL. Diagnostic accuracy of digital screening mammography with and without computer-aided detection. JAMA Intern Med. 2015. 175:1828–1837.
Article17.Sahiner B., Chan HP., Roubidoux MA., Hadjiiski LM., Helvie MA., Paramagul C, et al. Malignant and benign breast masses on 3D US volumetric images: effect of computer-aided diagnosis on radiologist accuracy. Radiology. 2007. 242:716–724.
Article18.Yoo JL., Woo OH., Kim YK., Cho KR., Yong HS., Seo BK, et al. Can MR imaging contribute in characterizing well-circumscribed breast carcinomas? Radiographics. 2010. 30:1689–1702.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Artificial intelligence in breast ultrasound: application in clinical practice
- Evaluation of Computer Aided Diagnosis (CAD) in the Interpretation of Mass Lesions seen on Breast Sonography
- Imaging Findings of Missed Breast Cancer: Retrospective Analysis
- Digital Mammography
- Computer-Aided Diagnosis in Chest CT