J Korean Neurosurg Soc.
2016 Nov;59(6):577-583. 10.3340/jkns.2016.59.6.577.
Parasellar Extension Grades and Surgical Extent in Endoscopic Endonasal Transsphenoidal Surgery for Pituitary Adenomas : A Single Surgeon's Consecutive Series with the Aspects of Reliability and Clinical Validity
- Affiliations
-
- 1Department of Neurosurgery, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea. hongyk@catholic.ac.kr
- 2Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- 3Department of Otorhinolaryngology, Seoul St. Mary's Hospital, The Catholic University of Korea, Seoul, Korea.
- KMID: 2417339
- DOI: http://doi.org/10.3340/jkns.2016.59.6.577
Abstract
OBJECTIVE
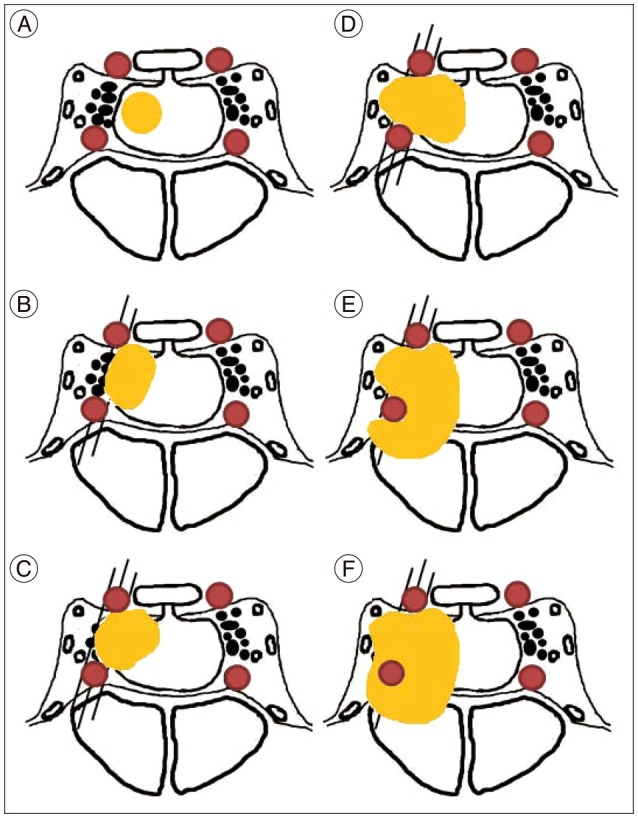
The inter-rater reliability of the modified Knosp's classification was measured before the analysis. The clinical validity of the parasellar extension grading system was evaluated by investigating the extents of resection and complication rates among the grades in the endoscopic endonasal transsphenoidal surgery (EETS) for pituitary adenomas.
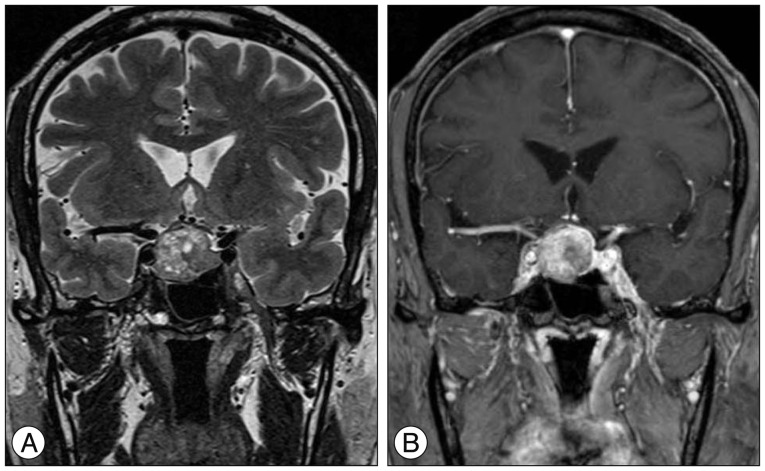
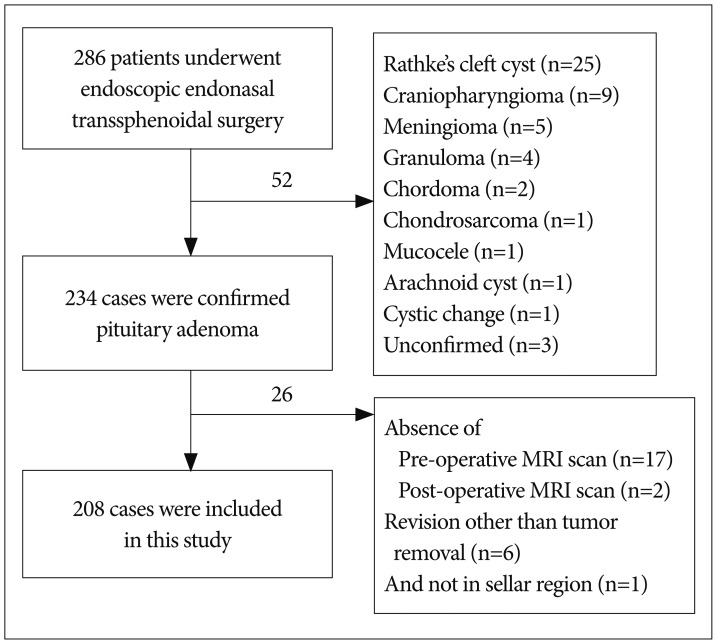
METHODS
From November 2008 to August 2015, of the 286 patients who underwent EETS by the senior author, 208 were pituitary adenoma cases (146 non-functioning pituitary adenomas, 10 adrenocorticotropic hormone-secreting adenomas, 31 growth hormone-secreting adenomas, 17 prolactin-secreting adenomas, and 4 thyroid-stimulating hormone-secreting adenomas; 23 microadenomas, 174 macroadenomas, and 11 giant adenomas). Two neurosurgeons and a neuroradiologist independently measured the degree of parasellar extension on the preoperative sellar MRI according to the modified Knosp's classification. Inter-rater reliability was statistically assessed by measuring the intraclass correlation coefficient. The extents of resection were evaluated by comparison of the pre- and post-operative MR images; the neurovascular complications were assessed by reviewing the patients' medical records. The extent of resection was measured in each parasellar extension grade; thereafter, their statistical differences were calculated.
RESULTS
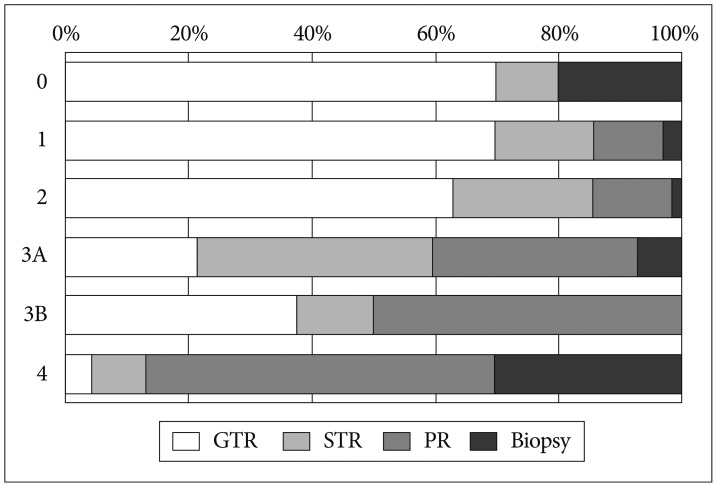
The intraclass correlation coefficient value of reliability across the three raters amounted to 0.862. The gross total removal (GTR) rates achieved in each grade were 70.0, 69.8, 62.9, 21.4, 37.5, and 4.3% in Grades 0, 1, 2, 3A, 3B, and 4, respectively. A significant difference in the extent of resection was observed only between Grades 2 and 3A. In addition, significantly higher complication rates were observed in the groups above Grade 3A.
CONCLUSION
Although the modified Knosp's classification system appears to be complex, its inter-rater reliability proves to be excellent. Regarding the clinical validity of the parasellar extension grading system, Grades 3A, 3B, and 4 have a negative predictive value for the GTR rate, with higher complication rates.
Keyword
MeSH Terms
Figure
Reference
-
1. Agrawal A, Cincu R, Goel A. Current concepts and controversies in the management of non-functioning giant pituitary macroadenomas. Clin Neurol Neurosurg. 2007; 109:645–650. PMID: 17686573.
Article2. Beardsley C, Egerton T, Skinner B. Test-re-test reliability and inter-rater reliability of a digital pelvic inclinometer in young, healthy males and females. PeerJ. 2016; 4:e1881. PMID: 27069812.
Article3. Burke SM, Hwang SW, Mehan WA Jr, Bedi HS, Ogbuji R, Riesenburger RI. Reliability of the modified Tufts Lumbar Degenerative Disc Classification between neurosurgeons and neuroradiologists. J Clin Neurosci. 2016; 29:111–116. PMID: 27021223.
Article4. Casanueva FF, Molitch ME, Schlechte JA, Abs R, Bonert V, Bronstein MD, et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin Endocrinol (Oxf). 2006; 65:265–273. PMID: 16886971.
Article5. Chang EF, Zada G, Kim S, Lamborn KR, Quinones-Hinojosa A, Tyrrell JB, et al. Long-term recurrence and mortality after surgery and adjuvant radiotherapy for nonfunctional pituitary adenomas. J Neurosurg. 2008; 108:736–745. PMID: 18377253.
Article6. Cunningham S. Inter-rater reliability and validity of the screenassist lumbar questionnaire : a pilot study. J Man Manip Ther. 2015; 23:254–263. PMID: 26952154.
Article7. de Divitiis E, Laws ER, Giani U, Iuliano SL, de Divitiis O, Apuzzo ML. The current status of endoscopy in transsphenoidal surgery : an international survey. World Neurosurg. 2015; 83:447–454. PMID: 25535063.
Article8. Dehdashti AR, Ganna A, Karabatsou K, Gentili F. Pure endoscopic endonasal approach for pituitary adenomas : early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery. 2008; 62:1006–1015. discussion 1015-1017. PMID: 18580798.
Article9. Dusick JR, Esposito F, Malkasian D, Kelly DF. Avoidance of carotid artery injuries in transsphenoidal surgery with the Doppler probe and micro-hook blades. Neurosurgery. 2007; 60(4 Suppl 2):322–328. discussion 328-329. PMID: 17415170.
Article10. Ferreli F, Turri-Zanoni M, Canevari FR, Battaglia P, Bignami M, Castelnuovo P, et al. Endoscopic endonasal management of non-functioning pituitary adenomas with cavernous sinus invasion : a 10- year experience. Rhinology. 2015; 53:308–316. PMID: 26301431.
Article11. Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. ed 3. Hoboken, NJ: John Wiley & Sons;2004. p. 598–626.12. Hardy J, Vezina JL. Transsphenoidal neurosurgery of intracranial neoplasm. Adv Neurol. 1976; 15:261–273. PMID: 945663.13. Ho RW, Huang HM, Ho JT. The influence of pituitary adenoma size on vision and visual outcomes after trans-sphenoidal adenectomy : a report of 78 cases. J Korean Neurosurg Soc. 2015; 57:23–31. PMID: 25674340.
Article14. Hwang JM, Kim YH, Kim JW, Kim DG, Jung HW, Chung YS. Feasibility of endoscopic endonasal approach for recurrent pituitary adenomas after microscopic trans-sphenoidal approach. J Korean Neurosurg Soc. 2013; 54:317–322. PMID: 24294455.
Article15. Jung KW, Ha J, Lee SH, Won YJ, Yoo H. An updated nationwide epidemiology of primary brain tumors in republic of Korea. Brain Tumor Res Treat. 2013; 1:16–23. PMID: 24904884.
Article16. Juraschka K, Khan OH, Godoy BL, Monsalves E, Kilian A, Krischek B, et al. Endoscopic endonasal transsphenoidal approach to large and giant pituitary adenomas : institutional experience and predictors of extent of resection. J Neurosurg. 2014; 121:75–83.
Article17. Kim BY, Shin JH, Kang SG, Kim SW, Hong YK, Jeun SS, et al. Bilateral modified nasoseptal "rescue" flaps in the endoscopic endonasal transsphenoidal approach. Laryngoscope. 2013; 123:2605–2609. PMID: 23553463.
Article18. Knosp E, Steiner E, Kitz K, Matula C. Pituitary adenomas with invasion of the cavernous sinus space : a magnetic resonance imaging classification compared with surgical findings. Neurosurgery. 1993; 33:610–617. discussion 617-618. PMID: 8232800.
Article19. Magro E, Graillon T, Lassave J, Castinetti F, Boissonneau S, Tabouret E, et al. Complications related to the endoscopic endonasal transsphenoidal approach for nonfunctioning pituitary macroadenomas in 300 consecutive patients. World Neurosurg. 2016; 89:442–453. PMID: 26902781.
Article20. Mazur MD, Taussky P, Shah LM, Winegar B, Park MS. Inter-rater reliability of published flow diversion occlusion scales. J Neurointerv Surg. 2016; 1. 20. DOI: 10.1136/neurintsurg-2015-012193. [Epub ahead of print].
Article21. Micko AS, Wöhrer A, Wolfsberger S, Knosp E. Invasion of the cavernous sinus space in pituitary adenomas : endoscopic verification and its correlation with an MRI-based classification. J Neurosurg. 2015; 122:803–811. PMID: 25658782.
Article22. Mortini P. Cons : endoscopic endonasal transsphenoidal pituitary surgery is not superior to microscopic transsphenoidal surgery for pituitary adenomas. Endocrine. 2014; 47:415–420. PMID: 25081297.
Article23. Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, et al. CBTRUS statistical report : primary brain and central nervous system tumors diagnosed in the United States in 2007-2011. Neuro Oncol. 16(Suppl 4):2014; iv1–iv63. PMID: 25304271.24. Park JH, Choi JH, Kim YI, Kim SW, Hong YK. Modified graded repair of cerebrospinal fluid leaks in endoscopic endonasal transsphenoidal surgery. J Korean Neurosurg Soc. 2015; 58:36–42. PMID: 26279811.
Article25. van Lummel RC, Walgaard S, Hobert MA, Maetzler W, van Dieën JH, Galindo-Garre F, et al. Intra-rater, inter-rater and test-retest reliability of an instrumented timed up and go (iTUG) test in patients with Parkinson's disease. PLoS One. 2016; 11:e0151881. PMID: 26999051.
Article26. Zaidi HA, Awad AW, Bohl MA, Chapple K, Knecht L, Jahnke H, et al. Comparison of outcomes between a less experienced surgeon using a fully endoscopic technique and a very experienced surgeon using a microscopic transsphenoidal technique for pituitary adenoma. J Neurosurg. 2016; 124:596–604. PMID: 26473774.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Deliberate Two-Staged Endoscopic Endonasal Transsphenoidal Surgery in Large Pituitary Adenomas
- Endoscopic Endonasal Surgery for Pituitary Adenoma
- Endoscopic Endonasal Transsphenoidal Pituitary Tumor Surgery: An Early Experience
- Endocrine Outcome of Endoscopic Endonasal Transsphenoidal Surgery in Functioning Pituitary Adenomas
- Surgical Experiences of Three Cases of Giant Pituitary Adenoma