J Clin Neurol.
2018 Jul;14(3):265-274. 10.3988/jcn.2018.14.3.265.
Swallowing and Aspiration Risk: A Critical Review of Non Instrumental Bedside Screening Tests
- Affiliations
-
- 1Department of Internal Medicine, School of Medicine, University of Ioannina, Ioannina, Greece. info@virvidaki.gr
- 2Department of Speech and Language Therapy, Technological Educational Institute of Epirus, Ioannina, Greece.
- 3Department of Neurology, School of Medicine, University of Ioannina, Ioannina, Greece.
- KMID: 2415040
- DOI: http://doi.org/10.3988/jcn.2018.14.3.265
Abstract
- BACKGROUND AND PURPOSE
The presence of dysphagia and aspiration in stroke patients is associated with increased mortality and morbidity. Early recognition and management of these two conditions via reliable, minimally invasive bedside procedures before complications arise remains challenging in everyday clinical practice. This study reviews the available bedside screening tools for detecting swallowing status and aspiration risk in acute stroke by qualitatively observing reference population study design, clinical flexibility, reliability and applicability to acute-care settings.
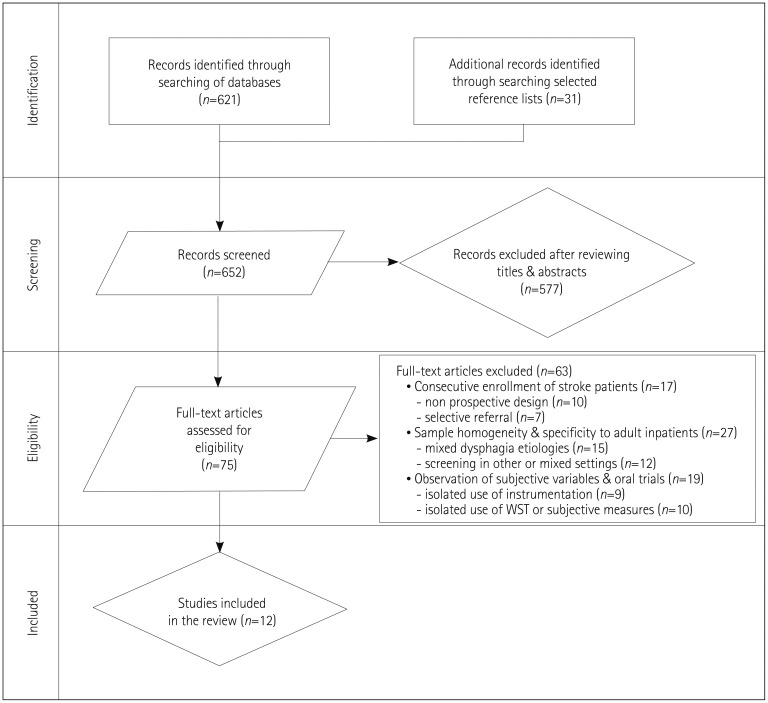
METHODS
The primary search was conducted using the PubMed, Embase, and Cochrane Library databases. The search was limited to papers on humans written in English and published from 1991 to 2016. Eligibility criteria included the consecutive enrollment of acute-stroke inpatients and the development of a protocol for screening aspiration risk during oral feeding in this population.
RESULTS
Of the 652 sources identified, 75 articles were reviewed in full however, only 12 fulfilled the selection criteria. Notable deficiencies in most of the bedside screening protocols included poor methodological designs and inadequate predictive values for aspiration risk which render clinicians to be more conservative in making dietary recommendations.
CONCLUSIONS
The literature is dense with screening methods for assessing the presence of dysphagia but with low predictive value for aspiration risk after acute stroke. A standard, practical, and cost-effective screening tool that can be applied at the bedside and interpreted by a wide range of hospital personnel remains to be developed. This need is highlighted in settings where neither trained personnel in evaluating dysphagia nor clinical instrumentation procedures are available.
MeSH Terms
Figure
Reference
-
1. Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalized patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg. 2010; 136:784–789. PMID: 20713754.2. Armstrong JR, Mosher BD. Aspiration pneumonia after stroke: intervention and prevention. Neurohospitalist. 2011; 1:85–93. PMID: 23983842.3. Goldstein LB, Bushnell CD, Adams RJ, Appel LJ, Braun LT, Chaturvedi S, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:517–584. PMID: 21127304.
Article4. Camm AJ, Lobban T, Knight E, Wait S, Harding E. The Route Map for Change & the European Atlas on the Prevention of AF-Related Stroke. London: The Health Policy Partnership;2014.5. OECD/EU. Health at a Glance: Europe 2010. Paris: OECD Publishing;2010.6. Health and Social Care Information Centre (GB). Statistics on Smoking, England: 2016. London: Health and Social Care Information Centre;2016.7. Flowers HL, Silver FL, Fang J, Rochon E, Martino R. The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke. J Commun Disord. 2013; 46:238–248. PMID: 23642855.
Article8. Wieseke A, Bantz D, Siktberg L, Dillard N. Assessment and early diagnosis of dysphagia. Geriatr Nurs. 2008; 29:376–383. PMID: 19064135.
Article9. Ickenstein GW, Höhlig C, Prosiegel M, Koch H, Dziewas R, Bodechtel U, et al. Prediction of outcome in neurogenic oropharyngeal dysphagia within 72 hours of acute stroke. J Stroke Cerebrovasc Dis. 2012; 21:569–576. PMID: 21683618.
Article10. Smithard DG, O'Neill PA, England RE, Park CL, Wyatt R, Martin DF, et al. The natural history of dysphagia following a stroke. Dysphagia. 1997; 12:188–193. PMID: 9294937.
Article11. Okubo PC, Fábio SR, Domenis DR, Takayanagui OM. Using the National Institute of Health Stroke Scale to predict dysphagia in acute ischemic stroke. Cerebrovasc Dis. 2012; 33:501–507. PMID: 22538772.
Article12. Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke. 1999; 30:744–748. PMID: 10187872.13. Wirth R, Smoliner C, Jäger M, Warnecke T, Leischker AH, Dziewas R. DGEM Steering Committee. Guideline clinical nutrition in patients with stroke. Exp Transl Stroke Med. 2013; 5:14. PMID: 24289189.
Article14. Shaker R, Geenen JE. Management of dysphagia in stroke patients. Gastroenterol Hepatol (N Y). 2011; 7:308–332. PMID: 21857832.15. Gosney MA, Martin MV, Wright AE, Gallagher M. Enterobacter sakazakii in the mouths of stroke patients and its association with aspiration pneumonia. Eur J Intern Med. 2006; 17:185–188. PMID: 16618451.
Article16. Finlayson O, Kapral M, Hall R, Asllani E, Selchen D, Saposnik G. Canadian Stroke Network. Stroke Outcome Research Canada (SORCan) Working Group. Risk factors, inpatient care, and outcomes of pneumonia after ischemic stroke. Neurology. 2011; 77:1338–1345. PMID: 21940613.
Article17. Finestone HM, Greene-Finestone LS, Wilson ES, Teasell RW. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictor. Arch Phys Med Rehabil. 1995; 76:310–316. PMID: 7717830.18. Foley NC, Salter KL, Robertson J, Teasell RW, Woodbury MG. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke. 2009; 40:e66–e74. PMID: 19164799.
Article19. Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008; 65:39–43. PMID: 18195138.
Article20. Kammersgaard LP, Jørgensen HS, Rungby JA, Reith J, Nakayama H, Weber UJ, et al. Admission body temperature predicts long-term mortality after acute stroke: the Copenhagen Stroke Study. Stroke. 2002; 33:1759–1762. PMID: 12105348.21. Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2197–2223. PMID: 23245608.22. National Institute for Health and Care Excellence (GB). Stroke and transient ischaemic attack in over 16s: diagnosis and initial management [Internet]. London: National Institute for Health and Care Excellence;2008. cited 2017 Aug 26. Available from: http://nice.org.uk/guidance/cg68.23. Intercollegiate Stroke Working Party (GB). National Clinical Guideline for Stroke. 4th ed. London: Royal College of Physicians;2012.24. Boaden E, Doran D, Burnell J, Clegg A, Dey P, Hurley M, et al. Screening for aspiration risk associated with dysphagia in acute stroke (diagnostic test accuracy protocol). Cochrane Database Syst Rev. 2017; CD012679.
Article25. Ramsey DJ, Smithard DG, Kalra L. Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke. 2003; 34:1252–1257. PMID: 12677020.
Article26. Schultheiss C, Nusser-Müller-Busch R, Seidl RO. The semisolid bolus swallow test for clinical diagnosis of oropharyngeal dysphagia: a prospective randomised study. Eur Arch Otorhinolaryngol. 2011; 268:1837–1844. PMID: 21607581.
Article27. Donovan NJ, Daniels SK, Edmiaston J, Weinhardt J, Summers D, Mitchell PH. American Heart Association Council on Cardiovascular Nursing and Stroke Council. Dysphagia screening: state of the art: invitational conference proceeding from the State-of-the-Art Nursing Symposium, International Stroke Conference 2012. Stroke. 2013; 44:e24–e31. PMID: 23412377.28. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011; 155:529–536. PMID: 22007046.
Article29. Ramsey DJ, Smithard DG, Kalra L. Can pulse oximetry or a bedside swallowing assessment be used to detect aspiration after stroke? Stroke. 2006; 37:2984–2988. PMID: 17095740.
Article30. Turner-Lawrence DE, Peebles M, Price MF, Singh SJ, Asimos AW. A feasibility study of the sensitivity of emergency physician Dysphagia screening in acute stroke patients. Ann Emerg Med. 2009; 54:344–348. PMID: 19362752.
Article31. Smith HA, Lee SH, O'Neill PA, Connolly MJ. The combination of bedside swallowing assessment and oxygen saturation monitoring of swallowing in acute stroke: a safe and humane screening tool. Age Ageing. 2000; 29:495–499. PMID: 11191240.
Article32. Trapl M, Enderle P, Nowotny M, Teuschl Y, Matz K, Dachenhausen A, et al. Dysphagia bedside screening for acute-stroke patients: the Gugging Swallowing Screen. Stroke. 2007; 38:2948–2952. PMID: 17885261.33. Edmiaston J, Connor LT, Steger-May K, Ford AL. A simple bedside stroke dysphagia screen, validated against videofluoroscopy, detects dysphagia and aspiration with high sensitivity. J Stroke Cerebrovasc Dis. 2014; 23:712–716. PMID: 23910514.
Article34. Lim SH, Lieu PK, Phua SY, Seshadri R, Venketasubramanian SH, et al. Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia. 2001; 16:1–6. PMID: 11213241.
Article35. Leder SB, Espinosa JF. Aspiration risk after acute stroke: comparison of clinical examination and fiberoptic endoscopic evaluation of swallowing. Dysphagia. 2002; 17:214–218. PMID: 12140648.
Article36. Antonios N, Carnaby-Mann G, Crary M, Miller L, Hubbard H, Hood K, et al. Analysis of a physician tool for evaluating dysphagia on an inpatient stroke unit: the modified Mann Assessment of Swallowing Ability. J Stroke Cerebrovasc Dis. 2010; 19:49–57. PMID: 20123227.
Article37. Smithard DG, O'Neill PA, Park C, England R, Renwick DS, Wyatt R, et al. Can bedside assessment reliably exclude aspiration following acute stroke? Age Ageing. 1998; 27:99–106. PMID: 16296668.
Article38. Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL. Aspiration in patients with acute stroke. Arch Phys Med Rehabil. 1998; 79:14–19. PMID: 9440410.
Article39. McCullough GH, Rosenbek JC, Wertz RT, McCoy S, Mann G, McCullough K. Utility of clinical swallowing examination measures for detecting aspiration post-stroke. J Speech Lang Hear Res. 2005; 48:1280–1293. PMID: 16478371.
Article40. Nishiwaki K, Tsuji T, Liu M, Hase K, Tanaka N, Fujiwara T. Identification of a simple screening tool for dysphagia in patients with stroke using factor analysis of multiple dysphagia variables. J Rehabil Med. 2005; 37:247–251. PMID: 16024482.
Article41. Leigh JH, Lim JY, Han MK, Bae HJ, Kim WS, Paik NJ. A prospective comparison between bedside swallowing screening test and videofluoroscopic swallowing study in post-stroke dysphagia. Brain Neurorehabil. 2016; 9:e7.
Article42. Mann G. MASA: the Mann Assessment of Swallowing Ability. Clifton Park: Singular/Thomson Learning;2002.43. Martino R, Pron G, Diamant N. Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines. Dysphagia. 2000; 15:19–30. PMID: 10594255.
Article44. Hinchey JA, Shephard T, Furie K, Smith D, Wang D, Tonn S. Stroke Practice Improvement Network Investigators. Formal dysphagia screening protocols prevent pneumonia. Stroke. 2005; 36:1972–1976. PMID: 16109909.
Article45. Leder SB, Suiter DM, Green BG. Silent aspiration risk is volume-dependent. Dysphagia. 2011; 26:304–309. PMID: 21063732.
Article46. Parker C, Power M, Hamdy S, Bowen A, Tyrrell P, Thompson DG. Awareness of dysphagia by patients following stroke predicts swallowing performance. Dysphagia. 2004; 19:28–35. PMID: 14745643.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Utility of the Bedside Swallowing Evaluations for Dysphagia
- Risk Factors and Assessment of Aspiration
- Instrumental Assessment of Swallowing
- A Prospective Comparison between Bedside Swallowing Screening Test and Videofluoroscopic Swallowing Study in Post-Stroke Dysphagia
- Comparison between Gugging Swallowing Screen and Other Dysphagia Screening Tests