J Gastric Cancer.
2018 Jun;18(2):172-181. 10.5230/jgc.2018.18.e18.
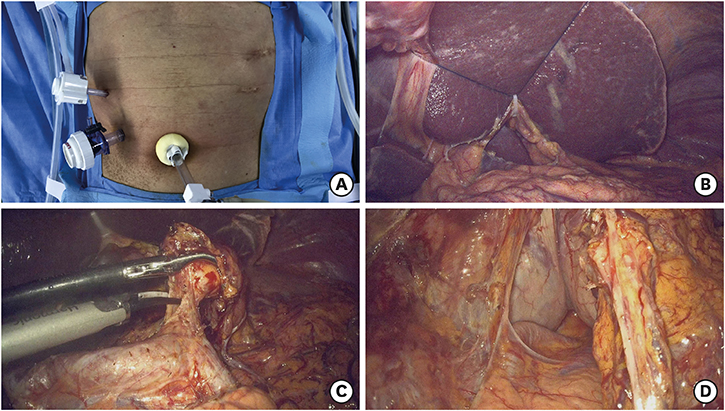
Transition from Conventional to Reduced-Port Laparoscopic Gastrectomy to Treat Gastric Carcinoma: a Single Surgeon's Experience from a Small-Volume Center
- Affiliations
-
- 1Division of Gastroenterologic Surgery, Department of Surgery, Chonnam National University Medical School, Gwangju, Korea. surgeonjeong@gmail.com
- KMID: 2414537
- DOI: http://doi.org/10.5230/jgc.2018.18.e18
Abstract
- PURPOSE
This study aimed to evaluate the surgical outcomes and investigate the feasibility of reduced-port laparoscopic gastrectomy using learning curve analysis in a small-volume center.
MATERIALS AND METHODS
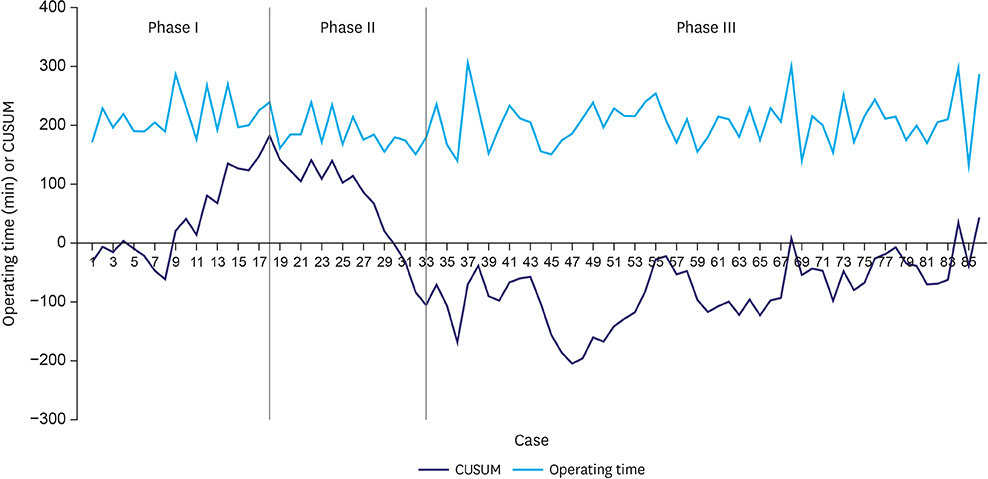
We reviewed 269 patients who underwent laparoscopic distal gastrectomy (LDG) for gastric carcinoma between 2012 and 2017. Among them, 159 patients underwent reduced-port laparoscopic gastrectomy. The cumulative sum technique was used for quantitative assessment of the learning curve.
RESULTS
There were no statistically significant differences in the baseline characteristics of patients who underwent conventional and reduced-port LDG, and the operative time did not significantly differ between the groups. However, the amount of intraoperative bleeding was significantly lower in the reduced-port laparoscopic gastrectomy group (56.3 vs. 48.2 mL; P < 0.001). There were no significant differences between the groups in terms of the first flatus time or length of hospital stay. Neither the incidence nor the severity of the complications significantly differed between the groups. The slope of the cumulative sum curve indicates the trend of learning performance. After 33 operations, the slope gently stabilized, which was regarded as the breakpoint of the learning curve.
CONCLUSIONS
The surgical outcomes of reduced-port laparoscopic gastrectomy were comparable to those of conventional laparoscopic gastrectomy, suggesting that transition from conventional to reduced-port laparoscopic gastrectomy is feasible and safe, with a relatively short learning curve, in a small-volume center.
Keyword
MeSH Terms
Figure
Reference
-
1. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994; 4:146–148.2. Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011; 11:69–77.
Article3. Viñuela EF, Gonen M, Brennan MF, Coit DG, Strong VE. Laparoscopic versus open distal gastrectomy for gastric cancer: a meta-analysis of randomized controlled trials and high-quality nonrandomized studies. Ann Surg. 2012; 255:446–456.4. Matsuda T, Ogura K, Uchida J, Fujita I, Terachi T, Yoshida O. Smaller ports result in shorter convalescence after laparoscopic varicocelectomy. J Urol. 1995; 153:1175–1177.
Article5. Usui S, Tashiro M, Haruki S, Matsumoto A. Triple-incision laparoscopic distal gastrectomy for the resection of gastric cancer: comparison with conventional laparoscopy-assisted distal gastrectomy. Asian J Endosc Surg. 2014; 7:197–205.
Article6. Kunisaki C, Makino H, Yamaguchi N, Izumisawa Y, Miyamato H, Sato K, et al. Surgical advantages of reduced-port laparoscopic gastrectomy in gastric cancer. Surg Endosc. 2016; 30:5520–5528.
Article7. Kawamura H, Tanioka T, Kuji M, Tahara M, Takahashi M. The initial experience of dual port laparoscopy-assisted total gastrectomy as a reduced port surgery for total gastrectomy. Gastric Cancer. 2013; 16:602–608.
Article8. Jeong O, Park YK, Ryu SY. Early experience of duet laparoscopic distal gastrectomy (duet-LDG) using three abdominal ports for gastric carcinoma: surgical technique and comparison with conventional laparoscopic distal gastrectomy. Surg Endosc. 2016; 30:3559–3566.
Article9. Kim SM, Ha MH, Seo JE, Kim JE, Choi MG, Sohn TS, et al. Comparison of reduced port totally laparoscopic distal gastrectomy (duet TLDG) and conventional laparoscopic-assisted distal gastrectomy. Ann Surg Oncol. 2015; 22:2567–2572.
Article10. Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc. 2011; 25:2400–2404.
Article11. Ahn SH, Park DJ, Son SY, Lee CM, Kim HH. Single-incision laparoscopic total gastrectomy with D1+beta lymph node dissection for proximal early gastric cancer. Gastric Cancer. 2014; 17:392–396.
Article12. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.14. Sobin LH, Gospodarowicz MK, Wittekind C. TNM Classification of Malignant Tumours. 7th ed. Hoboken (NJ): Wiley-Blackwell;2010.15. Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011; 25:855–860.
Article16. Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol. 2005; 11:7508–7511.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Issues in Reduced-Port Gastrectomy: A Comprehensive Review
- Single Port Gastrectomy for Gastric Cancer
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case
- Comparing the surgical outcomes of dual-port laparoscopic distal gastrectomy and three-port laparoscopic distal gastrectomy for gastric cancer
- Evaluation of Reduced Port Laparoscopic Distal Gastrectomy Performed by a Novice Surgeon