J Gastric Cancer.
2018 Jun;18(2):161-171. 10.5230/jgc.2018.18.e19.
Assessment of the Completeness of Lymph Node Dissection Using Near-infrared Imaging with Indocyanine Green in Laparoscopic Gastrectomy for Gastric Cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. wisehearted@gmail.com
- 2Department of Surgery, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 3Cancer Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2414536
- DOI: http://doi.org/10.5230/jgc.2018.18.e19
Abstract
- PURPOSE
This study assessed the feasibility of near-infrared (NIR) imaging with indocyanine green (ICG) in investigating the completeness of laparoscopic lymph node (LN) dissection for gastric cancer.
MATERIALS AND METHODS
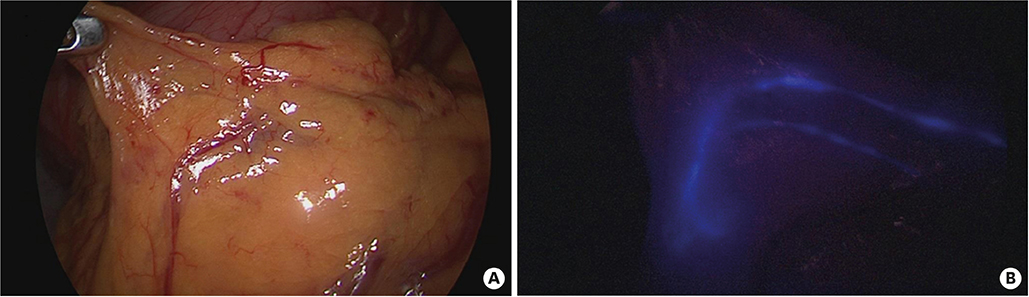
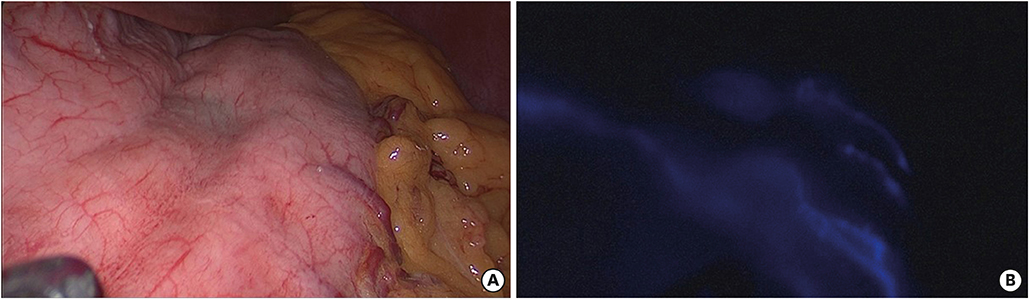
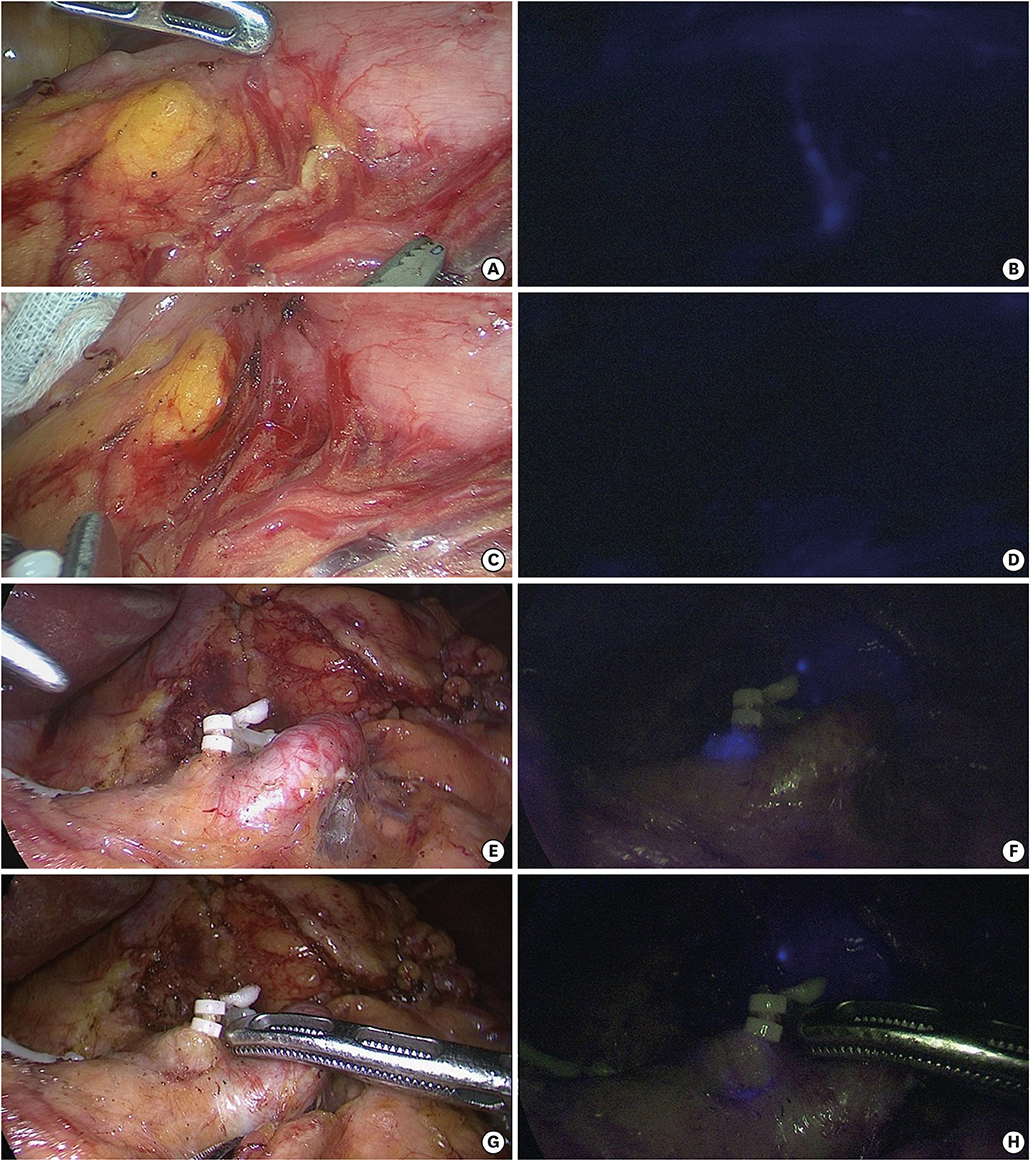
Patients scheduled for laparoscopic gastrectomy for treating gastric cancer were enrolled in the study. After intraoperative submucosal ICG injection (0.05 mg/mL), LN dissection was performed under conventional laparoscopic light. After dissection, the LN stations of interest were examined under the NIR mode to locate any extra ICG-stained (E) tissues, which were excised and sent for pathologic confirmation. This technique was tested in 2 steps: infra-pyloric LN dissection (step 1) and review of all stations after proper radical node dissection (step 2).
RESULTS
In step 1, 15 patients who underwent laparoscopic pylorus-preserving gastrectomy (LPPG) and 15 patients who underwent laparoscopic distal gastrectomy (LDG) were examined. Seven and 2 E-tissues were obtained during LPPG and LDG, respectively. From the retrieved E-tissues, 1 and 0 tissue obtained during LPPG and LDG, respectively, was confirmed as LN. In step 2, 20 patients were enrolled (13 D1+ dissection and 7 D2 dissection). Six E-tissues were retrieved from 5 patients, and 1 tissue was confirmed as LN in the pathologic review. Overall, 15 E-tissues were detected and removed, and 2 tissues were confirmed as LNs in the pathologic review. Both nodes were from LN station #6, with 1 case each in the LDG and LPPG groups.
CONCLUSIONS
NIR imaging may provide additional node detection during laparoscopic LN dissection for gastric cancer, especially in the infra-pyloric area.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim JP, Lee JH, Kim SJ, Yu HJ, Yang HK. Clinicopathologic characteristics and prognostic factors in 10 783 patients with gastric cancer. Gastric Cancer. 1998; 1:125–133.
Article2. Degiuli M, Sasako M, Ponti A, Vendrame A, Tomatis M, Mazza C, et al. Randomized clinical trial comparing survival after D1 or D2 gastrectomy for gastric cancer. Br J Surg. 2014; 101:23–31.3. Tokunaga M, Ohyama S, Hiki N, Fukunaga T, Yamada K, Sano T, et al. Investigation of the lymphatic stream of the stomach in gastric cancer with solitary lymph node metastasis. World J Surg. 2009; 33:1235–1239.
Article4. Kong SH, Noh YW, Suh YS, Park HS, Lee HJ, Kang KW, et al. Evaluation of the novel near-infrared fluorescence tracers pullulan polymer nanogel and indocyanine green/γ-glutamic acid complex for sentinel lymph node navigation surgery in large animal models. Gastric Cancer. 2015; 18:55–64.
Article5. Shinohara H, Kurahashi Y, Kanaya S, Haruta S, Ueno M, Udagawa H, et al. Topographic anatomy and laparoscopic technique for dissection of no. 6 infrapyloric lymph nodes in gastric cancer surgery. Gastric Cancer. 2013; 16:615–620.
Article6. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011; 14:113–123.7. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112.8. Sasako M, McCulloch P, Kinoshita T, Maruyama K. New method to evaluate the therapeutic value of lymph node dissection for gastric cancer. Br J Surg. 1995; 82:346–351.
Article9. Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, et al. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg. 2014; 259:485–493.
Article10. Sawai K, Takahashi T, Fujioka T, Minato H, Taniguchi H, Yamaguchi T. Pylorus-preserving gastrectomy with radical lymph node dissection based on anatomical variations of the infrapyloric artery. Am J Surg. 1995; 170:285–288.
Article11. Kim M, Son SY, Cui LH, Shin HJ, Hur H, Han SU. Real-time vessel navigation using indocyanine green fluorescence during robotic or laparoscopic gastrectomy for gastric cancer. J Gastric Cancer. 2017; 17:145–153.
Article12. Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011; 45:626–629.
Article13. Miyashiro I, Hiratsuka M, Kishi K, Takachi K, Yano M, Takenaka A, et al. Intraoperative diagnosis using sentinel node biopsy with indocyanine green dye in gastric cancer surgery: an institutional trial by experienced surgeons. Ann Surg Oncol. 2013; 20:542–546.
Article14. Miyashiro I, Kishi K, Yano M, Tanaka K, Motoori M, Ohue M, et al. Laparoscopic detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging. Surg Endosc. 2011; 25:1672–1676.
Article15. Miwa K, Kinami S, Taniguchi K, Fushida S, Fujimura T, Nonomura A. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br J Surg. 2003; 90:178–182.
Article16. Ergina PL, Cook JA, Blazeby JM, Boutron I, Clavien PA, Reeves BC, et al. Challenges in evaluating surgical innovation. Lancet. 2009; 374:1097–1104.
Article17. McCulloch P, Altman DG, Campbell WB, Flum DR, Glasziou P, Marshall JC, et al. No surgical innovation without evaluation: the IDEAL recommendations. Lancet. 2009; 374:1105–1112.
Article18. Barkun JS, Aronson JK, Feldman LS, Maddern GJ, Strasberg SM, Altman DG, et al. Evaluation and stages of surgical innovations. Lancet. 2009; 374:1089–1096.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Near-Infrared Fluorescence Imaging with Indocyanine Green in Totally Laparoscopic Distal Gastrectomy
- Is Laparoscopic Approach Also Safe for the Treatment of Remnant Gastric Cancer?
- Alterations in portal vein confluence during gastric cancer surgery: two case reports
- Indocyanine green and near-infrared fluorescenceguided surgery for gastric cancer: a narrative review
- Gastric cancer in pregnancy: is laparoscopic gastrectomy with lymph node dissection feasible and safe?