Korean Circ J.
2018 Jun;48(6):447-462. 10.4070/kcj.2018.0078.
Revascularization for Left Main and Multivessel Coronary Artery Disease: Current Status and Future Prospects after the EXCEL and NOBLE Trials
- Affiliations
-
- 1Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, USA. holmes.david@mayo.edu
- KMID: 2412538
- DOI: http://doi.org/10.4070/kcj.2018.0078
Abstract
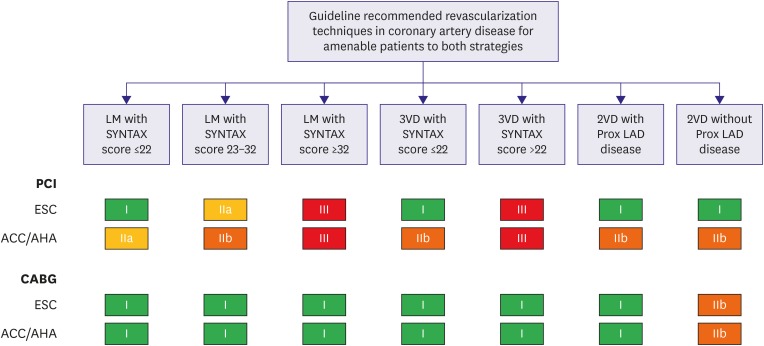
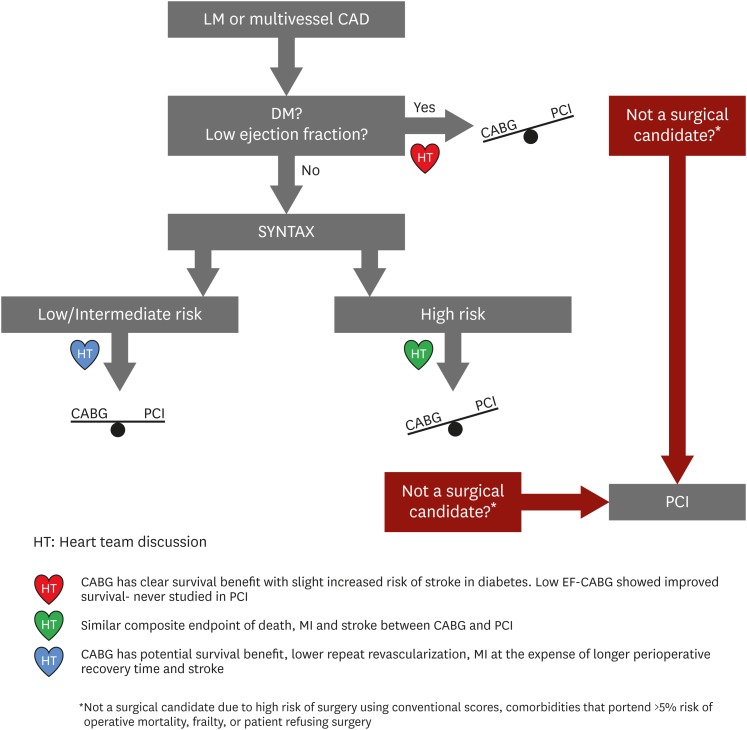
- Revascularization of severe left main and multivessel coronary artery disease has been shown to improve survival in both stable ischemic heart disease and acute coronary syndrome. While revascularization with coronary artery bypass surgery for these disease entities carries class I recommendation in most current guidelines, recent trials has shown potential comparable survival and cardiovascular outcomes between percutaneous and surgical interventions in patients with less complex coronary anatomy. Despite the conflicting results observed in the most recent left main revascularization trials, Everolimus-Eluting Stents or Bypass Surgery for Left Main Coronary Artery Disease (EXCEL) and Nordic-Baltic-British left main revascularization (NOBLE), both treatment strategies remain important for the management of left main disease (LMD) and multivessel disease (MVD) reflecting on the importance of heart team discussion. This review is focused on revascularization of LMD and MVD in patients who are not presenting with ST-segment elevation myocardial infarction, encompassing the evidence from historic and contemporary trials which shaped up current practices. This review discusses the heart team approach to guide decision making, including special populations that are not represented in clinical trials.
Keyword
MeSH Terms
Figure
Reference
-
1. Goetz RH, Rohman M, Haller JD, Dee R, Rosenak SS. Internal mammary-coronary artery anastomosis. A nonsuture method employing tantalum rings. J Thorac Cardiovasc Surg. 1961; 41:378–386. PMID: 13706288.2. Gruentzig A. Results from coronary angioplasty and implications for the future. Am Heart J. 1982; 103:779–783. PMID: 6461237.3. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007; 356:1503–1516. PMID: 17387127.4. Hueb W, Lopes NH, Gersh BJ, et al. Five-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2007; 115:1082–1089. PMID: 17339566.5. Velazquez EJ, Lee KL, Deja MA, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011; 364:1607–1616. PMID: 21463150.6. Velazquez EJ, Lee KL, Jones RH, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med. 2016; 374:1511–1520. PMID: 27040723.7. Yusuf S, Zucker D, Peduzzi P, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994; 344:563–570. PMID: 7914958.8. Kaiser GC, Davis KB, Fisher LD, et al. Survival following coronary artery bypass grafting in patients with severe angina pectoris (CASS). An observational study. J Thorac Cardiovasc Surg. 1985; 89:513–524. PMID: 3884909.9. Serruys PW, Ong AT, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005; 46:575–581. PMID: 16098418.10. Hueb W, Lopes N, Gersh BJ, et al. Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2010; 122:949–957. PMID: 20733102.11. Buszman PE, Buszman PP, Banasiewicz-Szkrobka I, et al. Left main stenting in comparison with surgical revascularization: 10-year outcomes of the (Left Main Coronary Artery Stenting) LE MANS Trial. JACC Cardiovasc Interv. 2016; 9:318–327. PMID: 26892080.12. Ahn JM, Roh JH, Kim YH, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease: 5-year outcomes of the PRECOMBAT study. J Am Coll Cardiol. 2015; 65:2198–2206. PMID: 25787197.13. Morice MC, Serruys PW, Kappetein AP, et al. Five-year outcomes in patients with left main disease treated with either percutaneous coronary intervention or coronary artery bypass grafting in the synergy between percutaneous coronary intervention with taxus and cardiac surgery trial. Circulation. 2014; 129:2388–2394. PMID: 24700706.14. Head SJ, Davierwala PM, Serruys PW, et al. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014; 35:2821–2830. PMID: 24849105.15. Stone GW, Sabik JF, Serruys PW, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016; 375:2223–2235. PMID: 27797291.16. Mäkikallio T, Holm NR, Lindsay M, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet. 2016; 388:2743–2752. PMID: 27810312.17. Ragosta M, Dee S, Sarembock IJ, Lipson LC, Gimple LW, Powers ER. Prevalence of unfavorable angiographic characteristics for percutaneous intervention in patients with unprotected left main coronary artery disease. Catheter Cardiovasc Interv. 2006; 68:357–362. PMID: 16892431.18. Bruschke AV, Proudfit WL, Sones FM Jr. Progress study of 590 consecutive nonsurgical cases of coronary disease followed 5–9 years. II. Ventriculographic and other correlations. Circulation. 1973; 47:1154–1163. PMID: 4709535.19. Park SJ, Kim YH, Park DW, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med. 2011; 364:1718–1727. PMID: 21463149.20. Taggart DP, Kaul S, Boden WE, et al. Revascularization for unprotected left main stem coronary artery stenosis stenting or surgery. J Am Coll Cardiol. 2008; 51:885–892. PMID: 18308155.21. Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009; 360:961–972. PMID: 19228612.22. Morice MC, Serruys PW, Kappetein AP, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010; 121:2645–2653. PMID: 20530001.23. Bangalore S, Kumar S, Fusaro M, et al. Short- and long-term outcomes with drug-eluting and bare-metal coronary stents: a mixed-treatment comparison analysis of 117 762 patient-years of follow-up from randomized trials. Circulation. 2012; 125:2873–2891. PMID: 22586281.24. Alazzoni A, Al-Saleh A, Jolly SS. Everolimus-eluting versus paclitaxel-eluting stents in percutaneous coronary intervention: meta-analysis of randomized trials. Thrombosis. 2012; 2012:126369. PMID: 22655192.25. Ye Y, Yang M, Zhang S, Zeng Y. Percutaneous coronary intervention in left main coronary artery disease with or without intravascular ultrasound: a meta-analysis. PLoS One. 2017; 12:e0179756. PMID: 28640875.26. Chen SL, Xu B, Han YL, et al. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013; 61:1482–1488. PMID: 23490040.27. Chen SL, Xu B, Han YL, et al. Clinical outcome after DK crush versus culotte stenting of distal left main bifurcation lesions: the 3-year follow-up results of the DKCRUSH-III study. JACC Cardiovasc Interv. 2015; 8:1335–1342. PMID: 26315736.28. Chen SL, Zhang JJ, Han Y, et al. Double kissing crush versus provisional stenting for left main distal bifurcation lesions: DKCRUSH-V randomized trial. J Am Coll Cardiol. 2017; 70:2605–2617. PMID: 29096915.29. Giacoppo D, Colleran R, Cassese S, et al. Percutaneous coronary intervention vs coronary artery bypass grafting in patients with left main coronary artery stenosis: a systematic review and meta-analysis. JAMA Cardiol. 2017; 2:1079–1088. PMID: 28903139.30. Capodanno D, Stone GW, Morice MC, Bass TA, Tamburino C. Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of randomized clinical data. J Am Coll Cardiol. 2011; 58:1426–1432. PMID: 21939824.31. Sos Investigators. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the Stent or Surgery trial): a randomised controlled trial. Lancet. 2002; 360:965–970. PMID: 12383664.32. Booth J, Clayton T, Pepper J, et al. Randomized, controlled trial of coronary artery bypass surgery versus percutaneous coronary intervention in patients with multivessel coronary artery disease: six-year follow-up from the Stent or Surgery Trial (SoS). Circulation. 2008; 118:381–388. PMID: 18606919.33. Sipahi I, Akay MH, Dagdelen S, Blitz A, Alhan C. Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease: meta-analysis of randomized clinical trials of the arterial grafting and stenting era. JAMA Intern Med. 2014; 174:223–230. PMID: 24296767.34. Sarno G, Garg S, Onuma Y, et al. Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol. 2010; 106:1369–1375. PMID: 21059423.35. Vieira RD, Hueb W, Gersh BJ, et al. Effect of complete revascularization on 10-year survival of patients with stable multivessel coronary artery disease: MASS II trial. Circulation. 2012; 126:S158–S163. PMID: 22965977.36. Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts--effects on survival over a 15-year period. N Engl J Med. 1996; 334:216–220. PMID: 8531997.37. Fitzgibbon GM, Kafka HP, Leach AJ, Keon WJ, Hooper GD, Burton JR. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol. 1996; 28:616–626. PMID: 8772748.38. De Bruyne B, Pijls NH, Kalesan B, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012; 367:991–1001. PMID: 22924638.39. Taggart DP, Altman DG, Gray AM, et al. Randomized trial of bilateral versus single internal-thoracic-artery grafts. N Engl J Med. 2016; 375:2540–2549. PMID: 27959712.40. Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA. 2011; 305:167–174. PMID: 21224458.41. Yamasaki M, Deb S, Tsubota H, et al. Comparison of radial artery and saphenous vein graft stenosis more than 5 years after coronary artery bypass grafting. Ann Thorac Surg. 2016; 102:712–719. PMID: 27154160.42. Gansera B, Schmidtler F, Angelis I, Kiask T, Kemkes BM, Botzenhardt F. Patency of internal thoracic artery compared to vein grafts - postoperative angiographic findings in 1189 symptomatic patients in 12 years. Thorac Cardiovasc Surg. 2007; 55:412–417. PMID: 17902061.43. Sardar P, Kundu A, Bischoff M, et al. Hybrid coronary revascularization versus coronary artery bypass grafting in patients with multivessel coronary artery disease: a meta-analysis. Catheter Cardiovasc Interv. 2018; 91:203–212. PMID: 28471093.44. Puskas JD, Halkos ME, DeRose JJ, et al. Hybrid coronary revascularization for the treatment of multivessel coronary artery disease: a multicenter observational study. J Am Coll Cardiol. 2016; 68:356–365. PMID: 27443431.45. Abdallah MS, Wang K, Magnuson EA, et al. Quality of life after surgery or DES in patients with 3-vessel or left main disease. J Am Coll Cardiol. 2017; 69:2039–2050. PMID: 28427580.46. Baron SJ, Chinnakondepalli K, Magnuson EA, et al. Quality-of-life after everolimus-eluting stents or bypass surgery for left-main disease: results from the EXCEL trial. J Am Coll Cardiol. 2017; 70:3113–3122. PMID: 29097293.47. Osnabrugge RL, Magnuson EA, Serruys PW, et al. Cost-effectiveness of percutaneous coronary intervention versus bypass surgery from a Dutch perspective. Heart. 2015; 101:1980–1988. PMID: 26552756.48. Cohen DJ, Osnabrugge RL, Magnuson EA, et al. Cost-effectiveness of percutaneous coronary intervention with drug-eluting stents versus bypass surgery for patients with 3-vessel or left main coronary artery disease: final results from the Synergy Between Percutaneous Coronary Intervention With TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2014; 130:1146–1157. PMID: 25085960.49. Kappetein AP, Head SJ, Morice MC, et al. Treatment of complex coronary artery disease in patients with diabetes: 5-year results comparing outcomes of bypass surgery and percutaneous coronary intervention in the SYNTAX trial. Eur J Cardiothorac Surg. 2013; 43:1006–1013. PMID: 23413014.50. Kapur A, Hall RJ, Malik IS, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial. J Am Coll Cardiol. 2010; 55:432–440. PMID: 20117456.51. Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012; 367:2375–2384. PMID: 23121323.52. Navarese EP, Kowalewski M, Kandzari D, et al. First-generation versus second-generation drug-eluting stents in current clinical practice: updated evidence from a comprehensive meta-analysis of randomised clinical trials comprising 31 379 patients. Open Heart. 2014; 1:e000064. PMID: 25332803.53. Wolff G, Dimitroulis D, Andreotti F, et al. Survival benefits of invasive versus conservative strategies in heart failure in patients with reduced ejection fraction and coronary artery disease: a meta-analysis. Circ Heart Fail. 2017; 10:e003255. PMID: 28087687.54. Hemmelgarn BR, Southern D, Culleton BF, Mitchell LB, Knudtson ML, Ghali WA. Survival after coronary revascularization among patients with kidney disease. Circulation. 2004; 110:1890–1895. PMID: 15451786.55. Chang TI, Shilane D, Kazi DS, Montez-Rath ME, Hlatky MA, Winkelmayer WC. Multivessel coronary artery bypass grafting versus percutaneous coronary intervention in ESRD. J Am Soc Nephrol. 2012; 23:2042–2049. PMID: 23204445.56. Lu R, Tang F, Zhang Y, et al. Comparison of drug-eluting and bare metal stents in patients with chronic kidney disease: an updated systematic review and meta-analysis. J Am Heart Assoc. 2016; 5:e003990. PMID: 27821401.57. Kim HJ, Kim JB, Jung SH, Choo SJ, Lee JW, Chung CH. Coronary artery bypass grafting in patients with severe chronic kidney disease: a propensity score-weighted analysis on the impact of on-pump versus off-pump strategies. Eur J Cardiothorac Surg. 2017; 52:937–944. PMID: 28958042.58. Wang Y, Zhu S, Gao P, Zhou J, Zhang Q. Off-pump versus on-pump coronary surgery in patients with chronic kidney disease: a meta-analysis. Clin Exp Nephrol. 2018; 22:99–109. PMID: 28634771.59. Graham MM, Ghali WA, Faris PD, Galbraith PD, Norris CM, Knudtson ML. Survival after coronary revascularization in the elderly. Circulation. 2002; 105:2378–2384. PMID: 12021224.60. Ramanathan KB, Weiman DS, Sacks J, et al. Percutaneous intervention versus coronary bypass surgery for patients older than 70 years of age with high-risk unstable angina. Ann Thorac Surg. 2005; 80:1340–1346. PMID: 16181866.61. McKellar SH, Brown ML, Frye RL, Schaff HV, Sundt TM 3rd. Comparison of coronary revascularization procedures in octogenarians: a systematic review and meta-analysis. Nat Clin Pract Cardiovasc Med. 2008; 5:738–746. PMID: 18825133.62. Varenne O, Cook S, Sideris G, et al. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet. 2018; 391:41–50. PMID: 29102362.63. TIME Investigators. Trial of invasive versus medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomised trial. Lancet. 2001; 358:951–957. PMID: 11583747.64. Authors/Task Force members. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619. PMID: 25173339.65. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011; 124:e574–e651. PMID: 22064601.66. Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2016 appropriate use criteria for coronary revascularization in patients with acute coronary syndromes: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society of Thoracic Surgeons. J Nucl Cardiol. 2017; 24:439–463. PMID: 28265967.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Coronary Intervention in Patients with ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease
- Current Status and Future Perspective of Left Main Coronary Intervention
- Ischemia-guided Revascularization for Stable Ischemic Heart Disease
- Stenting versus Bypass Surgery for the Treatment of Left Main Coronary Artery Disease
- Hybrid Coronary Revascularization Using Limited Incisional Full Sternotomy Coronary Artery Bypass Surgery in Multivessel Disease: Early Results