Arch Hand Microsurg.
2018 Mar;23(1):35-45. 10.12790/ahm.2018.23.1.35.
Operative Treatment for Nonunion of the Distal Scaphoid
- Affiliations
-
- 1Department of Orthopedic Surgery, Yonsei University College of Medicine, Seoul, Korea. KANGHO56@yuhs.ac
- KMID: 2412489
- DOI: http://doi.org/10.12790/ahm.2018.23.1.35
Abstract
- PURPOSE
The purpose of this study was to analyze the clinical and radiological outcomes of distal scaphoid nonunion patients who underwent operative treatment.
METHODS
From July 2006 to May 2014, there were a total of 9 distal scaphoid nonunion patients, with a mean age of 32 years. The mean time from symptom onset to operation was 15 months. Operative treatment was performed through a volar approach, osteosynthesis with an auto-iliac bone graft was performed. Union was determined through radiographs and computed tomography, while the scapholunate angle (SLA) and lateral intrascaphoid angle (LISA) were measured. Clinical outcomes were evaluated by assessing range of motion (ROM) of the wrist, the visual analogue scale (VAS), Mayo wrist score, and disabilities of arm, shoulder and hand (DASH) score.
RESULTS
The incidence of distal scaphoid nonunion was 11.8% (9/76), with all patients demonstrating union after the operation. Mean union time was 5 months and mean follow-up period was 23 months. Both SLA and LISA decreased, returning to normal range. The ROM of the wrist joint increased but not statistically significant. The postoperative VAS pain score improved, while grip strength advanced. In addition, both postoperative Mayo wrist and DASH scores document better results than those of pre-operation. Overall, there were two postoperative complication cases of joint motion limitation and pin site irritation.
CONCLUSION
Osteosynthesis with auto-iliac bone graft for nonunion of the distal scaphoid showed good clinical and radiological outcomes. Thus, it is considered a recommendable operation in the treatment of distal scaphoid nonunion.
Keyword
MeSH Terms
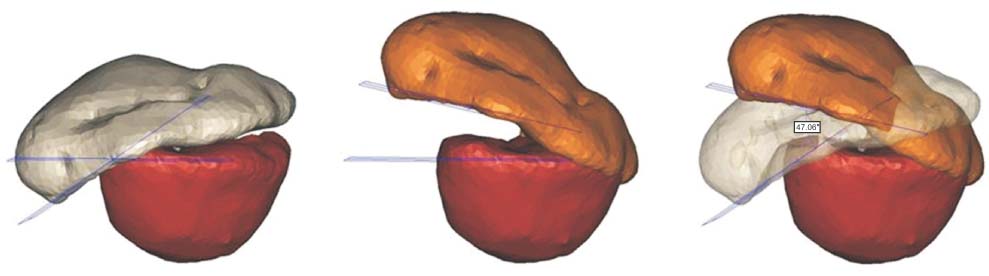
Figure
Reference
-
1. Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999; 33:423–426.
Article2. Herbert TJ, Fisher WE. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984; 66:114–123.
Article3. Leventhal EL, Wolfe SW, Moore DC, Akelman E, Weiss AP, Crisco JJ. Interfragmentary motion in patients with scaphoid nonunion. J Hand Surg Am. 2008; 33:1108–1115.
Article4. Grewal R, Suh N, MacDermid JC. The missed scaphoid fracture-outcomes of delayed cast treatment. J Wrist Surg. 2015; 4:278–283.5. Mack GR, Bosse MJ, Gelberman RH, Yu E. The natural history of scaphoid non-union. J Bone Joint Surg Am. 1984; 66:504–509.
Article6. Wong K, von Schroeder HP. Delays and poor management of scaphoid fractures: factors contributing to nonunion. J Hand Surg Am. 2011; 36:1471–1474.
Article7. Gelberman RH, Menon J. The vascularity of the scaphoid bone. J Hand Surg Am. 1980; 5:508–513.
Article8. Moritomo H, Murase T, Oka K, Tanaka H, Yoshikawa H, Sugamoto K. Relationship between the fracture location and the kinematic pattern in scaphoid nonunion. J Hand Surg Am. 2008; 33:1459–1468.
Article9. Oron A, Gupta A, Thirkannad S. Nonunion of the scaphoid distal pole. Hand Surg. 2013; 18:35–39.
Article10. Cooney WP, Dobyns JH, Linscheid RL. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res. 1980; (149):90–97.11. Jones DB Jr, Bürger H, Bishop AT, Shin AY. Treatment of scaphoid waist nonunions with an avascular proximal pole and carpal collapse. J Bone Joint Surg Am. 2008; 90:2616–2625.
Article12. Prosser AJ, Brenkel IJ, Irvine GB. Articular fractures of the distal scaphoid. J Hand Surg Br. 1988; 13:87–91.
Article13. Kang HJ, Park H, Hahn SB. The treatment of nonunion of the scaphoid with a horse-shoe bone graft and fixation with two screws. J Korean Orthop Assoc. 2009; 44:651–660.
Article14. Maudsley RH, Chen SC. Screw fixation in the management of the fractured carpal scaphoid. J Bone Joint Surg Br. 1972; 54:432–441.
Article15. Gelberman RH, Wolock BS, Siegel DB. Fractures and non-unions of the carpal scaphoid. J Bone Joint Surg Am. 1989; 71:1560–1565.
Article16. Tuncay I, Doğan A, Alpaslan S. Comparison between fixation with Herbert screws and Kirschner wires in the treatment of scaphoid pseudoarthrosis. Acta Orthop Traumatol Turc. 2002; 36:17–21.17. Schneider LH, Aulicino P. Nonunion of the carpal scaphoid: the Russe procedure. J Trauma. 1982; 22:315–319.18. Stark HH, Rickard TA, Zemel NP, Ashworth CR. Treatment of ununited fractures of the scaphoid by iliac bone grafts and Kirschner-wire fixation. J Bone Joint Surg Am. 1988; 70:982–991.
Article19. Jiranek WA, Ruby LK, Millender LB, Bankoff MS, Newberg AH. Long-term results after Russe bone-grafting: the effect of malunion of the scaphoid. J Bone Joint Surg Am. 1992; 74:1217–1228.20. Rajagopalan BM, Squire DS, Samuels LO. Results of Herbert-screw fixation with bone-grafting for the treatment of nonunion of the scaphoid. J Bone Joint Surg Am. 1999; 81:48–52.
Article21. Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL. Scaphoid malunion. J Hand Surg Am. 1989; 14:679–687.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Arthroscopic Bone Grafting and Kirschner-Wires Fixation for Scaphoid Nonunion
- Treatment of Scaphoid Nonunion with Matti - Russe Technique
- Scaphoid Fractures and Nonunions: Recent Trends of Treatment
- Scaphoid Fractures and Nonunion
- The Effect of Smoking on the Outcomes of Vascularized Bone Graft Surgery in Scaphoid Nonunion through Meta-analysis