Ann Hepatobiliary Pancreat Surg.
2018 May;22(2):105-115. 10.14701/ahbps.2018.22.2.105.
Are traditional scoring systems for severity stratification of acute pancreatitis sufficient?
- Affiliations
-
- 1Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore.
- 2Department of General Surgery, Tan Tock Seng Hospital, Singapore, Singapore. vgshelat@rediffmail.com
- KMID: 2412425
- DOI: http://doi.org/10.14701/ahbps.2018.22.2.105
Abstract
- BACKGROUNDS/AIMS
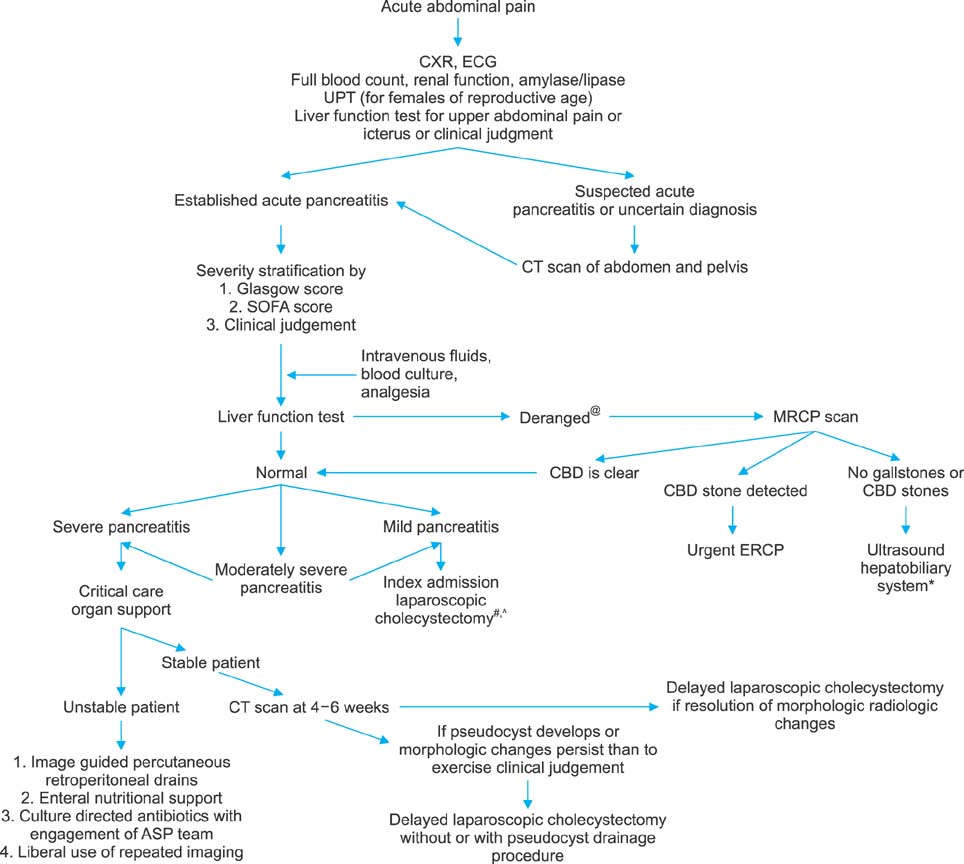
Ranson's score (RS) and Glasgow score (GS) have been utilized to stratify the severity of acute pancreatitis (AP). The aim of this study was to validate RS and GS for stratifying the severity of acute pancreatitis and audit our experience of managing AP.
METHODS
We conducted a retrospective review of patients treated for AP from July 2009 to September 2016. Final severity was determined using the revised Atlanta classification. Mortality and complications were analyzed.
RESULTS
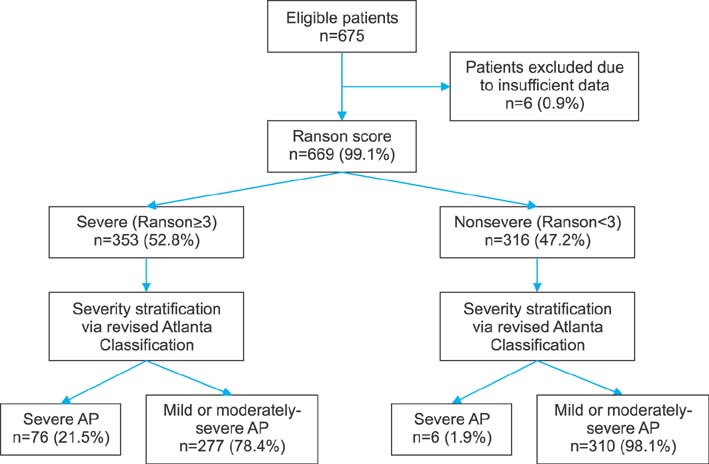
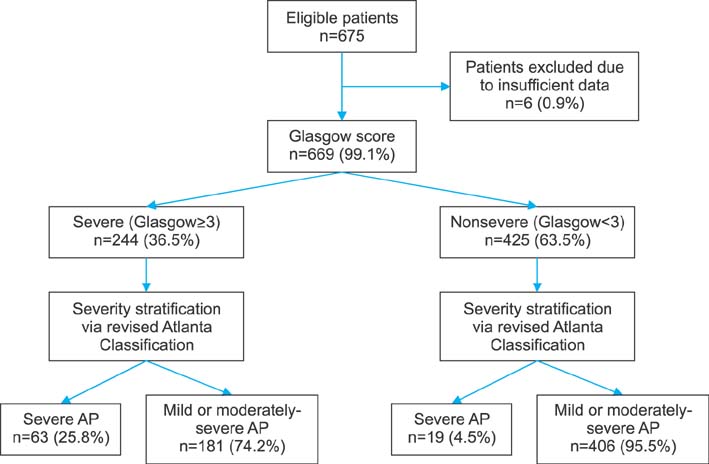
From July 2009 to September 2016, a total of 675 patients with a diagnosis of AP were admitted at the hospital. Of them, 669 patients who had sufficient data were analyzed. Their average age±SD was 58.7±17.4 years (range, 21-98 years). There was a male preponderance (n=393, 53.8%). A total of 82 (12.3%) patients had eventual severe pancreatitis. RS demonstrated a sensitivity of 92.7% and a specificity of 52.8% with a positive predictive value (PPV) of 21.5% and a negative predictive value (NPV) of 98.1%. GS demonstrated a sensitivity of 76.8% and a specificity of 69.2% with a PPV of 25.8% and a NPV of 95.5%. For severity prediction, areas under the curve (AUCs) for RS and GS were 0.848 (95% CI: 0.819-0.875) and 0.784 (95% CI: 0.750-0.814), respectively (p=0.003). Twelve (1.6%) patients died in the hospital.
CONCLUSIONS
RS has higher sensitivity, NPV and AUC for predicting severity of AP than GS.
MeSH Terms
Figure
Reference
-
1. Clancy TE, Benoit EP, Ashley SW. Current management of acute pancreatitis. J Gastrointest Surg. 2005; 9:440–452.
Article2. Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013; 108:1400–1415. 1416
Article3. Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006; 101:2379–2400.
Article4. Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013; 62:102–111.
Article5. Beger HG, Rau BM. Severe acute pancreatitis: clinical course and management. World J Gastroenterol. 2007; 13:5043–5051.
Article6. Shelat VG, Diddapur RK. Minimally invasive retroperitoneal pancreatic necrosectomy in necrotising pancreatitis. Singapore Med J. 2007; 48:e220–e223.7. Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974; 139:69–81.8. Blamey SL, Imrie CW, O'Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis. Gut. 1984; 25:1340–1346.
Article9. Papachristou GI, Muddana V, Yadav D, O'Connell M, Sanders MK, Slivka A, et al. Comparison of BISAP, Ranson's, APACHE-II, and CTSI scores in predicting organ failure, complications, and mortality in acute pancreatitis. Am J Gastroenterol. 2010; 105:435–441. quiz 442.
Article10. Simoes M, Alves P, Esperto H, Canha C, Meira E, Ferreira E, et al. Predicting acute pancreatitis severity: comparison of prognostic scores. Gastroenterology Res. 2011; 4:216–222.
Article11. Mounzer R, Langmead CJ, Wu BU, Evans AC, Bishehsari F, Muddana V, et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology. 2012; 142:1476–1482. quiz e15-e16.
Article12. Bollen TL, Singh VK, Maurer R, Repas K, van Es HW, Banks PA, et al. A comparative evaluation of radiologic and clinical scoring systems in the early prediction of severity in acute pancreatitis. Am J Gastroenterol. 2012; 107:612–619.
Article13. Williams M, Simms HH. Prognostic usefulness of scoring systems in critically ill patients with severe acute pancreatitis. Crit Care Med. 1999; 27:901–907.
Article14. De Bernardinis M, Violi V, Roncoroni L, Boselli AS, Giunta A, Peracchia A. Discriminant power and information content of Ranson's prognostic signs in acute pancreatitis: a meta-analytic study. Crit Care Med. 1999; 27:2272–2283.
Article15. Robert JH, Frossard JL, Mermillod B, Soravia C, Mensi N, Roth M, et al. Early prediction of acute pancreatitis: prospective study comparing computed tomography scans, Ranson, Glascow, Acute Physiology and Chronic Health Evaluation II scores, and various serum markers. World J Surg. 2002; 26:612–619.16. Chauhan S, Forsmark CE. The difficulty in predicting outcome in acute pancreatitis. Am J Gastroenterol. 2010; 105:443–445.
Article17. Larvin M, McMahon MJ. APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet. 1989; 2:201–205.
Article18. Leese T, Shaw D, Holliday M. Prognostic markers in acute pancreatitis: can pancreatic necrosis be predicted. Ann R Coll Surg Engl. 1988; 70:227–232.19. Kandasami P, Harunarashid H, Kaur H. Acute pancreatitis in a multi-ethnic population. Singapore Med J. 2002; 43:284–288.20. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 1996; 22:707–710.21. Adam F, Bor C, Uyar M, Demırağ K, Çankayalı İ. Severe acute pancreatitis admitted to intensive care unit: SOFA is superior to Ranson's criteria and APACHE II in determining prognosis. Turk J Gastroenterol. 2013; 24:430–435.
Article22. Chari ST, Smyrk TC, Levy MJ, Topazian MD, Takahashi N, Zhang L, et al. Diagnosis of autoimmune pancreatitis: the Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006; 4:1010–1016. quiz 934.
Article23. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.
Article24. Anbalakan K, Chua D, Pandya GJ, Shelat VG. Five year experience in management of perforated peptic ulcer and validation of common mortality risk prediction models - are existing models sufficient? A retrospective cohort study. Int J Surg. 2015; 14:38–44.
Article25. Department of Statistics, Ministry of Trade and Industry, Republic of Singapore. Population. Department of Statistics, Ministry of Trade and Industry, Republic of Singapore. Population trends, 2016. 12th ed. Singapore: Department of Statistics, Singapore;2016. p. 3–17.26. Health Information Division, Ministry of Health, Singapore. Morbidity and biographic profile of patients. Ministry of Health, Singapore. Primary care survey 2010. Singapore: Ministry of Health, Singapore;2010. p. 6–14.27. Cho JH, Kim TN, Chung HH, Kim KH. Comparison of scoring systems in predicting the severity of acute pancreatitis. World J Gastroenterol. 2015; 21:2387–2394.
Article28. Wu BU, Bakker OJ, Papachristou GI, Besselink MG, Repas K, van Santvoort HC, et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch Intern Med. 2011; 171:669–676.
Article29. Wu BU, Johannes RS, Sun X, Conwell DL, Banks PA. Early changes in blood urea nitrogen predict mortality in acute pancreatitis. Gastroenterology. 2009; 137:129–135.
Article30. Talamini G, Uomo G, Pezzilli R, Rabitti PG, Billi P, Bassi C, et al. Serum creatinine and chest radiographs in the early assessment of acute pancreatitis. Am J Surg. 1999; 177:7–14.
Article31. Lankisch PG, Weber-Dany B, Maisonneuve P, Lowenfels AB. High serum creatinine in acute pancreatitis: a marker for pancreatic necrosis? Am J Gastroenterol. 2010; 105:1196–1200.
Article32. Muddana V, Whitcomb DC, Khalid A, Slivka A, Papachristou GI. Elevated serum creatinine as a marker of pancreatic necrosis in acute pancreatitis. Am J Gastroenterol. 2009; 104:164–170.
Article33. Hirota M, Takada T, Kawarada Y, Hirata K, Mayumi T, Yoshida M, et al. JPN guidelines for the management of acute pancreatitis: severity assessment of acute pancreatitis. J Hepatobiliary Pancreat Surg. 2006; 13:33–41.
Article34. Hritz I, Hegyi P. Early Achievable Severity (EASY) index for simple and accurate expedite risk stratification in acute pancreatitis. J Gastrointestin Liver Dis. 2015; 24:177–182.
Article35. Wang X, Cui Z, Li H, Saleen AF, Zhang D, Miao B, et al. Nosocomial mortality and early prediction of patients with severe acute pancreatitis. J Gastroenterol Hepatol. 2010; 25:1386–1393.
Article36. Ueda T, Takeyama Y, Yasuda T, Matsumura N, Sawa H, Nakajima T, et al. Simple scoring system for the prediction of the prognosis of severe acute pancreatitis. Surgery. 2007; 141:51–58.
Article37. Han C, Zeng J, Lin R, Liu J, Qian W, Ding Z, et al. The utility of neutrophil to lymphocyte ratio and fluid sequestration as an early predictor of severe acute pancreatitis. Sci Rep. 2017; 7:10704.
Article38. Yue W, Liu Y, Ding W, Jiang W, Huang J, Zhang J, et al. The predictive value of the prealbumin-to-fibrinogen ratio in patients with acute pancreatitis. Int J Clin Pract. 2015; 69:1121–1128.
Article39. Valverde-López F, Matas-Cobos AM, Alegría-Motte C, Jiménez-Rosales R, Úbeda-Muñoz M, Redondo-Cerezo E. BISAP, RANSON, lactate and others biomarkers in prediction of severe acute pancreatitis in a European cohort. J Gastroenterol Hepatol. 2017; 32:1649–1656.
Article40. Shah KS, Shelat VG, Jogai S, Trompetas V. Primary gallbladder lymphoma presenting with perforated cholecystitis and hyperamylasaemia. Ann R Coll Surg Engl. 2016; 98:e13–e15.
Article41. Tan YHA, Rafi S, Tyebally Fang M, Hwang S, Lim EW, Ngu J, et al. Validation of the modified Ranson versus Glasgow score for pancreatitis in a Singaporean population. ANZ J Surg. 2015; 87:700–703.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Severity in Acute Pancreatitis
- Diagnosis and Predicting Severity in Acute Pancreatitis
- Evaluation of Severity of Childhood Pancreatitis with Multiple Factor Scoring Systems
- A comparison of the BISAP score and serum procalcitonin for predicting the severity of acute pancreatitis
- Comparison of Multiple Scoring Systems and CT Severity Index for Systemic and Local Complications of Acute Pancreatitis