Clin Orthop Surg.
2016 Jun;8(2):133-139. 10.4055/cios.2016.8.2.133.
Measurement of Optimal Insertion Angle for Iliosacral Screw Fixation Using Three-Dimensional Computed Tomography Scans
- Affiliations
-
- 1Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Orthopedic Surgery, UC Davis Medical Center, Sacramento, CA, USA.
- 3Department of Orthopedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea. osd11@paik.ac.kr
- KMID: 2412336
- DOI: http://doi.org/10.4055/cios.2016.8.2.133
Abstract
- BACKGROUND
Percutaneous iliosacral screw fixation can provide stable fixation with a minimally invasive surgical technique for unstable posterior pelvic ring injuries. This surgical technique is not limited by cases of difficult fracture patterns, sacral dysplasia, and small sacral pedicles that can occur in Asians. The purpose of this study was to investigate the incidence of the sacral dysplasia in the Korean population and determine the optimal direction of iliosacral screws by analyzing pelvic three-dimensional computed tomography (3D-CT) scans.
METHODS
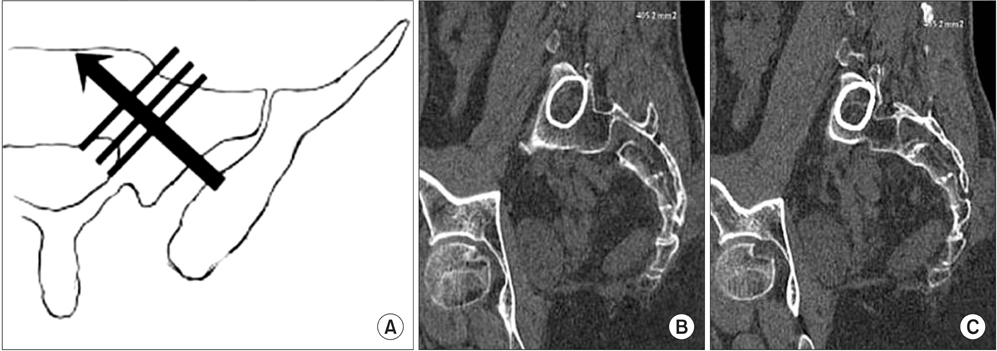
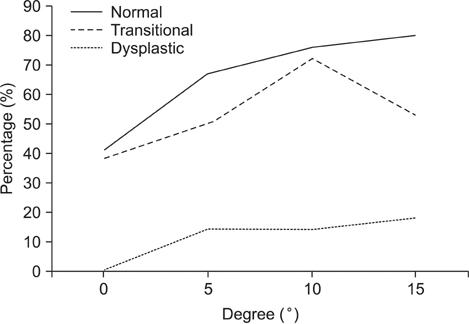
One hundred adult patients who had pelvic 3D-CT scans were evaluated. The upper sacral morphology was classified into three groups, i.e., normal, transitional, and dysplastic groups; the cross-sectional area of the safe zone was measured in each group. S1 pedicle with a short width of more than 11 mm was defined as safe pedicle. The incidences of safe pedicles at different angles ranging from 0° to 15° were investigated in order to determine optimal angle for screw direction.
RESULTS
The incidence of normal, transitional, and dysplastic group was 46%, 32%, and 22%, respectively. There were significant increases of the cross-sectional area of the safe zones by increasing the angles from 0° to 15° in all groups. The incidence of safe pedicles increased similar to the changes in cross-sectional area. The overall incidence of safe pedicles was highest at the 10° tilt angle.
CONCLUSIONS
The incidence of sacral dysplasia in Koreans was 54%, which is higher than previous studies for Western populations. The cross-sectional area of the safe zone can be increased by anteromedial direction of the iliosacral screw. Considering the diversity of sacral morphology present in the Korean population, a tilt angle of 10° may be the safest angle.
Keyword
MeSH Terms
Figure
Reference
-
1. Ebraheim NA, Coombs R, Hoeflinger MJ, Zeman C, Jackson WT. Anatomical and radiological considerations in compressive bar technique for posterior pelvic disruptions. J Orthop Trauma. 1991; 5(4):434–438.2. Kim HT, Son KM, Cheon SJ, Yoo CI. Treatment of pelvic bone fracture involving the sacrum and sacroiliac joint. J Korean Soc Fract. 2001; 14(3):313–322.
Article3. Oh JK, Bae SY, Kim JO, Roh KJ, Lee JJ, Chang SY. Radiologic evaluation for the safe zone of percutaneous iliosacral screw fixation. J Korean Soc Fract. 2002; 15(3):336–341.
Article4. Altman DT, Jones CB, Routt ML Jr. Superior gluteal artery injury during iliosacral screw placement. J Orthop Trauma. 1999; 13(3):220–227.
Article5. Routt ML Jr, Simonian PT, Mills WJ. Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma. 1997; 11(8):584–589.
Article6. Sagi HC, Lindvall EM. Inadvertent intraforaminal iliosacral screw placement despite apparent appropriate positioning on intraoperative fluoroscopy. J Orthop Trauma. 2005; 19(2):130–133.
Article7. Stephen DJ. Pseudoaneurysm of the superior gluteal arterial system: an unusual cause of pain after a pelvic fracture. J Trauma. 1997; 43(1):146–149.8. Routt ML Jr, Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996; 10(3):171–177.
Article9. Ebraheim NA, Xu R, Biyani A, Nadaud MC. Morphologic considerations of the first sacral pedicle for iliosacral screw placement. Spine (Phila Pa 1976). 1997; 22(8):841–846.
Article10. Mirkovic S, Abitbol JJ, Steinman J, et al. Anatomic consideration for sacral screw placement. Spine (Phila Pa 1976). 1991; 16:6 Suppl. S289–S294.
Article11. Xu R, Ebraheim NA, Robke J, Yeasting RA. Radiologic evaluation of iliosacral screw placement. Spine (Phila Pa 1976). 1996; 21(5):582–588.
Article12. Conflitti JM, Graves ML, Chip Routt ML Jr. Radiographic quantification and analysis of dysmorphic upper sacral osseous anatomy and associated iliosacral screw insertions. J Orthop Trauma. 2010; 24(10):630–636.
Article13. Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML Jr. Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma. 2010; 24(10):622–629.
Article14. Wu LP, Li YK, Li YM, Zhang YQ, Zhong SZ. Variable morphology of the sacrum in a Chinese population. Clin Anat. 2009; 22(5):619–626.
Article15. Miller AN, Routt ML Jr. Variations in sacral morphology and implications for iliosacral screw fixation. J Am Acad Orthop Surg. 2012; 20(1):8–16.
Article16. Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the "vestibule" concept. J Orthop Trauma. 2000; 14(4):264–269.
Article17. Day CS, Prayson MJ, Shuler TE, Towers J, Gruen GS. Transsacral versus modified pelvic landmarks for percutaneous iliosacral screw placement: a computed tomographic analysis and cadaveric study. Am J Orthop (Belle Mead NJ). 2000; 29:9 Suppl. 16–21.18. Kim JJ, Jung CY, Oh HK, Yang BS, Chang JS. Upper sacral morphology related to iliosacral screw fixation in Korean. J Korean Fract Soc. 2007; 20(2):115–122.
Article19. Noojin FK, Malkani AL, Haikal L, Lundquist C, Voor MJ. Cross-sectional geometry of the sacral ala for safe insertion of iliosacral lag screws: a computed tomography model. J Orthop Trauma. 2000; 14(1):31–35.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Iliosacral Screw Fixation of the Posterior Pelvic Ring Using Local Anesthesia and Computerized Tomography
- Rate of Pedicle Disruption after Screw Fixation
- Superior Gluteal Artery Injury during Percutaneous Iliosacral Screw Fixation: A Case Report
- Ideal Insertion Point and Angle of Cervical Pedicular Screws in Korean
- Percutaneous Iliosacral Screw Fixation in Unstable Pelvic Ring Injury