Clin Orthop Surg.
2017 Mar;9(1):29-36. 10.4055/cios.2017.9.1.29.
Healing Process of Osteonecrotic Lesions of the Femoral Head Following Transtrochanteric Rotational Osteotomy: A Computed Tomography-Based Study
- Affiliations
-
- 1Department of Orthopedic Surgery, Korea University Guro Hospital, Seoul, Korea. shonwy@hotmail.com
- 2Department of Radiology, Korea University Guro Hospital, Seoul, Korea.
- KMID: 2412300
- DOI: http://doi.org/10.4055/cios.2017.9.1.29
Abstract
- BACKGROUND
Transtrochanteric rotational osteotomy (TRO) is a controversial hip-preserving procedure with a variable success rate. The healing process of femoral head osteonecrosis after TRO has been poorly explained till now. This study aimed to evaluate the healing process of previously transposed necrotic lesion after a TRO for nontraumatic osteonecrosis of the femoral head using computed tomography (CT).
METHODS
Among 52 patients (58 hips) who had preserved original femoral head after TRO, we retrospectively reviewed 27 patients (28 hips) who had undergone sequential CT scans and had no major complication following TRO. The average age was 34 years (range, 18 to 59 years). The mean follow-up period was 9.1 years. We evaluated the reparative process of the transposed osteonecrotic lesion with CT scans.
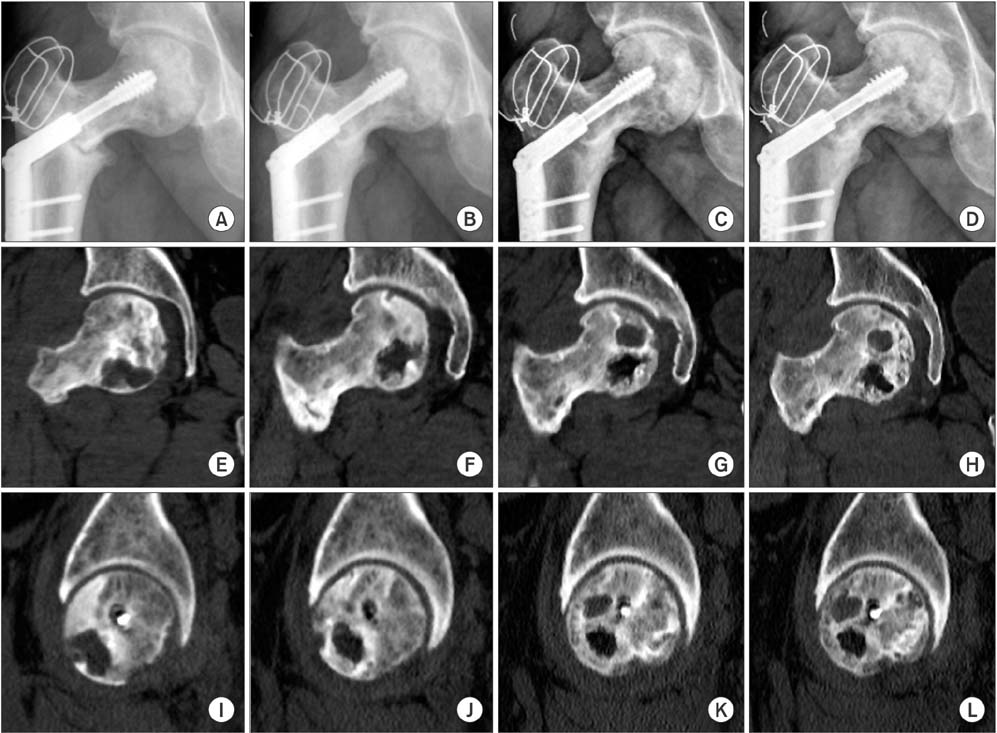
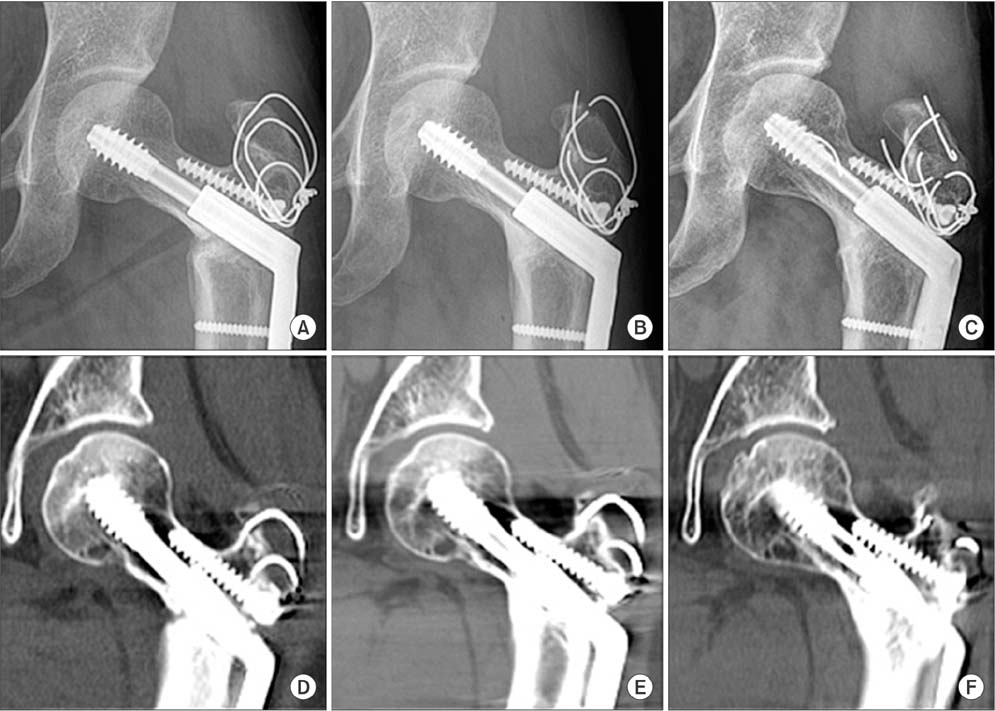
RESULTS
Plain radiographs of the osteonecrotic lesion revealed sclerotic and lucent changes in 14 hips (50%) and normal bony architecture in the other 14 hips (50%) at the final follow-up. CT scans of the osteonecrotic lesions showed cystic changes with heterogeneous sclerosis in 13 hips (46%), normal trabecular bone with or without small cysts in 9 hips (32%), and fragmentation of the necrotic lesion in 6 hips (22%). Seventeen hips (60%) showed minimal (13 hips) to mild (4 hips) nonprogressive collapse of the transposed osteonecrotic area. The collapse of the transposed osteonecrotic area on the CT scan was significantly associated with the healing pattern (p = 0.009), as all 6 patients (6 hips) with fragmentation of the necrotic lesion had minimal (5 hips) to mild (1 hip) collapse. Furthermore, a significant association was found between the collapse of the transposed osteonecrotic area on the CT scan of 17 hips (60%) and postoperative Harris hip score (p = 0.021). We observed no differences among the healing patterns on CT scans with regard to age, gender, etiology, staging, preoperative lesion type, preoperative intact area, percentage of necrotic area, direction of rotation and immediate postoperative intact area.
CONCLUSIONS
The majority of the hips showed incomplete regeneration of the transposed osteonecrotic lesion with cysts, sclerosis, and fragmentation, whereas repair with normal trabecular bone was observed only in one-third of the hips that were preserved after Sugioka TRO.
Keyword
MeSH Terms
Figure
Reference
-
1. Kokubo T, Takatori Y, Ninomiya S, Nakamura T, Kamogawa M. Magnetic resonance imaging and scintigraphy of avascular necrosis of the femoral head: prediction of subsequent segmental collapse. Clin Orthop Relat Res. 1992; (277):54–60.2. Ohzono K, Saito M, Takaoka K, et al. Natural history of nontraumatic avascular necrosis of the femoral head. J Bone Joint Surg Br. 1991; 73(1):68–72.
Article3. Nishii T, Sugano N, Ohzono K, Sakai T, Haraguchi K, Yoshikawa H. Progression and cessation of collapse in osteonecrosis of the femoral head. Clin Orthop Relat Res. 2002; (400):149–157.
Article4. Merle D'Aubigne R, Postel M, Mazabraud A, Massias P, Gueguen J, France P. Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br. 1965; 47(4):612–633.5. Sugioka Y. Transtrochanteric anterior rotational osteotomy of the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res. 1978; (130):191–201.6. Biswal S, Hazra S, Yun HH, Hur CY, Shon WY. Transtrochanteric rotational osteotomy for nontraumatic osteonecrosis of the femoral head in young adults. Clin Orthop Relat Res. 2009; 467(6):1529–1537.
Article7. Hisatome T, Yasunaga Y, Takahashi K, Ochi M. Progressive collapse of transposed necrotic area after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head induces osteoarthritic change: mid-term results of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2004; 124(2):77–81.
Article8. Inao S, Ando M, Gotoh E, Matsuno T. Minimum 10-year results of Sugioka's osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res. 1999; (368):141–148.
Article9. Koo KH, Song HR, Yang JW, Yang P, Kim JR, Kim YM. Trochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2001; 83(1):83–89.
Article10. Miyanishi K, Noguchi Y, Yamamoto T, et al. Prediction of the outcome of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2000; 82(4):512–516.
Article11. Sugioka Y. Transtrochanteric rotational osteotomy in the treatment of idiopathic and steroid-induced femoral head necrosis, Perthes' disease, slipped capital femoral epiphysis, and osteoarthritis of the hip: indications and results. Clin Orthop Relat Res. 1984; (184):12–23.12. Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head: indications and longterm results. Clin Orthop Relat Res. 1992; (277):111–120.13. Sugioka Y, Katsuki I, Hotokebuchi T. Transtrochanteric rotational osteotomy of the femoral head for the treatment of osteonecrosis: follow-up statistics. Clin Orthop Relat Res. 1982; (169):115–126.14. Sugioka Y, Yamamoto T. Transtrochanteric posterior rotational osteotomy for osteonecrosis. Clin Orthop Relat Res. 2008; 466(5):1104–1109.
Article15. Zhao G, Yamamoto T, Motomura G, et al. Radiological outcome analyses of transtrochanteric posterior rotational osteotomy for osteonecrosis of the femoral head at a mean follow-up of 11 years. J Orthop Sci. 2013; 18(2):277–283.
Article16. Zhao G, Yamamoto T, Ikemura S, et al. Clinico-radiological factors affecting the joint space narrowing after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Orthop Sci. 2012; 17(4):390–396.
Article17. Yamamoto T, Ikemura S, Iwamoto Y, Sugioka Y. The repair process of osteonecrosis after a transtrochanteric rotational osteotomy. Clin Orthop Relat Res. 2010; 468(12):3186–3191.
Article18. Yamasaki T, Yasunaga Y, Hisatome T, Tanaka R, Ochi M. Bone remodeling of a femoral head after transtrochanteric rotational osteotomy for osteonecrosis associated with slipped capital femoral epiphysis: a case report. Arch Orthop Trauma Surg. 2005; 125(7):486–489.
Article19. Yasunaga Y, Hisatome T, Ikuta Y, Nakamura S. A histological study of the necrotic area after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2001; 83(2):167–170.
Article20. Yamashita A, Yamamoto T, Jingushi S, Iwamoto Y, Sugioka Y, Sueishi K. Histopathological study of osteonecrosis 19 years after transtrochanteric rotational osteotomy. J Orthop Sci. 2006; 11(6):632–637.
Article21. Hasegawa Y, Yamaguchi J, Kanoh T, Seki T, Kawabe K. Low signal intensity area by magnetic resonance imaging that disappeared after a curved intertrochanteric varus osteotomy for traumatic osteonecrosis of the femoral head. J Orthop Sci. 2008; 13(3):265–268.
Article22. Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995; 77(3):459–474.
Article23. Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2002; 7(5):601–605.
Article24. Kim YM, Ahn JH, Kang HS, Kim HJ. Estimation of the extent of osteonecrosis of the femoral head using MRI. J Bone Joint Surg Br. 1998; 80(6):954–958.
Article25. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969; 51(4):737–755.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posttraumatic Osteonecrosis of the Femoral Head after Nine Years of Posterior Femoral Head Fracture Dislocation
- Comparison of the Results of Core Decompression and Sugioka's Transtrochanteric Rotational Osteotomy for Osteonecrosis of the Femoral Head
- Clinical Results of Transtrochanteric Rotational Osteotomy for Nontraumatic Avascular Necrosis of the Femoral Head
- Result of Sugioka's Transtrochanteric Osteotomy forOsteonecrosis of Femoral Head
- The Result of Sugioka's Transtrochanteric Rotational Osteotomy