J Korean Ophthalmol Soc.
2018 May;59(5):428-436. 10.3341/jkos.2018.59.5.428.
The Treatment of Large Macular Holes Using a Multi-layered Inverted Internal Limiting Membrane Flap Technique
- Affiliations
-
- 1Department of Ophthalmology, Maryknoll Medical Center, Busan, Korea. Pjm1438@hanmail.net
- KMID: 2411451
- DOI: http://doi.org/10.3341/jkos.2018.59.5.428
Abstract
- PURPOSE
To describe a multi-layered inverted internal limiting membrane (ILM) flap technique and to evaluate the surgical outcomes of this surgery in patients with macular holes > 800 µm in base diameter.
METHODS
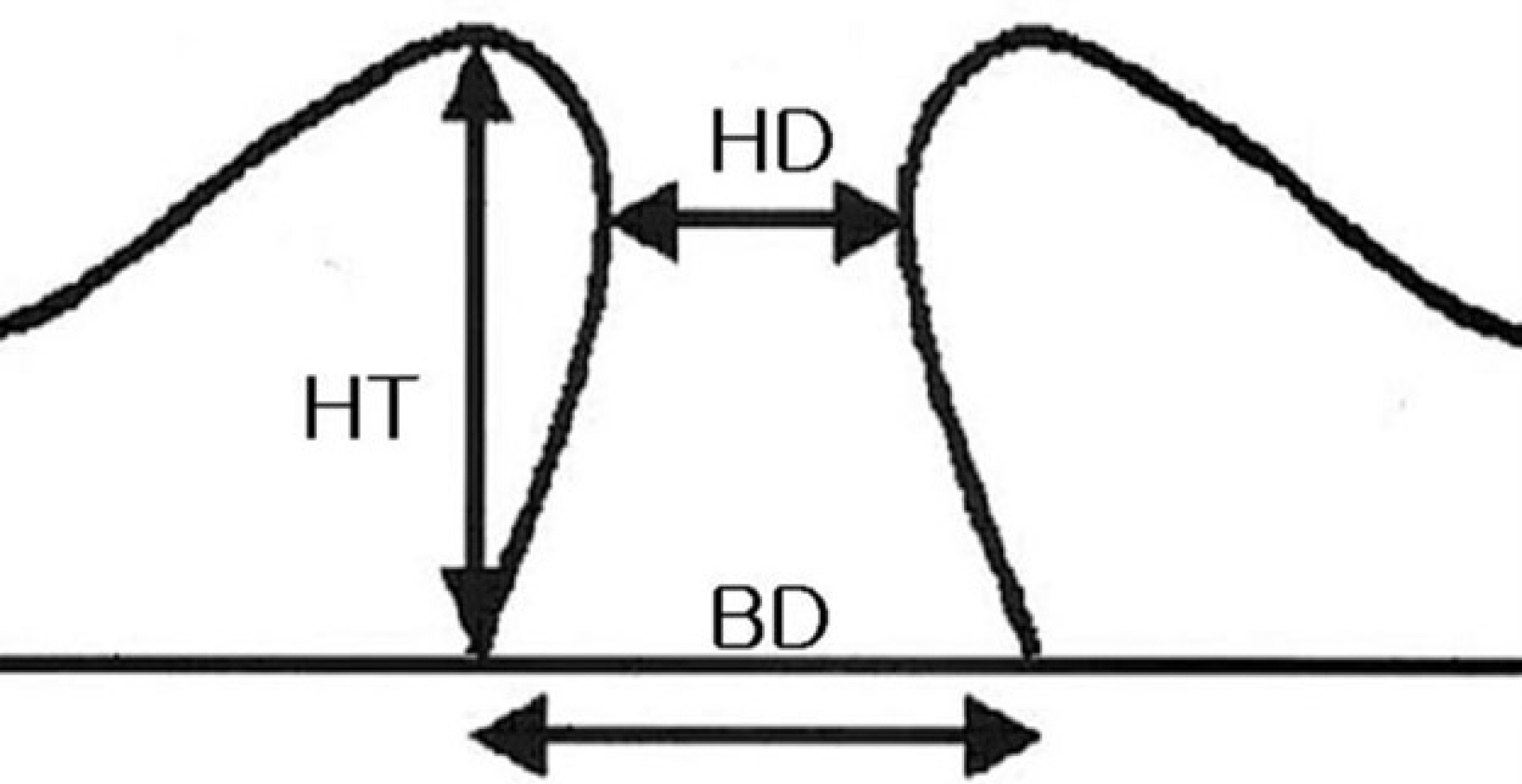
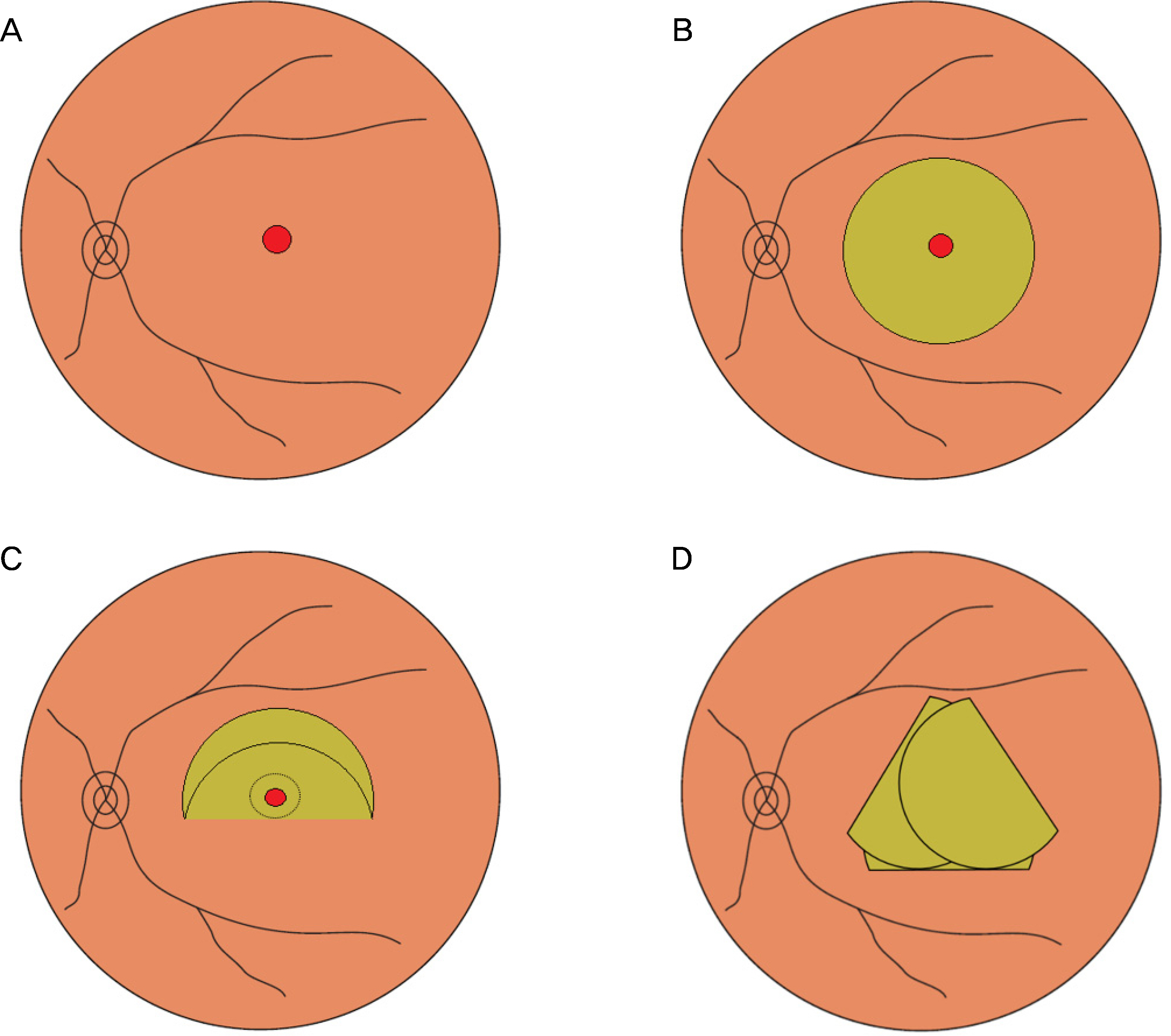
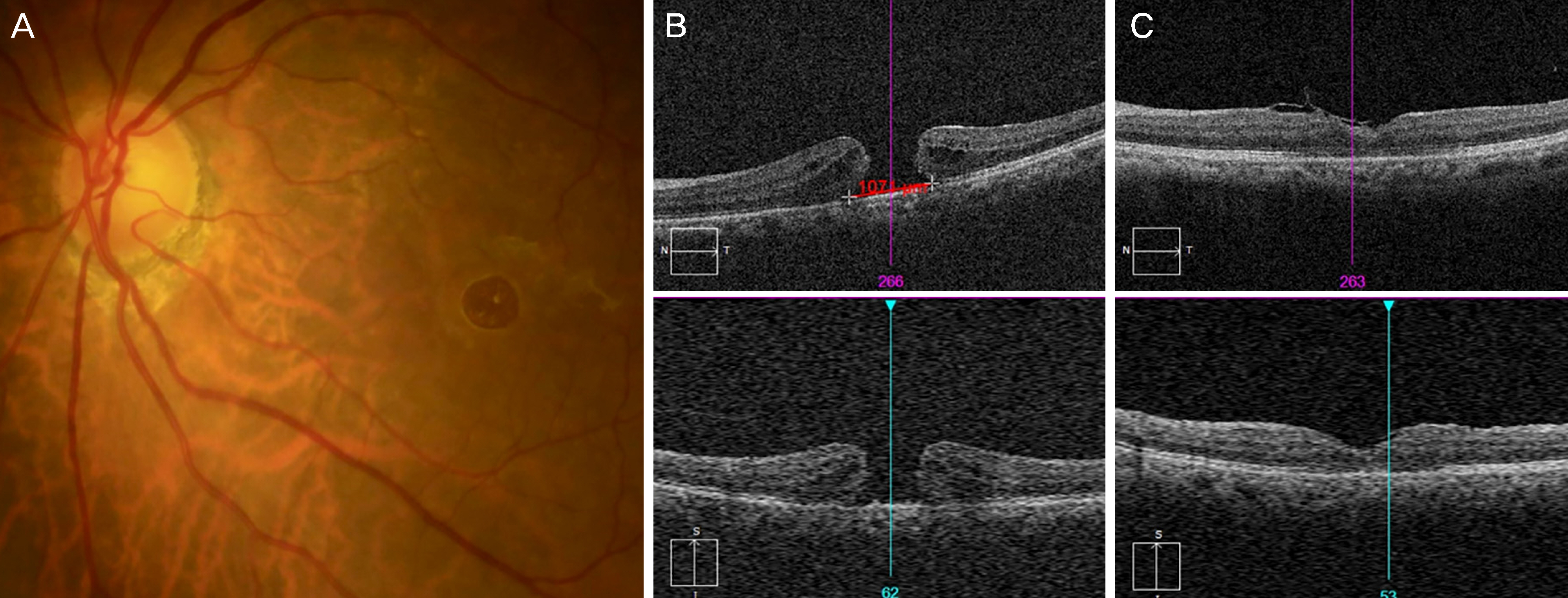
The medical records of patients who received a multi-layered ILM flap technique were retrospectively studied and patients with macular holes > 800 µm were included in the analyses. Best-corrected visual acuity (BCVA) before and after surgery, preoperative hole size, hole base size, vertical size, and hole closure after surgery were checked using spectral domain optical coherence tomography. Pars plana vitrectomy was performed and the ILM was stained using indocyanine green and peeled with the base attached at the hole margin. The ILM flap was inverted over the macular hole with 2~3 layers, and gas injection was performed.
RESULTS
The mean age of 12 patients was 65.2 ± 12.3 years. The mean BCVA (logMAR) was 1.27 ± 0.61. The mean hole size was 563.6 ± 221.9 µm, the mean vertical size was 418.8 ± 80.9 µm, and the mean hole base size was 1,182.8 ± 298.5 µm. The mean follow-up period was 174.4 ± 143.3 days. Nine macular holes were closed after surgery but three macular holes were not closed. The postoperative mean BCVA (logMAR) was 0.21 ± 0.51. Eight eyes showed visual improvement while three eyes did not show visual improvement after macular hole surgery.
CONCLUSIONS
The macular hole was closed successfully and the visual acuity improved after the multi-layered, inverted ILM flap technique. The multi-layered, inverted ILM flap technique is therefore considered the treatment of choice for large macular holes.
Keyword
MeSH Terms
Figure
Reference
-
References
1. La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand. 2002; 80:579–87.
Article2. Johnson RN, Gass JD. Idiopathic macular holes. Observations, stages of formation, and implications for surgical intervention. Ophthalmology. 1988; 95:917–24.3. Yooh HS, Brooks HL Jr, Capone A Jr, et al. Ultrastructural features of tissue removed during idiopathic macular hole surgery. Am J Ophthalmol. 1996; 122:67–75.4. Tatham A, Banerjee S. Face-down posturing after macular hole surgery: a meta-analysis. Br J Ophthalmol. 2010; 94:626–31.
Article5. Konstantinidis A, Hero M, Nanos P, Panos GD. Efficacy of abdominal platelets in macular hole surgery. Clin Ophthalmol. 2013; 7:745–50.6. Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large abdominal holes. Ophthalmology. 2010; 117:2018–25.7. Kuriyama S, Hayashi H, Jingami Y, et al. Efficacy of inverted abdominal limiting membrane flap technique for the treatment of macular hole in high myopia. Am J Ophthalmol. 2013; 156:125–31.e1.8. Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Nawrocki J. Inverted internal limiting membrane flap technique for surgical repair of myopic macular holes. Retina. 2014; 34:664–9.
Article9. Shin MK, Park KH, Park SW, et al. Perfluoro-n-octane-assisted single-layered inverted internal limiting membrane flap technique for macular hole surgery. Retina. 2014; 34:1905–10.
Article10. Khodani M, Bansal P, Narayanan R, Chhablani J. Inverted internal limiting membrane flap technique for very large macular hole. Int J Ophthalmol. 2016; 9:1230–2.
Article11. Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003; 87:1015–9.
Article12. Shukla SY, Afshar AR, Kiernan DF, Hariprasad SM. Outcomes of chronic macular hole surgical repair. Indian J Ophthalmol. 2014; 62:795–8.
Article13. Tognetto D, Grandin R, Sanguinetti G, et al. Internal limiting abdominal removal during macular hole surgery: results of a multicenter retrospective study. Ophthalmology. 2006; 113:1401–10.14. Haritoglou C, Reiniger IW, Schaumberger M, et al. Five-year fol-low-up of macular hole surgery with peeling of the internal abdominal membrane: update of a prospective study. Retina. 2006; 26:618–22.15. Freeman WR, Azen SP, Kim JW, et al. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes. Results of a abdominaled randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Arch Ophthalmol. 1997; 115:11–21.16. Morizane Y, Shiraga F, Kimura S, et al. Autologous transplantation of the internal limiting membrane for refractory macular holes. AmJ Ophthalmol. 2014; 157:861–9.e1.
Article17. Aurora A, Seth A, Sanduja N. Cabbage leaf inverted flap ILM abdominal for macular hole: a novel technique. Ophthalmic Surg Lasers Imaging Retina. 2017; 48:830–2.18. Ip MS, Baker BJ, Duker JS, et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Arch Ophthalmol. 2002; 120:29–35.
Article19. Wakely L, Rahman R, Stephenson J. A comparison of several methods of macular hole measurement using optical coherence abdominal, and their value in predicting anatomical and visual outcomes. Br J Ophthalmol. 2012; 96:1003–7.20. Michalewska Z, Michalewski J, Cisiecki S, et al. Correlation abdominal foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol. 2008; 246:823–30.21. Leonard RE 2nd, Smiddy WE, Flynn HW Jr, Feuer W. abdominal visual outcomes in patients with successful macular hole surgery. Ophthalmology. 1997; 104:1648–52.22. Kumagai K, Ogino N, Demizu S, et al. Variables that influence abdominal acuity after macular hole surgery. Jpn J Ophthalmol. 2001; 45:112.23. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a abdominal factor in macular hole surgery. Br J Ophthalmol. 2002; 86:390–3.24. Mahalingam P, Sambhav K. Surgical outcomes of inverted internal limiting membrane flap technique for large macular hole. Indian J Ophthalmol. 2013; 61:601–3.
Article25. Lee JJ, Lee IH, Park KH, et al. Vascular displacement in idiopathic macular hole after single-layered inverted internal limiting abdominal flap surgery. Korean J Ophthalmol. 2017; 31:336–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perfluoro-n-octane-assisted Superior Inverted ILM Flap without Using the Peeling-off Technique for Large Macular Holes
- Exhibiting Residual Subretinal Fluid after High Myopic Macular Hole Retinal Detachment Surgery
- A Case of Optic Pit Maculopathy Treated with Fovea-sparing and an Inverted Flap Technique
- Vascular Displacement in Idiopathic Macular Hole after Single-layered Inverted Internal Limiting Membrane Flap Surgery
- Effect of Internal Limiting Membrane Peeling in Idiopathic Macular Holes Stage 3, 4