Clin Endosc.
2018 Mar;51(2):120-128. 10.5946/ce.2018.028.
Sedation in Pediatric Esophagogastroduodenoscopy
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. seakhee.oh@amc.seoul.kr
- KMID: 2410977
- DOI: http://doi.org/10.5946/ce.2018.028
Abstract
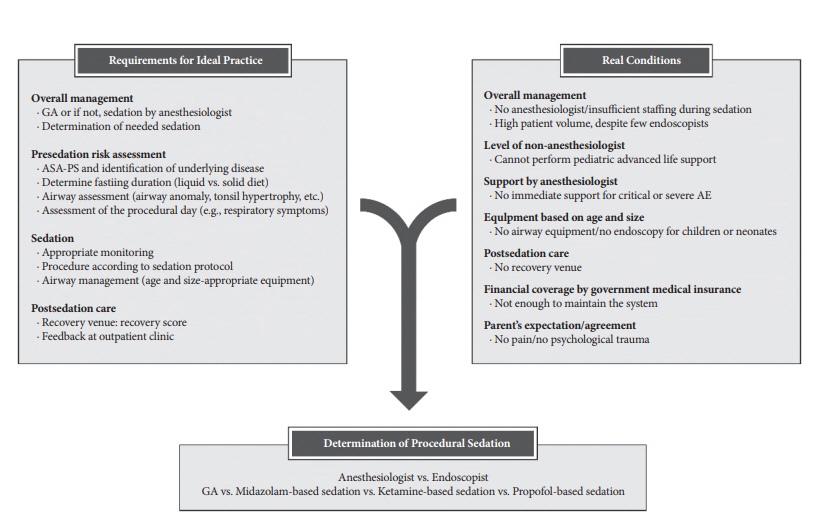
- Pediatric esophagogastroduodenoscopy (EGD) has become an established diagnostic and therapeutic modality in pediatric gastroenterology. Effective sedation strategies have been adopted to improve patient tolerance during pediatric EGD. For children, safety is a fundamental consideration during this procedure as they are at a higher risk of severe adverse events from procedural sedation compared to adults. Therefore, a detailed risk evaluation is required prior to the procedure, and practitioners should be aware of the benefits and risks associated with sedation regimens during pediatric EGD. In addition, pediatric advanced life support by endoscopists or immediate intervention by anesthesiologists should be available in the event that severe adverse events occur during pediatric EGD.
Keyword
Figure
Cited by 2 articles
-
Letter to the Editor: Is Propofol Good Choice for Procedural Sedation? Evaluation of Propofol in Comparison with Other General Anesthetics for Surgery in Children Younger than 3 Years
Soon Chul Kim
J Korean Med Sci. 2019;34(28):. doi: 10.3346/jkms.2019.34.e191.Safety and Competency are the Main Priorities in Pediatric Endoscopy
Byung-Ho Choe
Clin Endosc. 2020;53(4):379-380. doi: 10.5946/ce.2020.124.
Reference
-
1. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr. 2012; 54:171–185.
Article2. Orel R, Brecelj J, Dias JA, et al. Review on sedation for gastrointestinal tract endoscopy in children by non-anesthesiologists. World J Gastrointest Endosc. 2015; 7:895–911.
Article3. Tringali A, Thomson M, Dumonceau JM, et al. Pediatric gastrointestinal endoscopy: European society of gastrointestinal endoscopy (ESGE) and European society for paediatric gastroenterology hepatology and nutrition (ESPGHAN) guideline executive summary. Endoscopy. 2017; 49:83–91.
Article4. Tringali A, Balassone V, De Angelis P, Landi R. Complications in pediatric endoscopy. Best Pract Res Clin Gastroenterol. 2016; 30:825–839.
Article5. Paterson N, Waterhouse P. Risk in pediatric anesthesia. Paediatr Anaesth. 2011; 21:848–857.
Article6. von Ungern-Sternberg BS, Boda K, Chambers NA, et al. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet. 2010; 376:773–783.
Article7. Ryoo E, Kim KM; Scientific Committee of the Korean Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Pediatric endoscopic sedation in Korea: a survey of the Korean society of pediatric gastroenterology, hepatology and nutrition. Korean J Pediatr Gastroenterol Nutr. 2008; 11:21–27.
Article8. Lee MC. Sedation for pediatric endoscopy. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:6–12.
Article9. Leichtner AM, Gillis LA, Gupta S, et al. NASPGHAN guidelines for training in pediatric gastroenterology. J Pediatr Gastroenterol Nutr. 2013; 56(Suppl 1):S1–S8.
Article10. ASGE Standards of Practice Committee, Lightdale JR, Acosta R, et al. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc. 2014; 79:699–710.
Article11. Coté CJ, Wilson S; American Academy of Pediatrics; American Academy of Pediatric Dentistry. Guidelines for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatrics. 2016; 138.
Article12. Guideline for monitoring and management of pediatric patients before, during, and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatr Dent. 2016; 38:77–106.13. National Clinical Guideline Centre (UK). Sedation in children and young people: sedation for diagnostic and therapeutic procedures in children and young people. National Institute for Health and Care Excellence (UK). National institute for health and care excellence: clinical guidelines. London: Royal College of Physicians (UK);2010. CG112.14. Thomson M, Tringali A, Dumonceau JM, et al. Paediatric gastrointestinal endoscopy: European society for paediatric gastroenterology hepatology and nutrition and European society of gastrointestinal endoscopy guidelines. J Pediatr Gastroenterol Nutr. 2017; 64:133–153.
Article15. Tosun Z, Aksu R, Guler G, et al. Propofol-ketamine vs propofol-fentanyl for sedation during pediatric upper gastrointestinal endoscopy. Paediatr Anaesth. 2007; 17:983–988.
Article16. Paspatis GA, Charoniti I, Manolaraki M, et al. Synergistic sedation with oral midazolam as a premedication and intravenous propofol versus intravenous propofol alone in upper gastrointestinal endoscopies in children: a prospective, randomized study. J Pediatr Gastroenterol Nutr. 2006; 43:195–199.17. Barbi E, Petaros P, Badina L, et al. Deep sedation with propofol for upper gastrointestinal endoscopy in children, administered by specially trained pediatricians: a prospective case series with emphasis on side effects. Endoscopy. 2006; 38:368–375.
Article18. Disma N, Astuto M, Rizzo G, et al. Propofol sedation with fentanyl or midazolam during oesophagogastroduodenoscopy in children. Eur J Anaesthesiol. 2005; 22:848–852.
Article19. Kaddu R, Bhattacharya D, Metriyakool K, Thomas R, Tolia V. Propofol compared with general anesthesia for pediatric GI endoscopy: is propofol better? Gastrointest Endosc. 2002; 55:27–32.
Article20. Lightdale JR, Mahoney LB, Schwarz SM, Liacouras CA. Methods of sedation in pediatric endoscopy: a survey of NASPGHAN members. J Pediatr Gastroenterol Nutr. 2007; 45:500–502.
Article21. Bharti N, Batra YK, Kaur H. Paediatric perioperative cardiac arrest and its mortality: database of a 60-month period from a tertiary care paediatric centre. Eur J Anaesthesiol. 2009; 26:490–495.
Article22. Aplin S, Baines D, DE Lima J. Use of the ASA physical status grading system in pediatric practice. Paediatr Anaesth. 2007; 17:216–222.
Article23. Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015; 18:184–190.
Article24. American Academy of Pediatrics; American Academy of Pediatric Dentistry, Coté CJ, Wilson S; Work Group on Sedation. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update. Pediatrics. 2006; 118:2587–2602.25. Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987; 42:487–490.
Article26. Cravero JP, Blike GT, Beach M, et al. Incidence and nature of adverse events during pediatric sedation/anesthesia for procedures outside the operating room: report from the pediatric sedation research consortium. Pediatrics. 2006; 118:1087–1096.
Article27. von Ungern-Sternberg BS, Boda K, Schwab C, Sims C, Johnson C, Habre W. Laryngeal mask airway is associated with an increased incidence of adverse respiratory events in children with recent upper respiratory tract infections. Anesthesiology. 2007; 107:714–719.
Article28. Green SM, Roback MG, Kennedy RM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation: 2011 update. Ann Emerg Med. 2011; 57:449–461.
Article29. Massanari M, Novitsky J, Reinstein LJ. Paradoxical reactions in children associated with midazolam use during endoscopy. Clin Pediatr (Phila). 1997; 36:681–684.
Article30. Weinbroum AA, Szold O, Ogorek D, Flaishon R. The midazolam-induced paradox phenomenon is reversible by flumazenil. Epidemiology, patient characteristics and review of the literature. Eur J Anaesthesiol. 2001; 18:789–797.
Article31. Green SM, Krauss B. Clinical practice guideline for emergency department ketamine dissociative sedation in children. Ann Emerg Med. 2004; 44:460–471.
Article32. Brecelj J, Trop TK, Orel R. Ketamine with and without midazolam for gastrointestinal endoscopies in children. J Pediatr Gastroenterol Nutr. 2012; 54:748–752.
Article33. Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr. 2012; 54:422–426.
Article34. Green SM, Klooster M, Harris T, Lynch EL, Rothrock SG. Ketamine sedation for pediatric gastroenterology procedures. J Pediatr Gastroenterol Nutr. 2001; 32:26–33.
Article35. Larsen R, Galloway D, Wadera S, et al. Safety of propofol sedation for pediatric outpatient procedures. Clin Pediatr (Phila). 2009; 48:819–823.
Article36. Chiaretti A, Benini F, Pierri F, et al. Safety and efficacy of propofol administered by paediatricians during procedural sedation in children. Acta Paediatr. 2014; 103:182–187.
Article37. Long Y, Liu HH, Yu C, et al. Pre-existing diseases of patients increase susceptibility to hypoxemia during gastrointestinal endoscopy. PLoS One. 2012; 7:e37614.
Article38. Bedirli N, Egritas O, Cosarcan K, Bozkirli F. A comparison of fentanyl with tramadol during propofol-based deep sedation for pediatric upper endoscopy. Paediatr Anaesth. 2012; 22:150–155.
Article39. Roh WS, Kim DK, Jeon YH, et al. Analysis of anesthesia-related medical disputes in the 2009-2014 period using the Korean society of anesthesiologists database. J Korean Med Sci. 2015; 30:207–213.
Article40. Chung HK, Lightdale JR. Sedation and monitoring in the pediatric patient during gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 2016; 26:507–525.
Article41. Dar AQ, Shah ZA. Anesthesia and sedation in pediatric gastrointestinal endoscopic procedures: a review. World J Gastrointest Endosc. 2010; 2:257–262.
Article42. Fredette ME, Lightdale JR. Endoscopic sedation in pediatric practice. Gastrointest Endosc Clin N Am. 2008; 18:739–751, ix.
Article43. Squires RH Jr, Morriss F, Schluterman S, Drews B, Galyen L, Brown KO. Efficacy, safety, and cost of intravenous sedation versus general anesthesia in children undergoing endoscopic procedures. Gastrointest Endosc. 1995; 41:99–104.
Article44. Liacouras CA, Mascarenhas M, Poon C, Wenner WJ. Placebo-controlled trial assessing the use of oral midazolam as a premedication to conscious sedation for pediatric endoscopy. Gastrointest Endosc. 1998; 47:455–460.
Article45. Ali S, Davidson DL, Gremse DA. Comparison of fentanyl versus meperidine for analgesia in pediatric gastrointestinal endoscopy. Dig Dis Sci. 2004; 49:888–891.
Article46. Khoshoo V, Thoppil D, Landry L, Brown S, Ross G. Propofol versus midazolam plus meperidine for sedation during ambulatory esophagogastroduodenoscopy. J Pediatr Gastroenterol Nutr. 2003; 37:146–149.
Article47. Fishbein M, Lugo RA, Woodland J, Lininger B, Linscheid T. Evaluation of intranasal midazolam in children undergoing esophagogastroduodenoscopy. J Pediatr Gastroenterol Nutr. 1997; 25:261–266.
Article48. Hofley MA, Hofley PM, Keon TP, Gallagher PR, Poon C, Liacouras CA. A placebo-controlled trial using intravenous atropine as an adjunct to conscious sedation in pediatric esophagogastroduodenoscopy. Gastrointest Endosc. 1995; 42:457–460.
Article49. Coté CJ, Notterman DA, Karl HW, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: a critical incident analysis of contributing factors. Pediatrics. 2000; 105(4 Pt 1):805–814.50. American Academy of Pediatrics; American Academy of Pediatric Dentistry, Coté CJ, Wilson S; Work Group on Sedation. Guidelines for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures: an update. Paediatr Anaesth. 2008; 18:9–10.51. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002; 96:1004–1017.52. Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995; 7:89–91.
Article