J Korean Soc Echocardiogr.
1994 Jul;2(1):23-31. 10.4250/jkse.1994.2.1.23.
Intravascular Ultrasonic Comparison of the Arterial Remodeling after Directional Coronary Atherectomy and Mechanical Rotational Atherectomy
- Affiliations
-
- 1Department of Internal Medicine, Wonju College of Medicine, Yonsei University, Wonju, Korea.
- 2Washington Cardiology Center, Washington D.C., USA.
- KMID: 2410456
- DOI: http://doi.org/10.4250/jkse.1994.2.1.23
Abstract
- BACKGROUND
Directional coronary atherectomy(DCA) and mechanical rotational atherectomy(ROTA) were desinged to remove part of the obstructive tissue of atherosclerotic lesion. But, two devices have th different mechanisms of improving stenotic lesions. DCA procedure has the effects of tissue removal and some dilative effect from the large profile of the device and supporting balloon, and ROTA has the effect to increase lumen by abrading the atherosclerotic plaque into particulate debris. It is not clear at present what is more effective procedure for tissue removal, acute gain and long term results. To identify these facts, we assessed the differences of arterial and plaque remodeling between the patients treated with DCA and ROTA.
METHODS
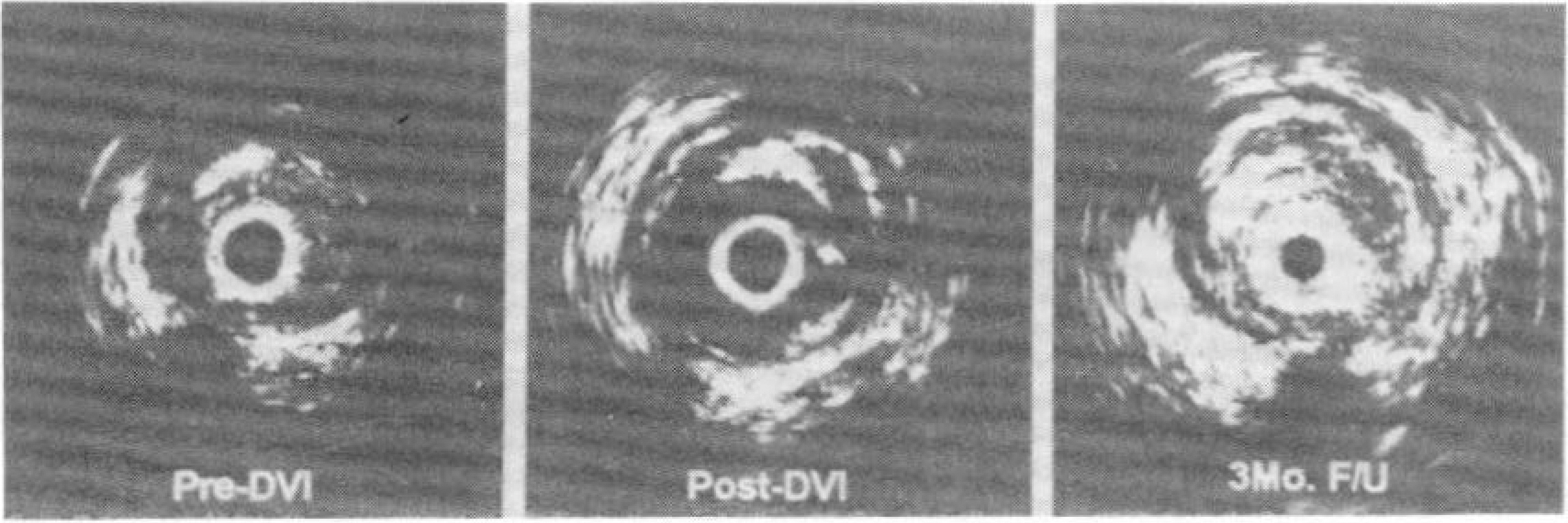
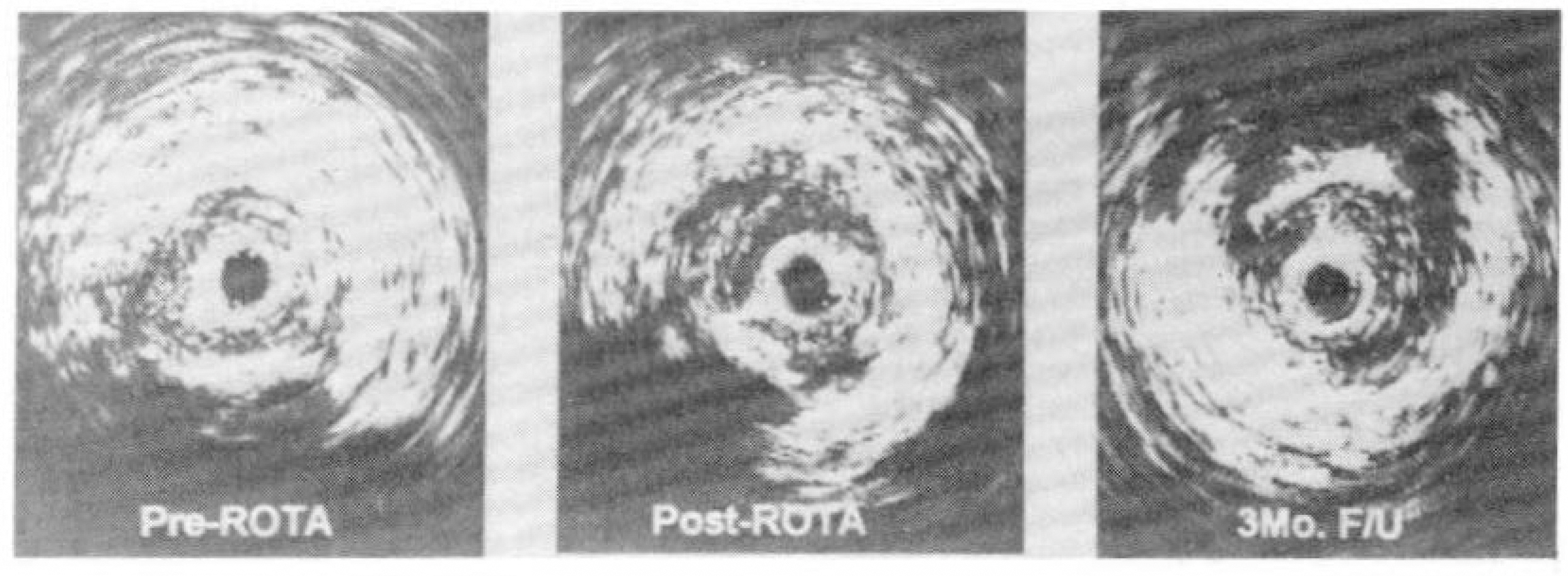
We used a comprehensive intravascular ultrasound imaging system(25MHz rotating transducer, 3.9 Fr monorail imaging sheath, motorized transducer pullback at 0.5mm/sec, and quantification) to study 32 patients(DCA : 1 left main, 12 LAD, 2 LCX, 7 RCA and ROTA : 6 LAD, 1 LCX, 3 RCA) before, immediately after DCA and ROTA, and follow-up. Before, after DCA and ROTA, and follow-up image slices were analysed ; and the cross-sectional area(CSA) of external clastic memvrane(EEM). lumen and plaque+media(P+M) were measured.
RESULTS
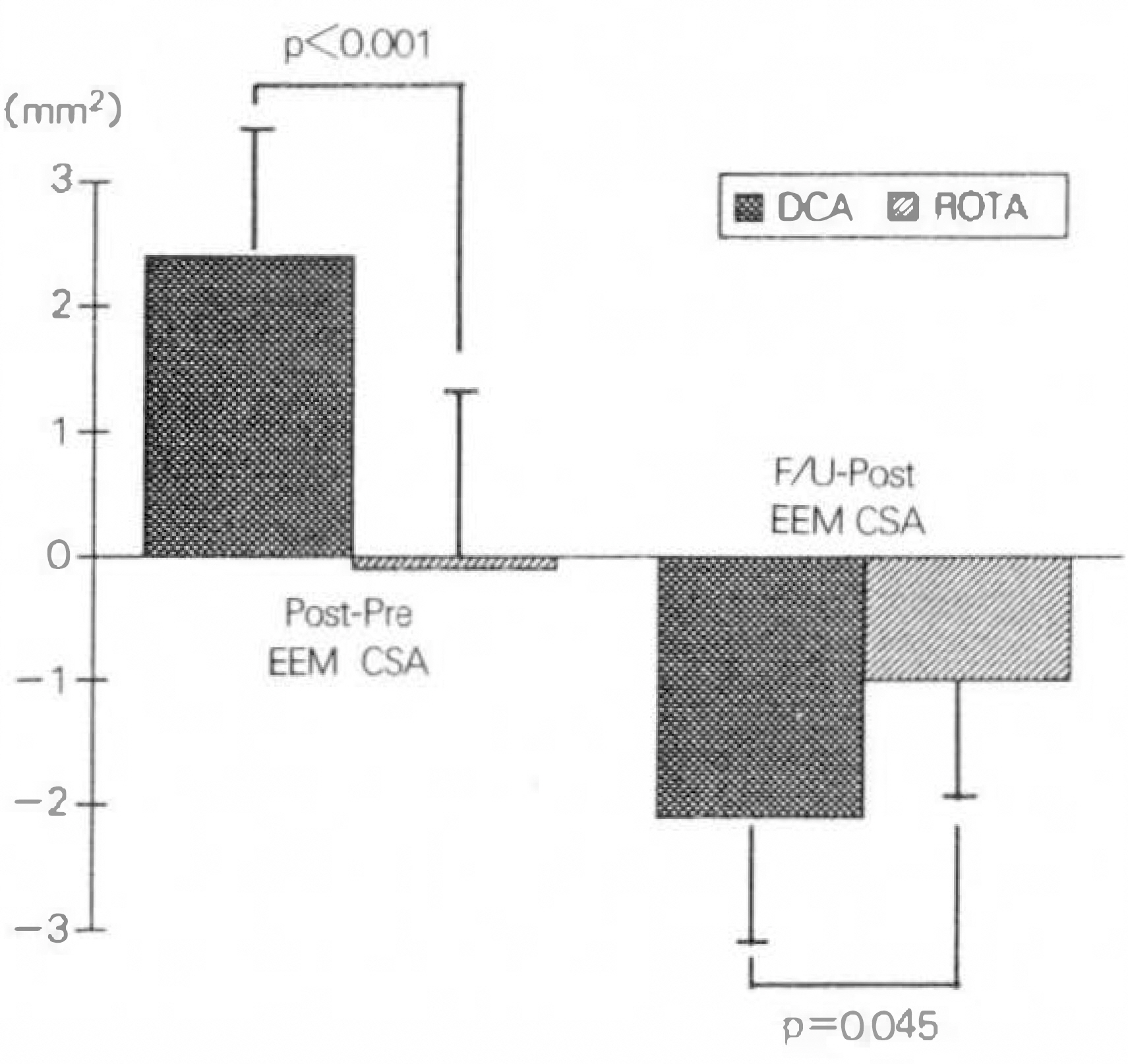
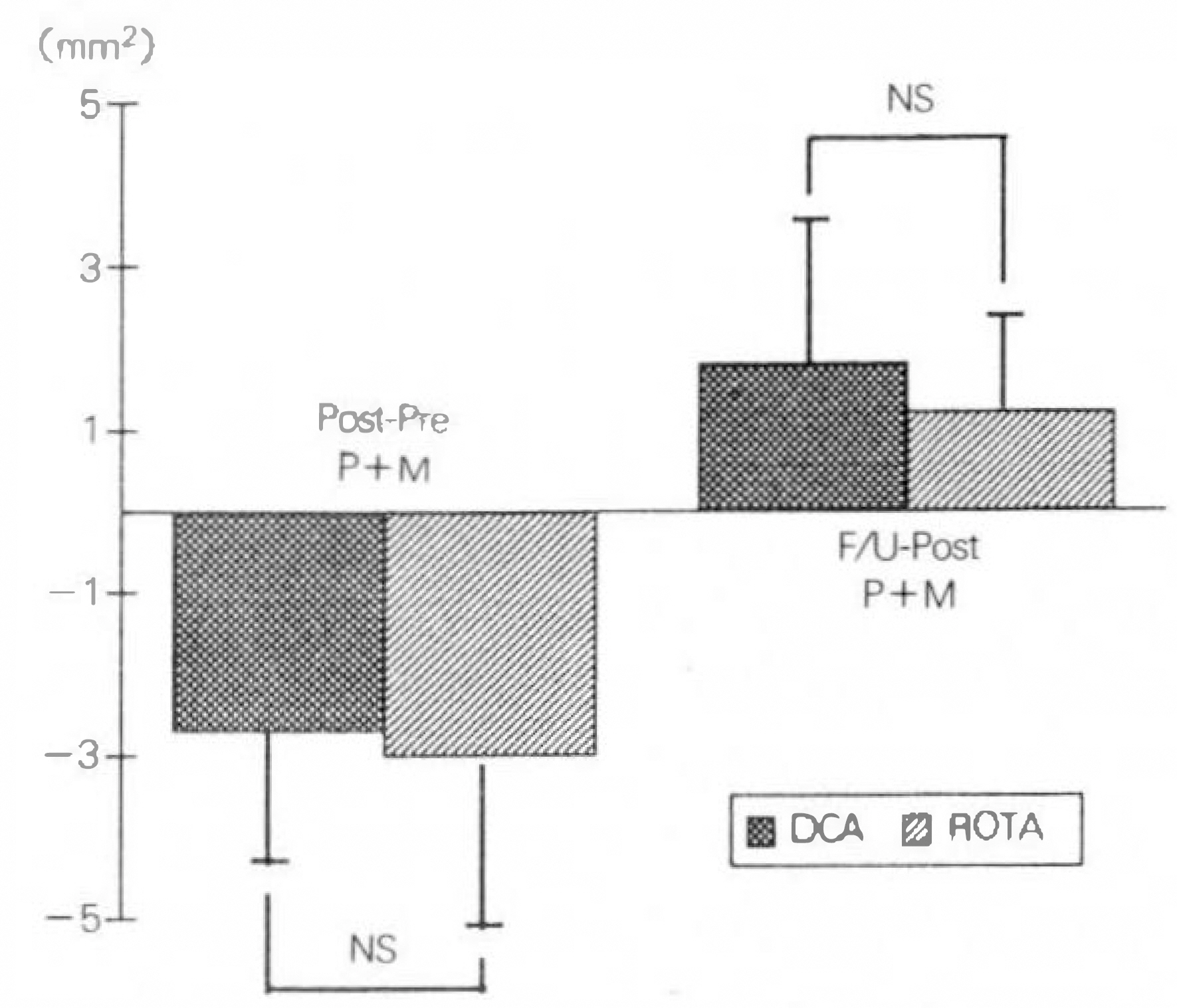
1) Before intervention, there were no significant differences of EEM-CSA, lumen CSA and P+M CSA(EEN-CSA : 17.3±5.6mm2 in DCA v.s 15.0±2.9mm2 in ROTA, lumen CSA : 1.5±0.3mm2 in DCA v.s 1.6±0.5mm2 in ROTA, P+M CSA : 15.8±5.6mm2 in DCA v.s 13.4±3.1mm2 in ROTA). 2) Immediately after intervention, there were significant differences of EEM-CSA and lumen CSA(EEM CSA : 20.1±5.2mm2 in DCA v.s 14.9±2.2mm2 in ROTA, Lumen CSA : 6.3±1.4mm2 in DCA v.s 4.2±1.2mm2 in ROTA)(p=0.001). But, no significant difference was noted in P+M CSA between two groups(13.9±5.2mm2 v.s 10.6±1.6mm2). 3) During follow-up, there were significant differences of EEM-CSA(18.7±5.4mm2 in DCA v.s 14.8±2.3mm2 in ROTA) and P+M CSA(15.7±5.6mm2 in DCA v.s 11.8±1.9mm2 in ROTA)(p=0.008). But, no significant difference was shown in lumen CSA(2.8±1.3mm2 v.s 2.9±1.5mm2 in ROTA).
CONCLUSIONS
DCA is more effecitive to get the large "acute gain" than ROTA. There was no differene of luminal area between the two groups at follow-up because of larger "chronic recoil" and "intimal hyperplasia" in DCA treated patients than ROTA.
Keyword
MeSH Terms
Figure
Reference
-
References
1). Gruentzig AR, Senning A, Siegenthaler WE. Nonoperative dilataton of coronary artery stenosis: percutaneous transluminal coronary angioplasty. N Engl J Med. 301:61. 1979.2). Detre KM, Holubkov R, Kelsey SF, Co-investigators of the NHLBI PTCA Registry. Percutaneous transluminal coronary angioplasty in 1985 – 1986 and 1977–1981. N Engl J Med. 318:265. 1988.3). Holme DR, Holubkov R, Vlietstra RE, Kelsey SF, Reeder GS, Dorros G, Williams DO, Cowley MJ, Faxon DP, Kent KM, Bentivoglio LG, Detre KM. Comparison of complication during percutaneous transluminal coronary angioplasty from 1977–1981 and from 1985 – 1986: the NHLBI PTCA Registry. J Am Coll Cardiol. 12:1149. 1988.4). Ellis SG, Roubin GS, King SB III, Douglas S, Weintraub G, Cox WS. Angiographic and clinical predictors of acute closure after native vessel coronary angioplasty. Circulation. 77:372. 1988.
Article5). King SB III, Schlumpf M. Ten-year completed follow-up of percutaneous transluminal coronary angioplasty: the early Zurich experience. J Am Coll Cardiol. 22:353. 1993.
Article6). Gershlick A, Brack MJ, More RS, Syndercombe-Court D, Balcon R. Angiographic restenosis after angioplasty: comparison of definitions and correlation with clinical outcome. Coronart Artery Disease. 4:73. 1993.7). Safian RD, Bairn DS. New devices for coronary intervention: intravascular stents and coronary atherectomy catheters. Cardiac catheterization, angiography, and intervention. Grossman W, Bairn DS, editors. 3rd Ed.p. 467. Philadelphia: Lea & Febiger;1991.8). Phillips HR III, Davidson CJ, Hinohara T, Simpson JB, Berdan LG. Directional coronary atherectomy. Interventional cardiovascular medicine. Roubin , editor. p. 789. New York: Churchill Livingstone;1994.9). Hansen DD, Auth DC, Vrocko R, Ritchie JL. Rotational atherectomy in atherosclerotic rabbit iliac arteries. Am Heart J. 115:160. 1988.
Article10). Bertrand ME, Bauters C, Lablanche JM. Percutaneous coronary rotational angioplasty with the Rotablator. Textbook of interventional cardiology. Topol EJ, editor. 2nd Ed. p. 659. Philadelphia: WB Saunders Co.;1994.11). Mintz GS, Douek P, Pichard AD, Kent KM, Satler LF, Popma JJ, Leon MB. Target lesion calcification in coronary artery disease: An intavascular ultrasound study. J Am Coll Cardiol. 20:1149. 1992.12). Coy KM, Maurer G, Siegel RJ. Intravascular ultrasound imaging: A current perspective. J Am Coll Cardiol. 18:1811. 1991.
Article13). Kovach JA, Mintz GS, Pichard AD, Kent KM, Popma JJ, Satler LF, Leon MB. Sequential intravascular ultrasound characterization of the mechanism of rotational atherectomy and ajunctive balloon angioplasty. J Am Coll Cardiol. 22:1024. 1993.14). Portkin BN, Bartorelli AL, Gessert JM, Neville RF, Almagor Y, Roberts WC, Leon MB. Coronary artery imaging with intravascular high-frequency ultrasound. Circulation. 81:1575. 1990.
Article15). Simpson JB, Johnson DE, Thapliyal HV, Marks DM, Braden LJ. Transluminal atherectomy: a new approach to the treatment of atherosclerotic vascular disease(abstr). Circulation. 72(suppl III):III–111. 1985.16). Penny WF, Schmidt DA, Safian RD, Erny RE, Baim DS. Insights into the mechanism of luminal improvement after directional coronary atherectomy. Am J Cardiol. 67:435. 1991.
Article17). Tenaglia AN, Buller CE, Kisslo KB, Stack RS, Davidson CJ. Mechanisms of balloon angioplasty and directional coronary atherectomy as assessed by intracoronary ultrasound. J Am Coll Cardiol. 20:685. 1992.
Article18). Ahn SS, Auth DC, Marcus DR, Moore WS. Removal of focal atheromatous lesions by angioscopically guided high speed rotary atherectomy. J Vasc Surg. 7:292. 1988.19). Safian RD, Gelbfish JS, Erny RE, Schnitt SJ, Schmidt DA, Bairn DS. Coronary atherectomy. Clinical, angiographic, and histologic findings and observations regarding potential mechanisms. Circulation. 82:69. 1990.20). Garratt KN, Holmes DR Jr., Bell MR, Bresnahan JF, Kaufmann UP, Vlietstra RE, Edwards WD. Restenosis after directional coronary atherectomy: differences between primary atheromatous and restenosis lesions and influence of subintimal tissue resection. J Am Coll Cardiol. 1665:1990.21). Bertrand ME, Lablanche JM, Leroy F, Bauters C, De Jaegere P, Serruys PW, Meyer J, Dietz U, Erbel R. Percutaneous transluminal coronary rotatonal ablation with Rotablator(European experience). Am J Cardiol. 69:470. 1992.22). Buchbinder M, Leon MB, Warth D, et al. Multi-center registry of percutaneous coronary rotatonal ablation using the Rotablator(abstr). J Am Coll Cardiol. 19:332A. 1992.23). Umans VAWM, Beatt KJ, Rensing BJWM, et al. Comparative quantitative angiographic analysis of directional coronary atherectomy and balloon coronary angioplasty. Am J Cardiol. 68:1556. 1991.
Article24). Kovach JA, Mintz GS, Kent KM, Pichard AD, Salter LF, Popma JJ, Leon MB. Serial intravascular ultasound studies indicate that chronic recoil is an important mechanism of restenosis following transcatheter therapy. J Am Coll Cardiol. 21:1993.25). Pichard AD, Mintz GS, Kent KM, Satler LF, Popma JJ, Leon MB. Transcatheter device synergy: preliminary experience with adjunct directional atherectomy following rotational atherectomy in treating calcific coronary artery disease(abstr). J Am Coll Cardiol. 21:227A. 1993.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience in High Speed Rotational Coronary Atherectomy
- Rotational Atherectomy through Inner Guiding Catheter System for 1.25 mm Rotational Burr Non-Crossable Heavily Calcified Coronary Stenosis
- Early and Late Clinical Outcomes after Directional Coronary Atherectomy
- Directional Coronary Atherectomy (Simpson AtheroCath) : Reasons for Device Selection, Angiographic and Histologic Findings, and Its Mechanisms
- Initial Experience of Rotational Atherectomy in Coronary Artery Disease