J Clin Neurol.
2018 Apr;14(2):141-152. 10.3988/jcn.2018.14.2.141.
The Influence of Sex in Stroke Thrombolysis: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Neurology, the First Affiliated Hospital of Chongqing Medical University, Chongqing, China. liguangqin@tom.com
- KMID: 2407939
- DOI: http://doi.org/10.3988/jcn.2018.14.2.141
Abstract
- BACKGROUND AND PURPOSE
There is increasing recognition of the importance of stroke in females to both clinical and public health. The natural course of stroke is worse in females than in males, but the evidence regarding sex disparities in the responses to thrombolysis in stroke patents is still controversial. We compared outcomes after thrombolysis treatment between females and males.
METHODS
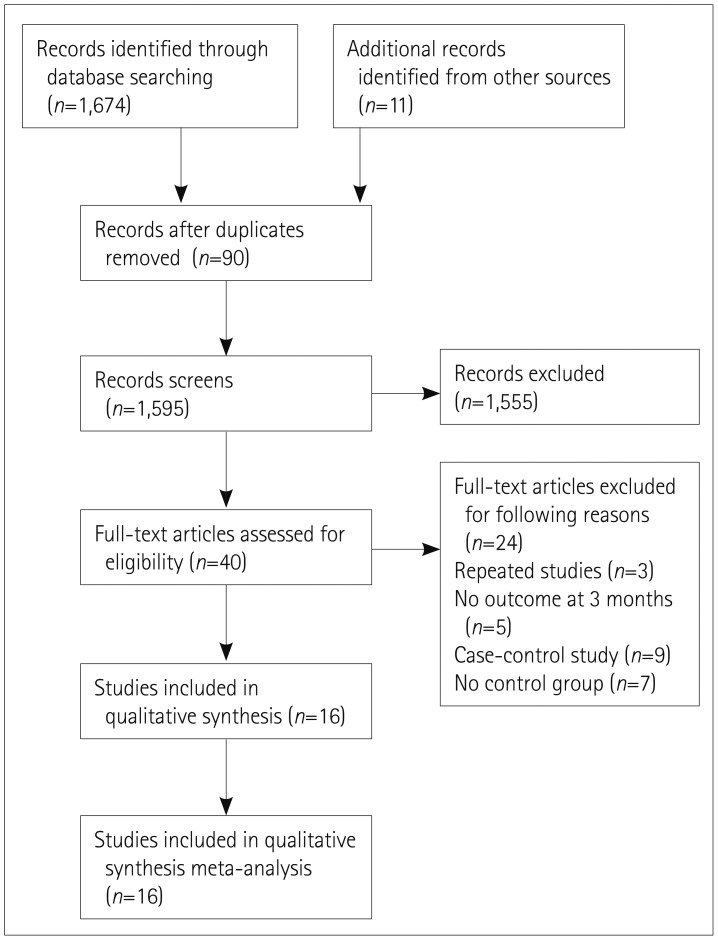
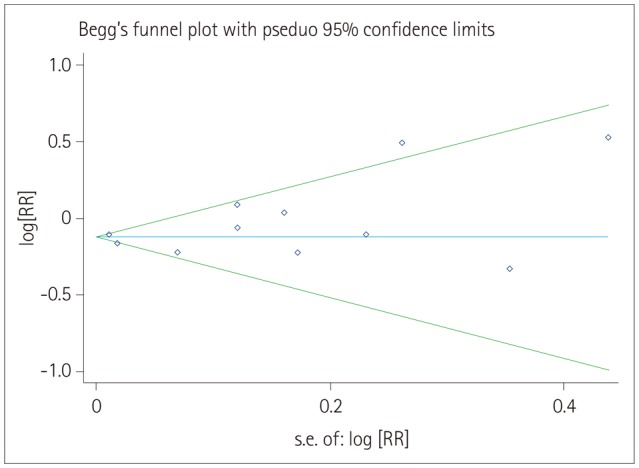
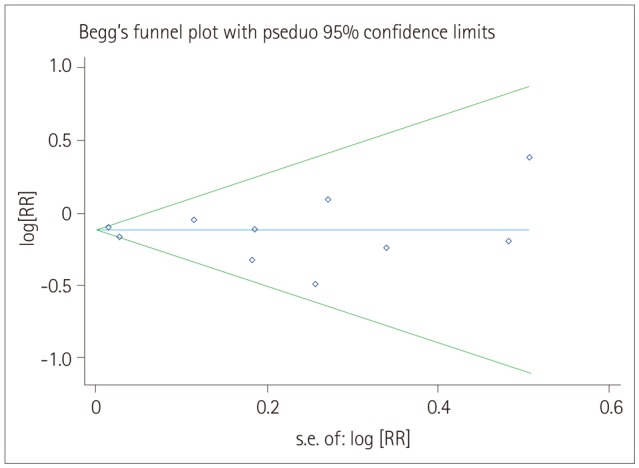
Clinical trials reported in the Embase, PubMed, and Cochrane Library electronic databases up to March 13, 2017 were included in this analysis. Two reviewers independently extracted the data and conducted quality assessments. Statistical tests were performed to check for heterogeneity and publication bias. Sensitivity analysis was also performed to evaluate the stability of the conclusions.
RESULTS
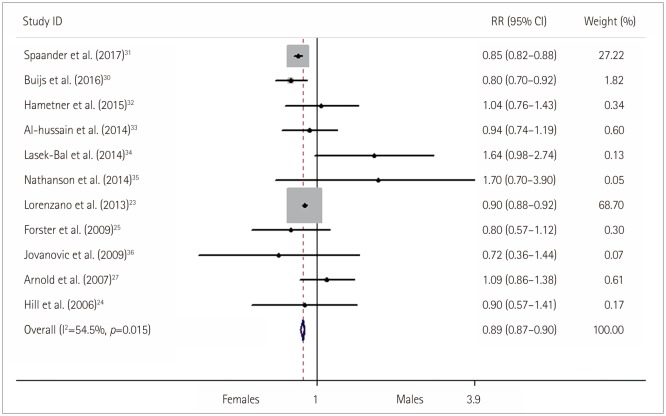
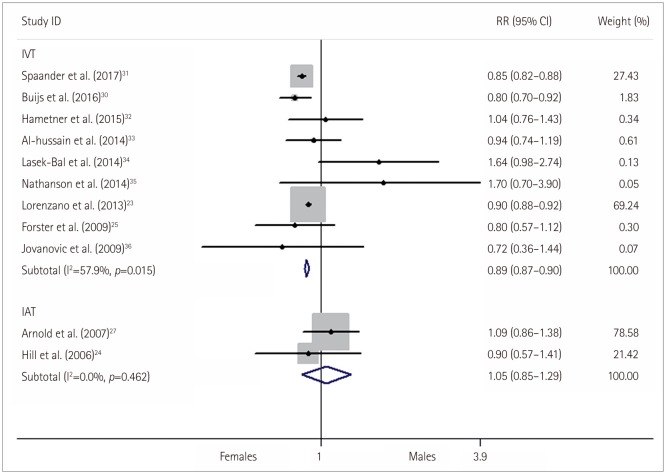
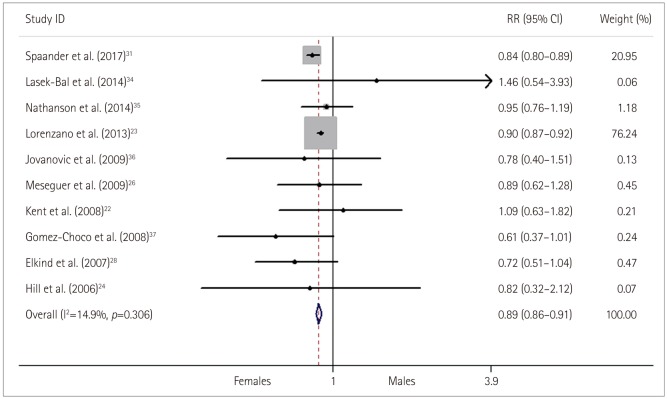
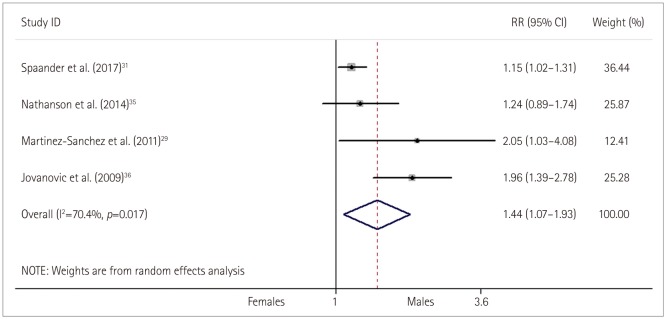
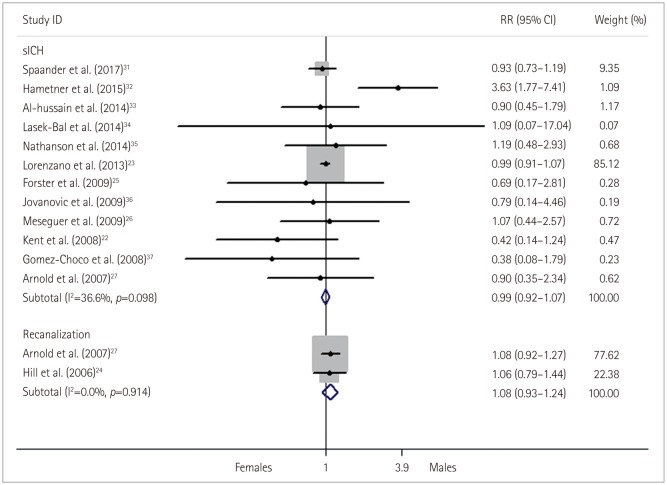
Sixteen reports involving 60,159 patients were available for analysis. The female patients were a 0.89-fold [95% confidence interval (CI)=0.87-0.90, p < 0.001], 0.89-fold (95% CI=0.87-0.91, p < 0.001), and 1.24-fold (95% CI=1.11-1.36, p < 0.001) more likely to obtain good, excellent, and poor functional outcomes, respectively, with no significant difference in the complications of symptomatic intracranial hemorrhage among the sexes [risk ratios (RR)=0.99, 95% CI=0.92-1.07, p=0.81] after thrombolysis treatment. In addition, the prevalence of a good functional outcome did not differ significantly between females and males in the intra-arterial thrombolysis (IAT) group (RR=1.05, 95% CI=0.85-1.29, p=0.67) in a subgroup analysis.
CONCLUSIONS
This study has demonstrated that females often exhibit a worse outcome than males after intravenous thrombolysis (IVT), whereas no relevant sex differences were found in outcome or recanalization after IAT, with safety regarding hemorrhage complications from thrombolysis being the same for the sexes. However, IVT should not be withheld from female stroke patients solely based on their sex before the findings are confirmed in further large-scale research.
Keyword
MeSH Terms
Figure
Reference
-
1. Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008; 7:915–926. PMID: 18722812.
Article2. Bushnell CD, Hurn P, Colton C, Miller VM, del Zoppo G, Elkind MS, et al. Advancing the study of stroke in women: summary and recommendations for future research from an NINDS-Sponsored Multidisciplinary Working Group. Stroke. 2006; 37:2387–2399. PMID: 16857945.3. Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke. 2009; 40:1032–1037. PMID: 19211484.
Article4. Niewada M, Kobayashi A, Sandercock PA, Kamiński B, Członkowska A. International Stroke Trial Collaborative Group. Influence of gender on baseline features and clinical outcomes among 17,370 patients with confirmed ischaemic stroke in the international stroke trial. Neuroepidemiology. 2005; 24:123–128. PMID: 15637449.
Article5. Reeves MJ, Fonarow GC, Zhao X, Smith EE, Schwamm LH. Get With The Guidelines-Stroke Steering Committee & Investigators. Quality of care in women with ischemic stroke in the GWTG program. Stroke. 2009; 40:1127–1133. PMID: 19211482.
Article6. Roquer J, Campello AR, Gomis M. Sex differences in first-ever acute stroke. Stroke. 2003; 34:1581–1585. PMID: 12805490.
Article7. Glader EL, Stegmayr B, Norrving B, Terént A, Hulter-Asberg K, Wester PO, et al. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003; 34:1970–1975. PMID: 12855818.8. Reid JM, Dai D, Gubitz GJ, Kapral MK, Christian C, Phillips SJ. Gender differences in stroke examined in a 10-year cohort of patients admitted to a Canadian teaching hospital. Stroke. 2008; 39:1090–1095. PMID: 18292386.
Article9. Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG. Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke. 2001; 32:1832–1840. PMID: 11486113.
Article10. Deng YZ, Reeves MJ, Jacobs BS, Birbeck GL, Kothari RU, Hickenbottom SL, et al. IV tissue plasminogen activator use in acute stroke: experience from a statewide registry. Neurology. 2006; 66:306–312. PMID: 16476927.
Article11. Reeves M, Bhatt A, Jajou P, Brown M, Lisabeth L. Sex differences in the use of intravenous rt-PA thrombolysis treatment for acute ischemic stroke: a meta-analysis. Stroke. 2009; 40:1743–1749. PMID: 19228855.12. Kapral MK, Devon J, Winter AL, Wang J, Peters A, Bondy SJ. Gender differences in stroke care decision-making. Med Care. 2006; 44:70–80. PMID: 16365615.
Article13. Turtzo LC, McCullough LD. Sex differences in stroke. Cerebrovasc Dis. 2008; 26:462–474. PMID: 18810232.
Article14. Gargano JW, Wehner S, Reeves MJ. Do presenting symptoms explain sex differences in emergency department delays among patients with acute stroke. Stroke. 2009; 40:1114–1120. PMID: 19211483.
Article15. Kapral MK, Fang J, Hill MD, Silver F, Richards J, Jaigobin C, et al. Sex differences in stroke care and outcomes: results from the Registry of the Canadian Stroke Network. Stroke. 2005; 36:809–814. PMID: 15731476.16. Niewada M, Kobayashi A, Sandercock PA, Kamiński B, Członkowska A. International Stroke Trial Collaborative Group. Influence of gender on baseline features and clinical outcomes among 17,370 patients with confirmed ischaemic stroke in the international stroke trial. Neuroepidemiology. 2005; 24:123–128. PMID: 15637449.
Article17. Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Basile AM, Wolfe CD, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003; 34:1114–1119. PMID: 12690218.18. Bousser MG. Stroke in women: the 1997 Paul Dudley White International Lecture. Circulation. 1999; 99:463–467. PMID: 9927389.19. Holroyd-Leduc JM, Kapral MK, Austin PC, Tu JV. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000; 31:1833–1837. PMID: 10926943.
Article20. Sturm JW, Donnan GA, Dewey HM, Macdonell RA, Gilligan AK, Srikanth V, et al. Quality of life after stroke: the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2004; 35:2340–2345. PMID: 15331799.21. Kent DM, Price LL, Ringleb P, Hill MD, Selker HP. Sex-based differences in response to recombinant tissue plasminogen activator in acute ischemic stroke: a pooled analysis of randomized clinical trials. Stroke. 2005; 36:62–65. PMID: 15569865.22. Kent DM, Buchan AM, Hill MD. The gender effect in stroke thrombolysis: of CASES, controls, and treatment-effect modification. Neurology. 2008; 71:1080–1083. PMID: 18495951.
Article23. Lorenzano S, Ahmed N, Falcou A, Mikulik R, Tatlisumak T, Roffe C, et al. Does sex influence the response to intravenous thrombolysis in ischemic stroke?: answers from safe implementation of treatments in Stroke-International Stroke Thrombolysis Register. Stroke. 2013; 44:3401–3406. PMID: 24172579.24. Hill MD, Kent DM, Hinchey J, Rowley H, Buchan AM, Wechsler LR, et al. Sex-based differences in the effect of intra-arterial treatment of stroke: analysis of the PROACT-2 study. Stroke. 2006; 37:2322–2325. PMID: 16888269.25. Förster A, Gass A, Kern R, Wolf ME, Ottomeyer C, Zohsel K, et al. Gender differences in acute ischemic stroke: etiology, stroke patterns and response to thrombolysis. Stroke. 2009; 40:2428–2432. PMID: 19461021.26. Meseguer E, Mazighi M, Labreuche J, Arnaiz C, Cabrejo L, Slaoui T, et al. Outcomes of intravenous recombinant tissue plasminogen activator therapy according to gender: a clinical registry study and systematic review. Stroke. 2009; 40:2104–2110. PMID: 19372440.27. Arnold M, Kappeler L, Nedeltchev K, Brekenfeld C, Fischer U, Keserue B, et al. Recanalization and outcome after intra-arterial thrombolysis in middle cerebral artery and internal carotid artery occlusion: does sex matter. Stroke. 2007; 38:1281–1285. PMID: 17332466.28. Elkind MS, Prabhakaran S, Pittman J, Koroshetz W, Jacoby M, Johnston KC. GAIN Americas Investigators. Sex as a predictor of outcomes in patients treated with thrombolysis for acute stroke. Neurology. 2007; 68:842–848. PMID: 17353472.
Article29. Martínez-Sánchez P, Fuentes B, Alonso de, Masjuan J, Simal P, Egido J, et al. Female gender is a factor of worse outcome in acute stroke even after thrombolytic treatment. Int J Stroke. 2011; 6:371–372.
Article30. Buijs JE, Uyttenboogaart M, Brouns R, de Keyser J, Kamphuisen PW, Luijckx GJ. The effect of age and sex on clinical outcome after intravenous recombinant tissue plasminogen activator treatment in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis. 2016; 25:312–316. PMID: 26527412.
Article31. Spaander FH, Zinkstok SM, Baharoglu IM, Gensicke H, Polymeris A, Traenka C, et al. Sex differences and functional outcome after intravenous thrombolysis. Stroke. 2017; 48:699–703. PMID: 28143921.
Article32. Hametner C, Kellert L, Ringleb PA. Impact of sex in stroke thrombolysis: a coarsened exact matching study. BMC Neurol. 2015; 15:10. PMID: 25855102.
Article33. Al-hussain F, Hussain MS, Molina C, Uchino K, Shuaib A, Demchuk AM, et al. Does the sex of acute stroke patients influence the effectiveness of rt-PA? BMC Neurol. 2014; 14:60. PMID: 24669960.
Article34. Lasek-Bal A, Puz P, Kazibutowska Z. Efficacy and safety assessment of alteplase in the treatment of stroke-gender differences. Neurol Res. 2014; 36:851–856. PMID: 24620981.35. Nathanson D, Patrone C, Nyström T, von Euler M. Sex, diastolic blood pressure, and outcome after thrombolysis for ischemic stroke. Stroke Res Treat. 2014; 2014:747458. PMID: 25302134.
Article36. Jovanović DR, Beslać-Bumbasirević Lj, Budimkić M, Pekmezović T, Zivković M, Kostić VS. Do women benefit more from systemic thrombolysis in acute ischemic stroke? A Serbian experience with thrombolysis in ischemic stroke (SETIS) study. Clin Neurol Neurosurg. 2009; 111:729–732. PMID: 19647928.
Article37. Gómez-Choco M, Obach V, Urra X, Amaro S, Cervera A, Vargas M, et al. The response to IV rt-PA in very old stroke patients. Eur J Neurol. 2008; 15:253–256. PMID: 18190509.
Article38. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 333:1581–1587. PMID: 7477192.39. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet. 1998; 352:1245–1251. PMID: 9788453.40. Wahlgren N, Ahmed N, Dávalos A, Ford GA, Grond M, Hacke W, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): an observational study. Lancet. 2007; 369:275–282. PMID: 17258667.
Article41. Kain K, Carter AM, Bamford JM, Grant PJ, Catto AJ. Gender differences in coagulation and fibrinolysis in white subjects with acute ischemic stroke. J Thromb Haemost. 2003; 1:390–392. PMID: 12871521.
Article42. Kain K, Catto AJ, Carter AM, Young J, Bamford J, Bavington J, et al. Decreased fibrinolytic potential in South Asian women with ischaemic cerebrovascular disease. Br J Haematol. 2001; 114:155–161. PMID: 11472361.
Article43. Ribo M, Montaner J, Molina CA, Arenillas JF, Santamarina E, Alvarez-Sabín J. Admission fibrinolytic profile predicts clot lysis resistance in stroke patients treated with tissue plasminogen activator. Thromb Haemost. 2004; 91:1146–1151. PMID: 15175801.
Article44. Savitz SI, Schlaug G, Caplan L, Selim M. Arterial occlusive lesions recanalize more frequently in women than in men after intravenous tissue plasminogen activator administration for acute stroke. Stroke. 2005; 36:1447–1451. PMID: 15947268.
Article45. De Silva DA, Ebinger M, Davis SM. Gender issues in acute stroke thrombolysis. J Clin Neurosci. 2009; 16:501–504. PMID: 19201193.
Article46. Mazighi M, Serfaty JM, Labreuche J, Laissy JP, Meseguer E, Lavallée PC, et al. Comparison of intravenous alteplase with a combined intravenous-endovascular approach in patients with stroke and confirmed arterial occlusion (RECANALISE study): a prospective cohort study. Lancet Neurol. 2009; 8:802–809. PMID: 19647488.
Article47. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA;. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009; 73:1066–1072. PMID: 19786699.
Article48. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014; 384:1929–1935. PMID: 25106063.
Article49. Mazighi M, Chaudhry SA, Ribo M, Khatri P, Skoloudik D, Mokin M, et al. Impact of onset-to-reperfusion time on stroke mortality: a collaborative pooled analysis. Circulation. 2013; 127:1980–1985. PMID: 23671178.50. Yang SH, Shi J, Day AL, Simpkins JW. Estradiol exerts neuroprotective effects when administered after ischemic insult. Stroke. 2000; 31:745–749. PMID: 10700514.
Article51. Liao S, Chen W, Kuo J, Chen C. Association of serum estrogen level and ischemic neuroprotection in female rats. Neurosci Lett. 2001; 297:159–162. PMID: 11137752.
Article52. Schierbeck LL, Rejnmark L, Tofteng CL, Stilgren L, Eiken P, Mosekilde L, et al. Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women: randomised trial. BMJ. 2012; 345:e6409. PMID: 23048011.
Article53. Shahar E, Folsom AR, Salomaa VV, Stinson VL, McGovern PG, Shimakawa T, et al. Relation of hormone-replacement therapy to measures of plasma fibrinolytic activity. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation. 1996; 93:1970–1975. PMID: 8640970.54. Gebara OC, Mittleman MA, Sutherland P, Lipinska I, Matheney T, Xu P, et al. Association between increased estrogen status and increased fibrinolytic potential in the Framingham Offspring Study. Circulation. 1995; 91:1952–1958. PMID: 7895352.
Article55. Klungel OH, Martens EP, Psaty BM, Grobbee DE, Sullivan SD, Stricker BH, et al. Methods to assess intended effects of drug treatment in observational studies are reviewed. J Clin Epidemiol. 2004; 57:1223–1231. PMID: 15617947.
Article56. Bosco JL, Silliman RA, Thwin SS, Geiger AM, Buist DS, Prout MN, et al. A most stubborn bias: no adjustment method fully resolves confounding by indication in observational studies. J Clin Epidemiol. 2010; 63:64–74. PMID: 19457638.
Article57. Liang W, Zhao Y, Lee AH. An investigation of the significance of residual confounding effect. Biomed Res Int. 2014; 2014:658056. PMID: 24696862.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of Mental Practice on Motor Function in Patients With Stroke: A Systematic Review and Meta-analysis
- An Introduction of the Systematic Review and Meta-Analysis
- A Systematic Review and Meta-Analysis of Music Therapy on Depression for Stroke Patients
- Systematic Review and Meta-analysis in Digestive Cancer Research
- Interventional Recanalization Treatment of Acute Ischemic Stroke