J Korean Foot Ankle Soc.
2018 Mar;22(1):44-47. 10.14193/jkfas.2018.22.1.44.
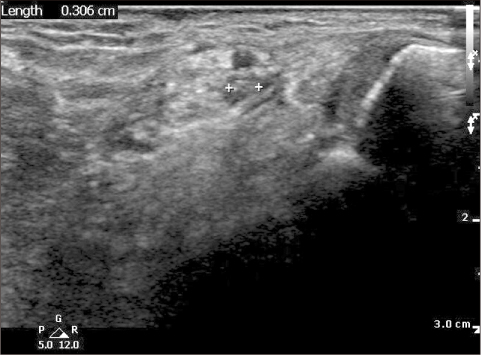
Tarsal Tunnel Syndrome Resulting from a Joint Originated the Intraneural Ganglion of the Medial Plantar Nerve: A Case Report: Surgical Treatment for Prevention of Recurrence
- Affiliations
-
- 1Department of Orthopedic Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- 2Department of Orthopedic Surgery, Yeungnam University Hospital, Daegu, Korea. chpark77@naver.com
- KMID: 2407375
- DOI: http://doi.org/10.14193/jkfas.2018.22.1.44
Abstract
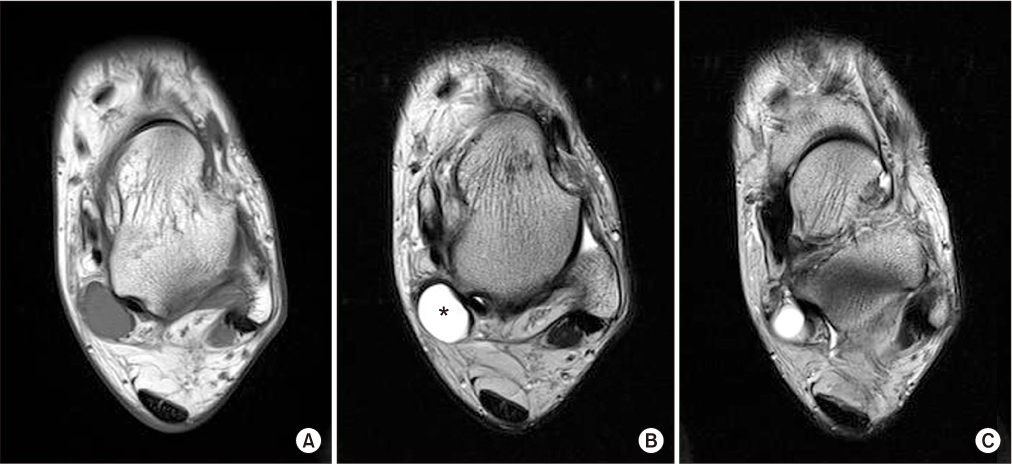
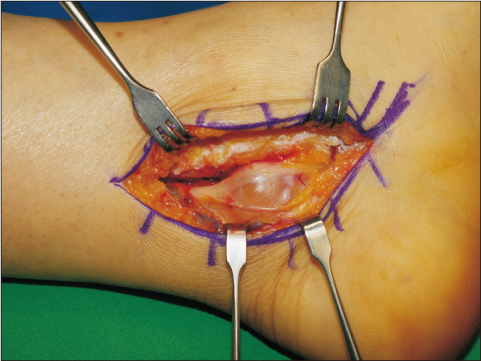
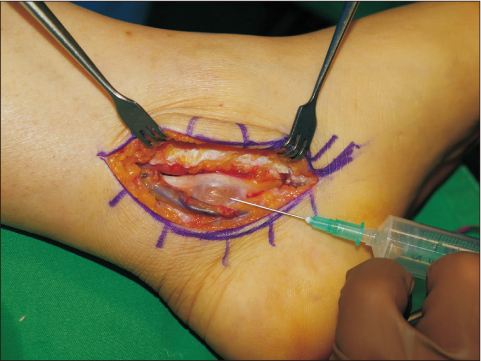
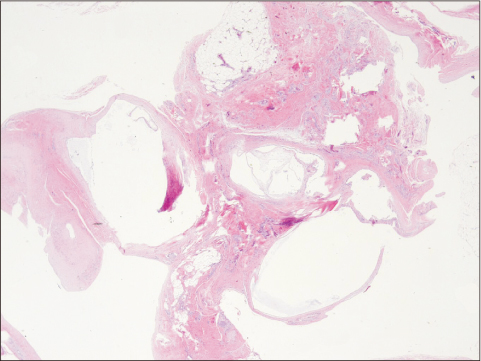
- There are a few reports on tarsal tunnel syndrome resulting from the intraneural ganglion. Although it can occur through a connection with the adjacent joint, there is no consensus on its pathogenesis and treatment method. This paper reports a case of tarsal tunnel syndrome resulting from the intraneural ganglion of the medial plantar nerve of the tibial nerve.
Figure
Reference
-
1. Ahmad M, Tsang K, Mackenney PJ, Adedapo AO. Tarsal tunnel syndrome: a literature review. Foot Ankle Surg. 2012; 18:149–152.
Article2. Lau JT, Daniels TR. Tarsal tunnel syndrome: a review of the literature. Foot Ankle Int. 1999; 20:201–209.
Article3. Sung KS, Park SJ. Short-term operative outcome of tarsal tunnel syndrome due to benign space-occupying lesions. Foot Ankle Int. 2009; 30:741–745.
Article4. Spinner RJ, Desy NM, Rock MG, Amrami KK. Peroneal intraneural ganglia. Part I. Techniques for successful diagnosis and treatment. Neurosurg Focus. 2007; 22:E16.5. Spinner RJ, Wang H. The first described joint-associated intraneural ganglion cyst. Neurosurgery. 2011; 69:1291–1298.
Article6. Fujita I, Matsumoto K, Minami T, Kizaki T, Akisue T, Yamamoto T. Tarsal tunnel syndrome caused by epineural ganglion of the posterior tibial nerve: report of 2 cases and review of the literature. J Foot Ankle Surg. 2004; 43:185–190.
Article7. Spinner RJ, Dellon AL, Rosson GD, Anderson SR, Amrami KK. Tibial intraneural ganglia in the tarsal tunnel: is there a joint connection? J Foot Ankle Surg. 2007; 46:27–31.
Article8. Friedlander HL. Intraneural ganglion of the tibial nerve. A case report. J Bone Joint Surg Am. 1967; 49:519–522.9. Spinner RJ, Atkinson JL, Harper CM Jr, Wenger DE. Recurrent intraneural ganglion cyst of the tibial nerve. Case report. J Neurosurg. 2000; 92:334–337.10. Chick G, Alnot JY, Silbermann-Hoffman O. Benign solitary tumors of the peripheral nerves. Rev Chir Orthop Reparatrice Appar Mot. 2000; 86:825–834.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ganglion of Flexor Digitorum Longus Tendon Sheath and Multifocal Myxoid Degeneration of Medial Plantar Nerve Producing Tarsal Tunnel Syndrome: A Case Report
- Surgical Decompression of Tarsal Tunnel Syndrome Associated with Ganglion Cyst: A Case Report
- Cubital tunnel syndrome caused by an intraneural ganglion cyst treated with epineurectomy: a report of three cases
- Tarsal Tunnel Syndrome caused by Neurilemoma of the Posterior Tibial Nerve: A case Report
- Intraneural Ganglion of Ulnar Nerve in Proximal Forearm: Case Report