J Neurocrit Care.
2017 Dec;10(2):136-139. 10.18700/jnc.170023.
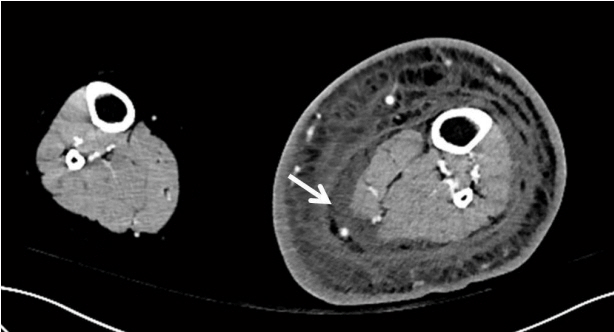
Reversible Splenial Lesion associated with Cellulitis in a Patient with Lymphedema
- Affiliations
-
- 1Department of Neurology, Kosin University College of Medicine, Busan, Korea. ybg99@naver.com
- KMID: 2405772
- DOI: http://doi.org/10.18700/jnc.170023
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Tada H, Takanashi J, Barkovich AJ, Oba H, Maeda M, Tsukahara H, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology. 2004; 63:1854–8.
Article2. Avcu G, Kilinc MA, Eraslan C, Karapinar B, Vardar F. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) associated with Streptococcus pneumoniae Bacteraemia. J Infect Public Health. 2017; 10:479–82.
Article3. Yuan J, Yang S, Wang S, Qin W, Yang L, Hu W. Mild encephalitis/encephalopathy with reversible splenial lesion (MERS) in adults-a case report and literature review. BMC Neurol. 2017; 17:103.
Article4. Zhang S, Ma Y, Feng J. Clinicoradiological spectrum of reversible splenial lesion syndrome (RESLES) in adults: a retrospective study of a rare entity. Medicine (Baltimore). 2015; 94:e512.5. Kosami K, Kenzaka T, Sagara Y, Minami K, Matsumura M. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion caused by methicillin-sensitive Staphylococcus aureus bacteremia with toxic shock syndrome: a case report. BMC Infect Dis. 2016; 16:160.
Article6. Takanashi J. Two newly proposed infectious encephalitis/encephalopathy syndromes. Brain Dev. 2009; 31:521–8.
Article7. Park SI, Yang EJ, Kim DK, Jeong HJ, Kim GC, Sim YJ. Prevalence and epidemiological factors involved in cellulitis in korean patients with lymphedema. Ann Rehabil Med. 2016; 40:326–33.
Article8. Gürgöze MK, Akarsu S, Yilmaz E, Gödekmerdan A, Akça Z, Ciftçi I, et al. Proinflammatory cytokines and procalcitonin in children with acute pyelonephritis. Pediatr Nephrol. 2005; 20:1445–8.
Article9. Teerachaisakul M, Ekataksin W, Durongwatana S, Taneepanichskul S. Diet, C-reactive protein levels and cellulitis in patients with lymphedema: a cross-sectional study. J Med Med Sci. 2011; 2:1297–301.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Lithium-Induced Downbeat Nystagmus with Reversible Splenial Lesion
- The Changes in Axial and Radial Diffusivity in a Patient with Clinically Mild Encephalitis/Encephalopathy with a Reversible Splenial Lesion
- A Case of Transient Isolated Splenial Lesion of the Corpus Callosum After New Onset Seizure
- Long-Term Dysfunction of Frontal Lobe in a Patient with Isolated Reversible Splenial Lesion after Status Epilepticus
- Reversible Cerebral Vasoconstriction Syndrome Combined with Posterior Encephalopathy Syndrome, and Transient Splenial Lesion after Delivery