Clin Orthop Surg.
2018 Mar;10(1):47-54. 10.4055/cios.2018.10.1.47.
What Is the Most Effective Eccentric Stretching Position in Lateral Elbow Tendinopathy?
- Affiliations
-
- 1Department of Orthopedic Surgery, Dankook University College of Medicine, Cheonan, Korea. osarthro@gmail.com
- KMID: 2405482
- DOI: http://doi.org/10.4055/cios.2018.10.1.47
Abstract
- BACKGROUND
A variety of treatment options suggest that the optimal treatment strategy for lateral elbow tendinopathy (LET) is not known, and further research is needed to discover the most effective treatment for LET. The purpose of the present study was to verify the most effective position of eccentric stretching for the extensor carpi radialis brevis (ECRB) in vivo using ultrasonic shear wave elastography.
METHODS
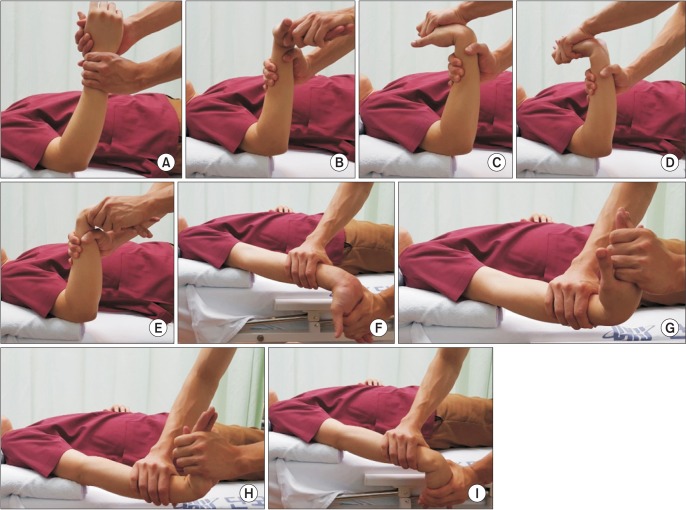
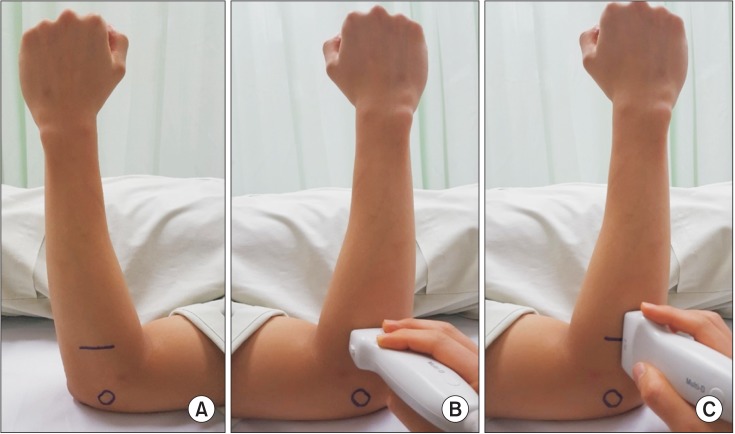
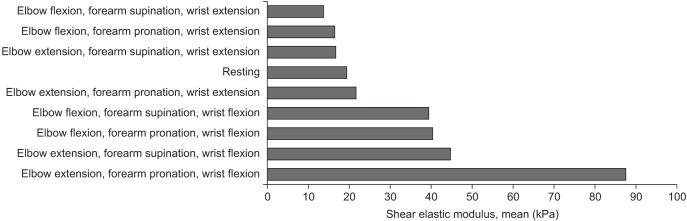
A total of 20 healthy males participated in this study. Resting position was defined as 90° elbow flexion and neutral position of the forearm and wrist. Elongation of the ECRB was measured for four stretching maneuvers (forearm supination/pronation and wrist extension/flexion) at two elbow angles (90° flexion and full extension). The shear elastic modulus, used as the index of muscle elongation, was computed using ultrasonic shear wave elastography for the eight aforementioned stretching maneuverangle combinations.
RESULTS
The shear elastic modulus was the highest in elbow extension, forearm pronation, and wrist flexion. The shear elastic moduli of wrist flexion with any forearm and elbow position were significantly higher than the resting position. There was no significant difference associated with elbow and forearm positions except for elbow extension, forearm pronation, and wrist flexion positions.
CONCLUSIONS
This study determined that elbow extension, forearm pronation, and wrist flexion was the most effective eccentric stretching for the ECRB in vivo.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comments on the Article “What Is the Most Effective Eccentric Stretching Position in Lateral Elbow Tendinopathy?”: To the Editor
Dimitrios Stasinopoulos
Clin Orthop Surg. 2018;10(2):269-269. doi: 10.4055/cios.2018.10.2.269.
Reference
-
1. Stasinopoulos D, Stasinopoulos I. Comparison of effects of eccentric training, eccentric-concentric training, and eccentric-concentric training combined with isometric contraction in the treatment of lateral elbow tendinopathy. J Hand Ther. 2017; 30(1):13–19. PMID: 27823901.
Article2. Stasinopoulos D, Johnson MI. 'Lateral elbow tendinopathy' is the most appropriate diagnostic term for the condition commonly referred-to as lateral epicondylitis. Med Hypotheses. 2006; 67(6):1400–1402. PMID: 16843614.
Article3. Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother. 2015; 61(4):174–181. PMID: 26361816.
Article4. Vicenzino B, Collins D, Wright A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain. 1996; 68(1):69–74. PMID: 9252000.
Article5. Trudel D, Duley J, Zastrow I, Kerr EW, Davidson R, Mac-Dermid JC. Rehabilitation for patients with lateral epicondylitis: a systematic review. J Hand Ther. 2004; 17(2):243–266. PMID: 15162109.
Article6. Smidt N, Assendelft WJ, Arola H, et al. Effectiveness of physiotherapy for lateral epicondylitis: a systematic review. Ann Med. 2003; 35(1):51–62. PMID: 12693613.
Article7. Malliaras P, Barton CJ, Reeves ND, Langberg H. Achilles and patellar tendinopathy loading programmes: a systematic review comparing clinical outcomes and identifying potential mechanisms for effectiveness. Sports Med. 2013; 43(4):267–286. PMID: 23494258.8. Stasinopoulos D, Johnson MI. Cyriax physiotherapy for tennis elbow/lateral epicondylitis. Br J Sports Med. 2004; 38(6):675–677. PMID: 15562158.
Article9. Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control. 2004; 51(4):396–409. PMID: 15139541.
Article10. Shiina T, Nightingale KR, Palmeri ML, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography. Part 1: basic principles and terminology. Ultrasound Med Biol. 2015; 41(5):1126–1147. PMID: 25805059.
Article11. Song S, Huang Z, Nguyen TM, et al. Shear modulus imaging by direct visualization of propagating shear waves with phase-sensitive optical coherence tomography. J Biomed Opt. 2013; 18(12):121509. PMID: 24213539.
Article12. Koo TK, Guo JY, Cohen JH, Parker KJ. Relationship between shear elastic modulus and passive muscle force: an ex-vivo study. J Biomech. 2013; 46(12):2053–2059. PMID: 23769175.
Article13. Umegaki H, Ikezoe T, Nakamura M, et al. The effect of hip rotation on shear elastic modulus of the medial and lateral hamstrings during stretching. Man Ther. 2015; 20(1):134–137. PMID: 25194631.
Article14. Umegaki H, Ikezoe T, Nakamura M, et al. Acute effects of static stretching on the hamstrings using shear elastic modulus determined by ultrasound shear wave elastography: differences in flexibility between hamstring muscle components. Man Ther. 2015; 20(4):610–613. PMID: 25795108.
Article15. Kudo M, Shiina T, Moriyasu F, et al. JSUM ultrasound elastography practice guidelines: liver. J Med Ultrason (2001). 2013; 40(4):325–357. PMID: 27277450.
Article16. Alfredson H, Pietila T, Jonsson P, Lorentzon R. Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis. Am J Sports Med. 1998; 26(3):360–366. PMID: 9617396.17. Jensen K, Di Fabio RP. Evaluation of eccentric exercise in treatment of patellar tendinitis. Phys Ther. 1989; 69(3):211–216. PMID: 2919192.
Article18. el Hawary R, Stanish WD, Curwin SL. Rehabilitation of tendon injuries in sport. Sports Med. 1997; 24(5):347–358. PMID: 9368280.
Article19. Khan KM, Cook JL, Kannus P, Maffulli N, Bonar SF. Time to abandon the “tendinitis” myth. BMJ. 2002; 324(7338):626–627. PMID: 11895810.
Article20. Ackermann PW, Renstrom P. Tendinopathy in sport. Sports Health. 2012; 4(3):193–201. PMID: 23016086.
Article21. Murtaugh B, Ihm JM. Eccentric training for the treatment of tendinopathies. Curr Sports Med Rep. 2013; 12(3):175–182. PMID: 23669088.
Article22. Soderberg J, Grooten WJ, Ang BO. Effects of eccentric training on hand strength in subjects with lateral epicondylalgia: a randomized-controlled trial. Scand J Med Sci Sports. 2012; 22(6):797–803. PMID: 21496112.23. Tyler TF, Thomas GC, Nicholas SJ, McHugh MP. Addition of isolated wrist extensor eccentric exercise to standard treatment for chronic lateral epicondylosis: a prospective randomized trial. J Shoulder Elbow Surg. 2010; 19(6):917–922. PMID: 20579907.24. Nordez A, Gennisson JL, Casari P, Catheline S, Cornu C. Characterization of muscle belly elastic properties during passive stretching using transient elastography. J Biomech. 2008; 41(10):2305–2311. PMID: 18539284.
Article25. Umehara J, Nakamura M, Fujita K, et al. Shoulder horizontal abduction stretching effectively increases shear elastic modulus of pectoralis minor muscle. J Shoulder Elbow Surg. 2017; 26(7):1159–1165. PMID: 28169137.
Article26. Sarvazyan AP, Rudenko OV, Swanson SD, Fowlkes JB, Emelianov SY. Shear wave elasticity imaging: a new ultrasonic technology of medical diagnostics. Ultrasound Med Biol. 1998; 24(9):1419–1435. PMID: 10385964.
Article27. Morrow DA, Haut Donahue TL, Odegard GM, Kaufman KR. Transversely isotropic tensile material properties of skeletal muscle tissue. J Mech Behav Biomed Mater. 2010; 3(1):124–129. PMID: 19878911.
Article28. Ewertsen C, Carlsen JF, Christiansen IR, Jensen JA, Nielsen MB. Evaluation of healthy muscle tissue by strain and shear wave elastography: dependency on depth and ROI position in relation to underlying bone. Ultrasonics. 2016; 71:127–133. PMID: 27336792.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comments on the Article “What Is the Most Effective Eccentric Stretching Position in Lateral Elbow Tendinopathy?â€: In Reply
- Comments on the Article “What Is the Most Effective Eccentric Stretching Position in Lateral Elbow Tendinopathy?â€: To the Editor
- Comparison of Wrist Extension Stretching Exercise and a Wait-and-see Policy for Treatment of Lateral Epicondylitis
- Biologic Treatment for the Elbow Tendinopathy
- Ultrasonographic Findings of Epicondylitis