J Korean Ophthalmol Soc.
2018 Feb;59(2):110-116. 10.3341/jkos.2018.59.2.110.
The Cosmetic Effects of Full Thickness Eyelid Resection and Direct Closure for Eyelid Malignant Tumors
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. oculoplasty@gmail.com
- 2T2B Infrastructure Center for Ocular Disease, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Ophthalmology, Dong-Eui Medical Center, Busan, Korea.
- 4Ulsan Shinsaegae Eye Clinic, Ulsan, Korea.
- KMID: 2403802
- DOI: http://doi.org/10.3341/jkos.2018.59.2.110
Abstract
- PURPOSE
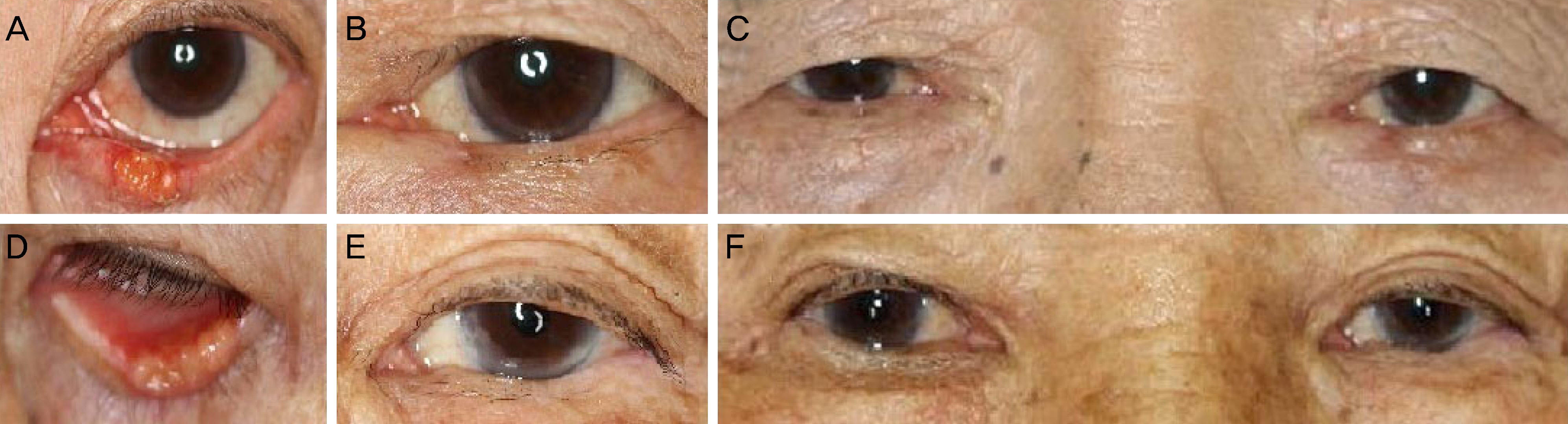
To evaluate the degree of eyelid deformation and satisfaction after direct closure in patients with 40-70% eyelid defects after resection of an eyelid malignant tumor.
METHODS
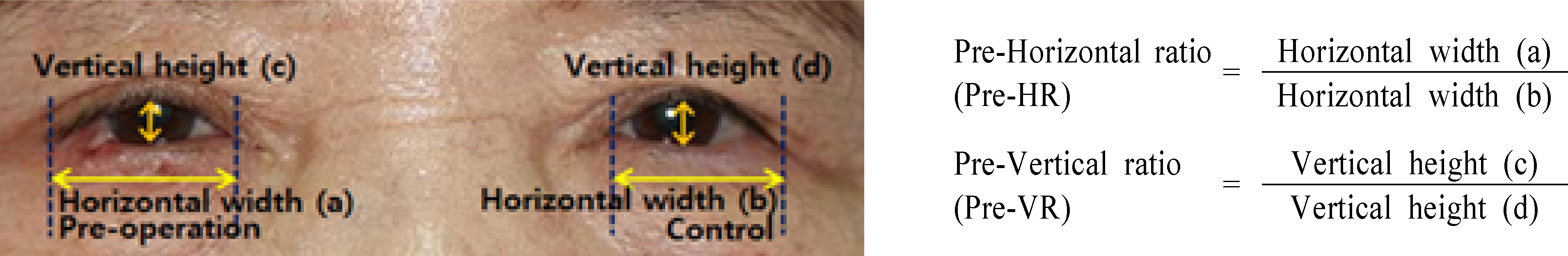
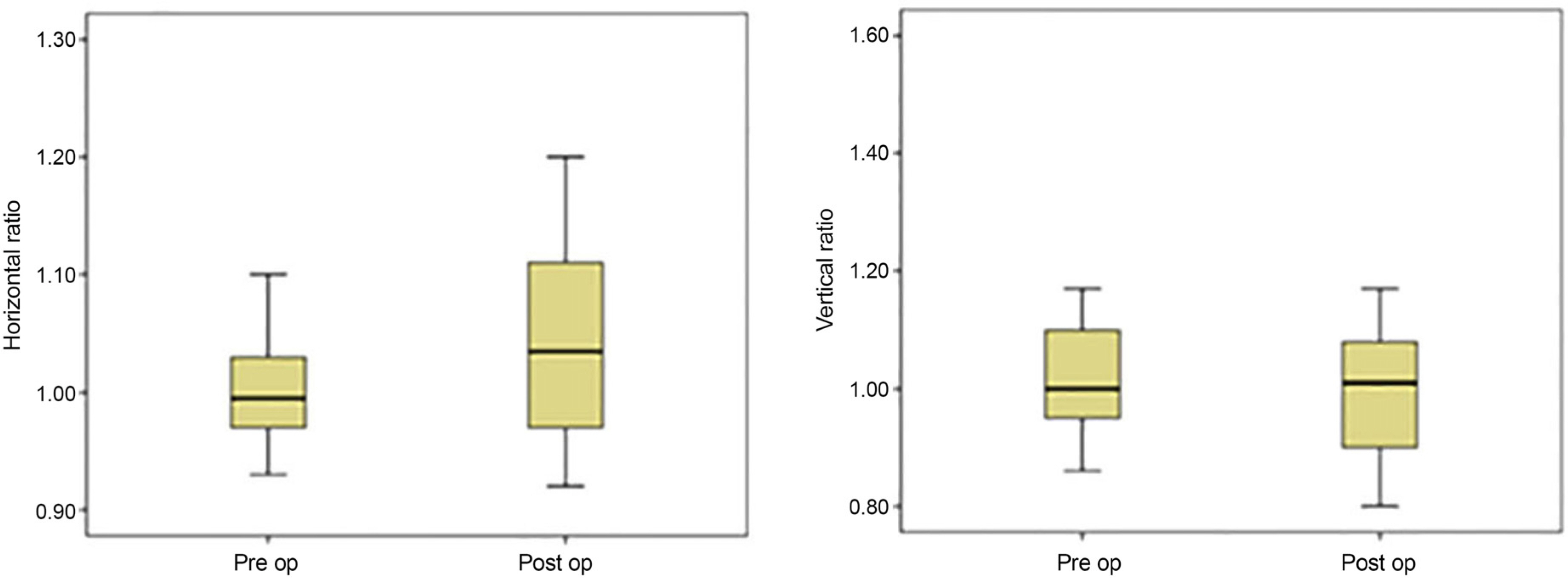
We retrospectively reviewed the clinical records of patients diagnosed with eyelid malignant tumors between January 2009 and June 2016, who were treated with resection of 40-70% of the eyelid, followed by reconstructed direct closure only or by direct closure with lateral canthotomy and cantholysis. Age, sex, diagnosis, tumor location, satisfaction, and complications were analyzed, and the ratio of horizontal width ratio and vertical height ratio were compared before and after surgery.
RESULTS
The results of satisfaction were: 12 patients (60%), very good; five patients (25%), good; and three patients (15%), fair. The average preoperative horizontal width ratio and vertical height ratio were 1.03 ± 0.01 and 1.08 ± 0.30, respectively. The average postoperative horizontal width ratio and vertical height ratio were 1.04 ± 0.08 and 1.01 ± 0.17, respectively There was no significant difference in horizontal width ratio or vertical height ratio before and after surgery (p = 0.314 and p = 0.087, respectively).
CONCLUSIONS
Eyelid reconstruction with a direct closure can be performed without a flap or graft for 40-70% of eyelid defects when resecting the eyelid of a malignant eyelid tumor.
Figure
Reference
-
References
1. Werner MS, Olson JJ, Putterman AM. Composite grafting for abdominal reconstruction. Am J Ophthalmol. 1993; 116:11–6.2. Putterman AM. Combined viable composite graft and temporal semicircular skin flap procedure. Am J Ophthalmol. 1984; 98:349–54.
Article3. Hughes WL. Reconstruction of the lids. Am J Ophthalmol. 1945; 28:1203–11.
Article4. Renner G, Kang T. Periorbital reconstruction: brows and eyelids. Facial Plast Surg Clin North Am. 2005; 13:253–65. vi.
Article5. Rafii AA, Enepekides DJ. Upper and lower eyelid reconstruction: the year in review. Curr Opin Otolaryngol Head Neck Surg. 2006; 14:227–33.
Article6. Moss AL, Cooper MA, Lendrum J, Hiles RW. The sanctity of the upper lid in lower eyelid reconstruction questioned. A modification of a lid sharing procedure with a long-term follow-up. Br J Plast Surg. 1987; 40:246–57.
Article7. Putterman AM. Reconstruction of the eyelids following resection for carcinoma. Clin Plast Surg. 1985; 12:393–410.
Article8. Mehta MP, Lewis CD, Perry JD. Internal cantholysis for full abdominal eyelid defects. Saudi J Ophthalmol. 2011; 25:31–6.9. Tenzel RR, Stewart WB. Eyelid reconstruction by the semicircle flap technique. Ophthalmology. 1978; 85:1164–9.
Article10. Hornblass A, Vincent MP. Oculoplastic, orbital and reconstructive surgery. Plast Reconstr Surg. 1990; 86:1033.
Article11. Tse DT, McCafferty LR. Controlled tissue expansion in periocular reconstructive surgery. Ophthalmology. 1993; 100:260–8.
Article12. Petro JA, Niazi ZB. Immediate skin expansion: an old concept by a novel and inexpensive technique. Ann Plast Surg. 1996; 36:479–84.13. Marcus J, Horan DB, Robinson JK. Tissue expansion: past, abdominal, and future. J Am Acad Dermatol. 1990; 23(5 Pt 1):813–25.14. Foster JA, Scheiner AJ, Wulc AE, et al. Intraoperative tissue abdominal in eyelid reconstruction. Ophthalmology. 1998; 105:170–5.15. Papadopoulos O, Konofaos P, Chrisostomidis C, et al. Orbitopalpebral repair after 835 excisions of malignant tumours. Scand J Plast Reconstr Surg Hand Surg. 2005; 39:353–9.
Article16. Miller EA, Boynton JR. Complications of eyelid reconstruction abdominal a semicircular flap. Ophthalmic Surg. 1987; 18:807–10.17. Thaller VT, Then KY, Luhishi E. Spontaneous eyelid expansion abdominal full thickness eyelid resection and direct closure. Br J Ophthalmol. 2001; 85:1450–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Surgical Effect of Full-Thickness Eyelid Resection in Traumatic Blepharoptosis
- Upper Eyelid Reconstruction Using the Medpor(R) Sheet and Median Forehead Flap
- Early cicatricial lagophthalmos release with pentagonal wedge resection of the scar, fat redistribution, and full-thickness skin grafting
- A Case of Full-thickness Lower Eyelid Reconstruction by a Tenzel Flap
- Anatomy of upper Eyelid in Korean