J Korean Soc Spine Surg.
2017 Mar;24(1):49-54. 10.4184/jkss.2017.24.1.49.
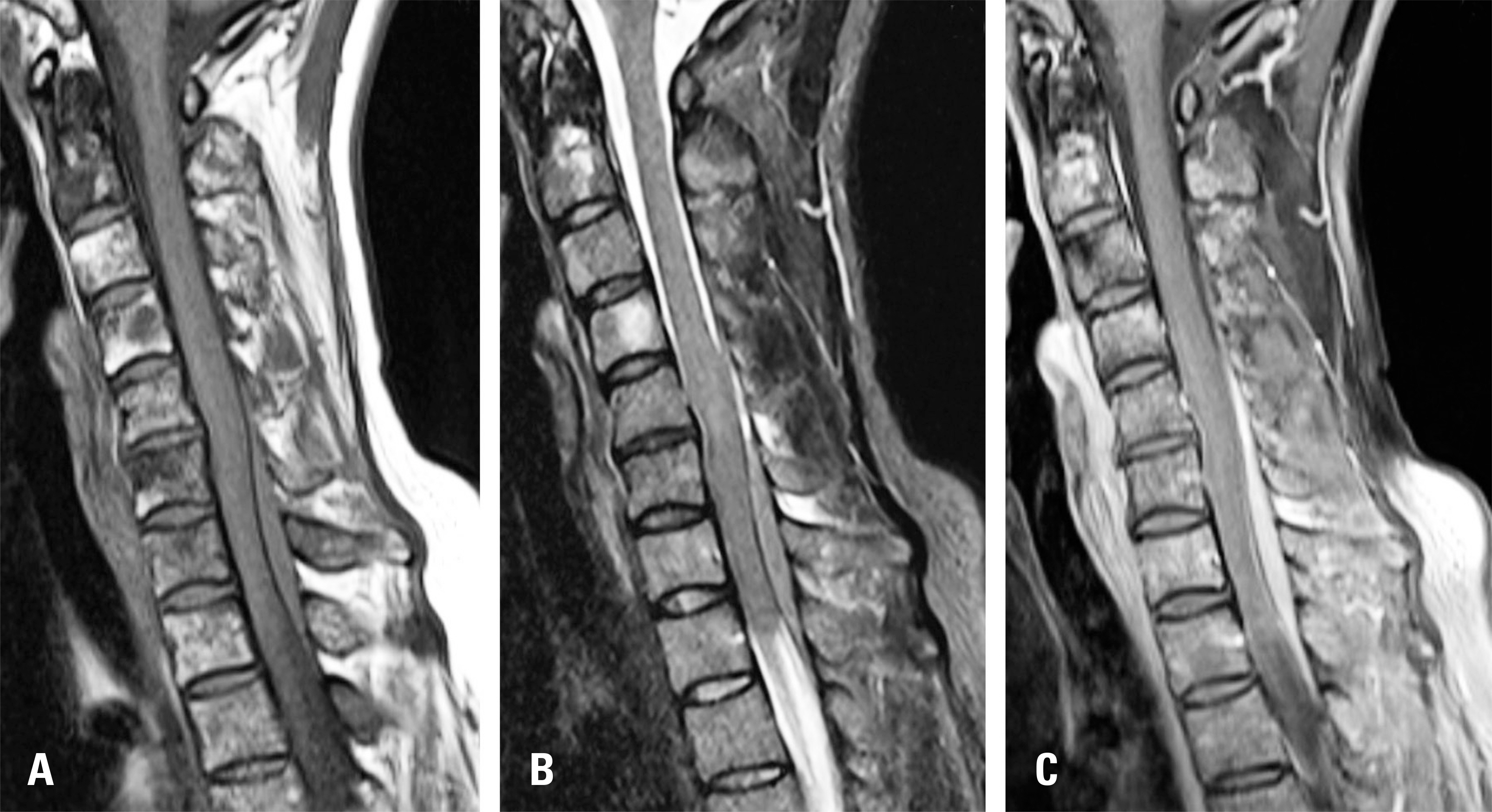
Epidural Lymphoma Mimicking Hematoma: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Gyeongsang National University School of Medicine and Gyeongsang National University Hospital, Jinju, Republic of Korea. dhkim8311@gnu.ac.kr
- 2Department of Pathology, Gyeongsang National University School of Medicine and Gyeongsang National University Hospital, Jinju, Republic of Korea.
- KMID: 2402843
- DOI: http://doi.org/10.4184/jkss.2017.24.1.49
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
To present a rare case of a spinal epidural lymphoma mimicking a hematoma. SUMMARY OF LITERATURE REVIEW: The incidence of extranodal invasion of lymphoma is very low, and spinal compression as a clinical symptom rarely occurs in extranodal lymphoma.
MATERIALS AND METHODS
A 37-year-old woman who complained of neck pain that had lasted for the past 3 months with no underlying disease visited the hospital and was treated conservatively with medication and physical therapy. Even though the patient was given an epidural injection 1 month prior to visiting our hospital, the pain lingered and the cervical myelopathy became aggravated, so the patient was initially diagnosed with epidural hematoma. This predisposed the patient to treatment strategies such as laminectomy and fusion, but the patient was ultimately diagnosed with non-Hodgkin lymphoma.
RESULTS
The patient underwent a laminectomy with excision of the lesion and fusion. The patient was diagnosed with non-Hodgkin lymphoma as a result of this, and the patient's radicular pain and numbness improved immediately following surgery, except for mild weakness in both hands.
CONCLUSIONS
Although spinal epidural lymphoma is similar to hematoma, and is a very rare disease, surgeons should take it into consideration in the differential diagnosis of patients with a spinal epidural lesion.
Keyword
MeSH Terms
Figure
Reference
-
1. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972; 29:252–60.
Article2. Aabo K, Walbom-Jorgensen S. Central nervous system complications by malignant lymphomas: radiation sched-ule and treatment results. Int J Radiat Oncol Biol Phys. 1986; 12:197–202.
Article3. Lim CC, Chong BK. Spinal epidural non-Hodgkin's lymphoma: case reports of three patients presenting with spinal cord compression. Singapore Med J. 1996; 37:497–500.4. Cho JH, Cho DC, Sung JK, et al. Primary malignant lym-phoma in a spinal cord presenting as an epidural mass with myelopathy: a case report. Korean J Spine. 2012; 9:265–8.
Article5. Mally R, Sharma M, Khan S, et al. Primary Lumbosacral Spinal Epidural Non-Hodgkin's Lymphoma: A Case Report and Review of Literature. Asian Spine J. 2011; 5:192–5.
Article6. Kapoor R, Kumar V, Sharma SC. Primary extradural non-Hodgkin's lymphoma. JK Science. 2006; 8:45–8.7. Braunistein EM, White SJ. Non-hodgkin's lymphoma of bone. Radiology. 1980. 59–63.8. Mascalchi M, Torselli P, Falaschi F, et al. MRI of spinal epidural lymphoma. Neuroradiology. 1995; 37:303–7.
Article9. Kim JM, Ko YH, Lee SS, et al. WHO Classification of Malignant Lymphomas in Korea: Report of the Third Nation-wide Study. Korean J Pathol. 2011; 45:254–60.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Epidural Lymphoma Mimicking Hematoma: A Case Report
- Thoracolumbar Epidural Hematoma Complicated by Cauda Equina Syndrome : Complication of Systemic Heparinization Following Epidural Anesthesia: A case report
- Epidural hematoma treated by aspiration after transforaminal epidural steroid injection - A case report -
- Spontaneous Cervical Epidural Hematoma Mimicking Acute Ischemic Stroke
- Spontaneous intracranial epidural hematoma following aortic valve replacement: A case report