Pediatr Gastroenterol Hepatol Nutr.
2017 Dec;20(4):252-258. 10.5223/pghn.2017.20.4.252.
Blunt Trauma Pancreas in Children: Is Non-Operative Management Appropriate for All Grades?
- Affiliations
-
- 1Department of General Surgery, Kalpna Chawla Govt. Medical College, Karnal, India.
- 2Department of Pediatric Surgery, Post Graduate Institute of Medical Education and Research, Chandigarh, India. jkmahajan@gmail.com
- KMID: 2398907
- DOI: http://doi.org/10.5223/pghn.2017.20.4.252
Abstract
- PURPOSE
Blunt trauma of pancreas in children is uncommon and its management varies from observational to early operative intervention. We analysed the feasibility and outcome of non-operative management in all grades of paediatric pancreatic injuries.
METHODS
A total of 15 patients of pancreatic trauma seen in a Paediatric Surgery Unit were retrospectively analyzed.
RESULTS
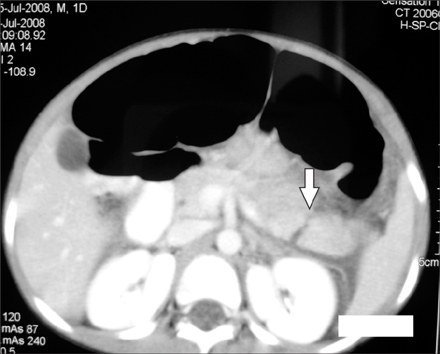
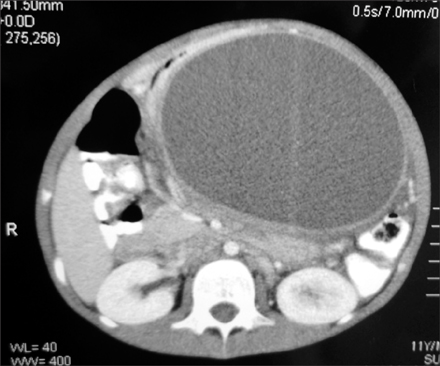
Age of the patients ranged from 3-11 years (mean, 7.7 years). The mode of injury was local trauma in 9 children. Only 3 patients had associated injuries and all were haemodynamically stable. Serum amylase levels were raised in 12 patients at admission which ranged from 400-1,000 IU. Computed tomography scan made a correct diagnosis in 14 patients. Grades of the injury varied from grade I-V (1, 3, 6, 4, 1 patients respectively). Fourteen patients were managed conservatively. One patient underwent laparotomy for suspected superior mesenteric hematoma. The average duration of enteral feeds was 3.7 days and of hospital stay was 9.4 days. Six patients formed pancreatic pseudocysts; two were managed conservatively while the other four underwent cystogastrostomy. The patients were followed up for a period of 1-12 years. All remained asymptomatic and none had exocrine or endocrine deficiencies.
CONCLUSION
Non-operative treatment for isolated blunt trauma of pancreas in children may be safely followed for all the grades of injury; if associated injuries requiring surgical intervention are ruled out with a good quality imaging and the patients are hemodynamically stable. It did not increase the hospital stay and morbidity and avoided operative intervention on acutely injured pancreas.
MeSH Terms
Figure
Reference
-
1. Jacombs AS, Wines M, Holland A, Ross FI, Shun A, Cass DT. Pancreatic trauma in children. J Pediatr Surg. 2004; 39:96–99.
Article2. Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J, et al. Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg. 2007; 42:340–344.
Article3. Paul MD, Mooney DP. The management of pancreatic injuries in children: operate or observe. J Pediatr Surg. 2011; 46:1140–1143.
Article4. Wood JH, Partrick DA, Bruny JL, Sauaia A, Moulton SL. Operative vs nonoperative management of blunt pancreatic trauma in children. J Pediatr Surg. 2010; 45:401–406.
Article5. Meier DE, Coln CD, Hicks BA, Guzzetta PC. Early operation in children with pancreas transection. J Pediatr Surg. 2001; 36:341–344.
Article6. Snajdauf J, Rygl M, Kalousová J, Kucera A, Petrů O, Pýcha K, et al. Surgical management of major pancreatic injury in children. Eur J Pediatr Surg. 2007; 17:317–321.
Article7. Cigdem MK, Senturk S, Onen A, Siga M, Akay H, Otcu S. Nonoperative management of pancreatic injuries in pediatric patients. Surg Today. 2011; 41:655–659.
Article8. de Blaauw I, Winkelhorst JT, Rieu PN, van der Staak FH, Wijnen MH, Severijnen RS, et al. Pancreatic injury in children: good outcome of nonoperative treatment. J Pediatr Surg. 2008; 43:1640–1643.
Article9. Herman R, Guire KE, Burd RS, Mooney DP, Ehlrich PF. Utility of amylase and lipase as predictors of grade of injury or outcomes in pediatric patients with pancreatic trauma. J Pediatr Surg. 2011; 46:923–926.
Article10. Adamson WT, Hebra A, Thomas PB, Wagstaff P, Tagge EP, Othersen HB. Serum amylase and lipase alone are not cost-effective screening methods for pediatric pancreatic trauma. J Pediatr Surg. 2003; 38:354–357. discussion 354-7.
Article11. Shilyansky J, Sena LM, Kreller M, Chait P, Babyn PS, Filler RM, et al. Nonoperative management of pancreatic injuries in children. J Pediatr Surg. 1998; 33:343–349.
Article12. Rekhi S, Anderson SW, Rhea JT, Soto JA. Imaging of blunt pancreatic trauma. Emerg Radiol. 2010; 17:13–19.
Article13. Canty TG Sr, Weinman D. Management of major pancreatic duct injuries in children. J Trauma. 2001; 50:1001–1007.
Article14. Gupta A, Stuhlfaut JW, Fleming KW, Lucey BC, Soto JA. Blunt trauma of the pancreas and biliary tract: a multimodality imaging approach to diagnosis. Radiographics. 2004; 24:1381–1395.
Article15. Houben CH, Ade-Ajayi N, Patel S, Kane P, Karani J, Devlin J, et al. Traumatic pancreatic duct injury in children: minimally invasive approach to management. J Pediatr Surg. 2007; 42:629–635.
Article16. Cuenca AG, Islam S. Pediatric pancreatic trauma: trending toward nonoperative management? Am Surg. 2012; 78:1204–1210.
Article17. Beres AL, Wales PW, Christison-Lagay ER, McClure ME, Fallat ME, Brindle ME. Non-operative management of high-grade pancreatic trauma: is it worth the wait. J Pediatr Surg. 2013; 48:1060–1064.
Article18. Jobst MA, Canty TG Sr, Lynch FP. Management of pancreatic injury in pediatric blunt abdominal trauma. J Pediatr Surg. 1999; 34:818–823. discussion 823-4.
Article19. Lin BC, Chen RJ, Fang JF, Hsu YP, Kao YC, Kao JL. Management of blunt major pancreatic injury. J Trauma. 2004; 56:774–778.
Article20. Fisher M, Brasel K. Evolving management of pancreatic injury. Curr Opin Crit Care. 2011; 17:613–617.
Article21. Wales PW, Shuckett B, Kim PC. Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg. 2001; 36:823–827.
Article22. Hamidian Jahromi A, D'Agostino HR, Zibari GB, Chu QD, Clark C, Shokouh-Amiri H. Surgical versus nonsurgical management of traumatic major pancreatic duct transection: institutional experience and review of the literature. Pancreas. 2013; 42:76–87.23. Keller MS, Stafford PW, Vane DW. Conservative management of pancreatic trauma in children. J Trauma. 1997; 42:1097–1100.
Article24. Teh SH, Pham TH, Lee A, Stavlo PL, Hanna AM, Moir C. Pancreatic pseudocyst in children: the impact of management strategies on outcome. J Pediatr Surg. 2006; 41:1889–1893.
Article25. Abbo O, Lemandat A, Reina N, Bouali O, Ballouhey Q, Carfagna L, et al. Conservative management of blunt pancreatic trauma in children: a single center experience. Eur J Pediatr Surg. 2013; 23:470–473.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blunt abdominal trauma resulting in pancreatic injury in a pediatric patient in Australia: a case report
- Nonoperative Management of Children with Blunt Abdominal Trauma
- Roentgenologic evaluation of blunt abdominal trauma
- Nonoperative Management of Blunt Abdominal Trauma with Hemoperitoneum
- Management of High-grade Blunt Renal Trauma