Korean J Gastroenterol.
2017 Dec;70(6):273-277. 10.4166/kjg.2017.70.6.273.
Belching
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. ykcho@catholic.ac.kr
- KMID: 2398876
- DOI: http://doi.org/10.4166/kjg.2017.70.6.273
Abstract
- Supragastric belching is the most important factor in the etiology of excessive belching complaints. Supragastric belching is a belching disorder with a behavioral origin. The standard diagnosis is made by monitoring the esophageal impedance. Supragastric belching has been shown to be associated with globus, as well as reflux symptoms in proton pump inhibitor non-responders in gastroesophageal reflux disease; however, the pathophysiology of supragastric belching in patients with gastroesophageal reflux disease or functional dyspepsia has not been clarified. Patient education with behavioral therapy is the treatment of choice in isolated supragastric belching. On the other hand, the best management of supragastric belching associated with globus, gastroesophageal reflux disease, and dyspepsia remains to be studied.
MeSH Terms
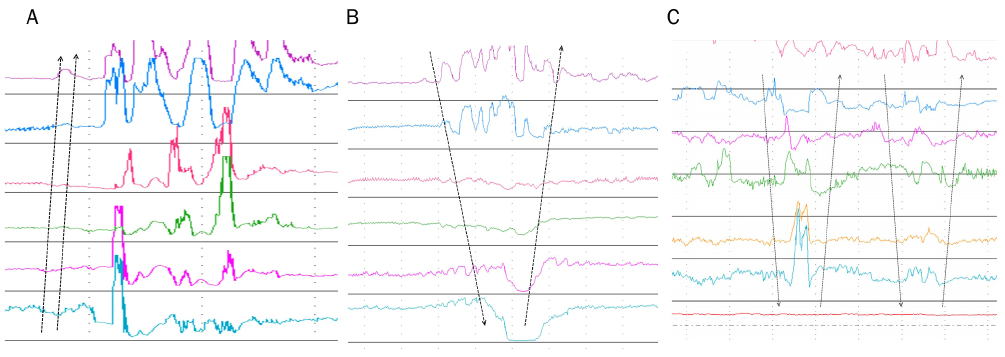
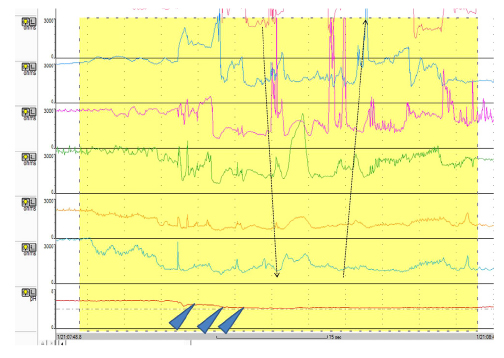
Figure
Cited by 1 articles
-
A Supragastric Belching Case Treated with Speech Therapy
Seoyeon Yoo, Ga Hee Kim, Ji Yong Ahn, Kee Wook Jung, Miseon Kwon
Korean J Gastroenterol. 2019;73(1):56-59. doi: 10.4166/kjg.2019.73.1.56.
Reference
-
1. Bredenoord AJ, Smout AJ. Impaired health-related quality of life in patients with excessive supragastric belching. Eur J Gastroenterol Hepatol. 2010; 22:1420–1423.2. Klauser AG, Schindlbeck NE, Müller-Lissner SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990; 335:205–208.3. Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Air swallowing, belching, and reflux in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2006; 101:1721–1726.4. Kessing BF, Bredenoord AJ, Velosa M, Smout AJ. Supragastric belches are the main determinants of troublesome belching symptoms in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2012; 35:1073–1079.5. Lin M, Triadafilopoulos G. Belching: dyspepsia or gastroesophageal reflux disease? Am J Gastroenterol. 2003; 98:2139–2145.6. Penagini R, Carmagnola S, Cantù P, Allocca M, Bianchi PA. Mechanoreceptors of the proximal stomach: role in triggering transient lower esophageal sphincter relaxation. Gastroenterology. 2004; 126:49–56.7. Mittal RK, Fisher MJ. Electrical and mechanical inhibition of the crural diaphragm during transient relaxation of the lower esophageal sphincter. Gastroenterology. 1990; 99:1265–1268.8. Lang IM, Medda BK, Shaker R. Digestive and respiratory tract motor responses associated with eructation. Am J Physiol Gastrointest Liver Physiol. 2013; 304:G1044–G1053.9. Babaei A, Bhargava V, Korsapati H, Zheng WH, Mittal RK. A unique longitudinal muscle contraction pattern associated with transient lower esophageal sphincter relaxation. Gastroenterology. 2008; 134:1322–1331.10. Shaker R, Ren J, Kern M, Dodds WJ, Hogan WJ, Li Q. Mechanisms of airway protection and upper esophageal sphincter opening during belching. Am J Physiol. 1992; 262(4 Pt 1):G621–G628.11. Karamanolis G, Triantafyllou K, Tsiamoulos Z, et al. Effect of sleep on excessive belching: a 24-hour impedance-pH study. J Clin Gastroenterol. 2010; 44:332–334.12. Chitkara DK, Bredenoord AJ, Talley NJ, Whitehead WE. Aerophagia and rumination: recognition and therapy. Curr Treat Options Gastroenterol. 2006; 9:305–313.13. Lee TH. A case of rumination documented by using high-resolution impedance manometry. J Neurogastroenterol Motil. 2013; 19:259–260.14. Tack J, Blondeau K, Boecxstaens V, Rommel N. Review article: the pathophysiology, differential diagnosis and management of rumination syndrome. Aliment Pharmacol Ther. 2011; 33:782–788.15. Bredenoord AJ, Weusten BL, Timmer R, Akkermans LM, Smout AJ. Relationships between air swallowing, intragastric air, belching and gastro-oesophageal reflux. Neurogastroenterol Motil. 2005; 17:341–347.16. Bredenoord AJ, Weusten BL, Sifrim D, Timmer R, Smout AJ. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut. 2004; 53:1561–1565.17. Rommel N, Tack J, Arts J, Caenepeel P, Bisschops R, Sifrim D. Rumination or belching-regurgitation? Differential diagnosis using oesophageal impedance-manometry. Neurogastroenterol Motil. 2010; 22:e97–e104.18. Hemmink GJ, Weusten BL, Bredenoord AJ, Timmer R, Smout AJ. Aerophagia: excessive air swallowing demonstrated by esophageal impedance monitoring. Clin Gastroenterol Hepatol. 2009; 7:1127–1129.19. Bredenoord AJ. Excessive belching and aerophagia: two different disorders. Dis Esophagus. 2010; 23:347–352.20. Hemmink GJ, Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Supragastric belching in patients with reflux symptoms. Am J Gastroenterol. 2009; 104:1992–1997.21. Hemmink GJ, Weusten BL, Timmer R, Smout AJ. Increased swallowing frequency in GORD is likely to be caused by perception of reflux episodes. Neurogastroenterol Motil. 2009; 21:143–148.22. Tack J, Caenepeel P, Fischler B, Piessevaux H, Janssens J. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001; 121:526–535.23. Conchillo JM, Selimah M, Bredenoord AJ, Samsom M, Smout AJ. Air swallowing, belching, acid and non-acid reflux in patients with functional dyspepsia. Aliment Pharmacol Ther. 2007; 25:965–971.24. Zella SJ, Geenens DL, Horst JN. Repetitive eructation as a manifestation of obsessive-compulsive disorder. Psychosomatics. 1998; 39:299–301.25. Jones WR, Morgan JF. Eructophilia in bulimia nervosa: a clinical feature. Int J Eat Disord. 2012; 45:298–301.26. Chitkara DK, Van Tilburg M, Whitehead WE, Talley NJ. Teaching diaphragmatic breathing for rumination syndrome. Am J Gastroenterol. 2006; 101:2449–2452.27. Hemmink GJ, Ten Cate L, Bredenoord AJ, Timmer R, Weusten BL, Smout AJ. Speech therapy in patients with excessive supragastric belching--a pilot study. Neurogastroenterol Motil. 2010; 22:24–28. e2–e3.28. Blondeau K, Boecxstaens V, Rommel N, et al. Baclofen improves symptoms and reduces postprandial flow events in patients with rumination and supragastric belching. Clin Gastroenterol Hepatol. 2012; 10:379–384.29. Koek GH, Sifrim D, Lerut T, Janssens J, Tack J. Effect of the GABA(B) agonist baclofen in patients with symptoms and duodeno-gastro-oesophageal reflux refractory to proton pump inhibitors. Gut. 2003; 52:1397–1402.30. Lehmann A, Bremner-Danielsen M, Brändén L, Kärrberg L. Inhibitory effects of GABA(B) receptor agonists on swallowing in the dog. Eur J Pharmacol. 2002; 448:67–70.31. Spiegel SB. Uses of hypnosis in the treatment of uncontrollable belching: a case report. Am J Clin Hypn. 1996; 38:263–270.32. Cigrang JA, Hunter CM, Peterson AL. Behavioral treatment of chronic belching due to aerophagia in a normal adult. Behav Modif. 2006; 30:341–351.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- What Is the Difference in Characteristics Between Belching Disorder and Gastroesophageal Reflux Disease With Belching? Centering Around Supragastric Belching
- A Psychiatric Approach to a Patient with Excessive Belching
- Factors Associated with Belching and Retching during Esophagogastroduodenoscopy and Their Effects on Z-Line Appearance
- Belching (Eructation)
- Characteristics of Symptomatic Belching in Patients With Belching Disorder and Patients Who Exhibit Gastroesophageal Reflux Disease With Belching