J Korean Ophthalmol Soc.
2017 Dec;58(12):1425-1430. 10.3341/jkos.2017.58.12.1425.
A Case of Optic Nerve Head Swelling in a Patient with Primary Open-angle Glaucoma
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. pcheck@hanmail.net
- 2Therapeutics Center for Ocular Neovascular Disease, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2397859
- DOI: http://doi.org/10.3341/jkos.2017.58.12.1425
Abstract
- PURPOSE
To report a case of masked glaucomatous optic nerve head damage due to acute swelling in a primary open-angle glaucoma patient.
CASE SUMMARY
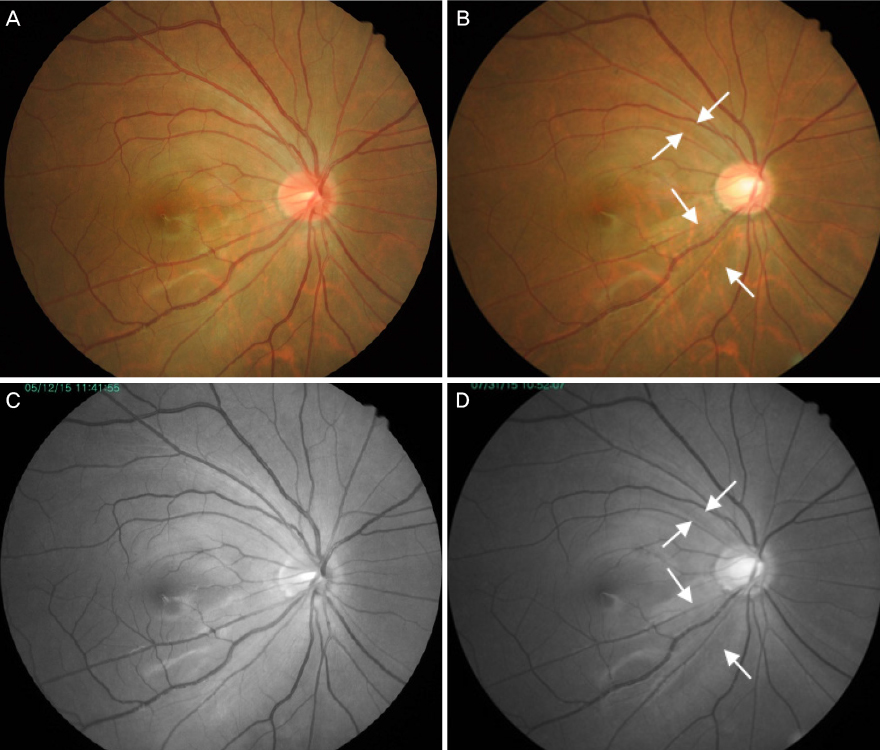
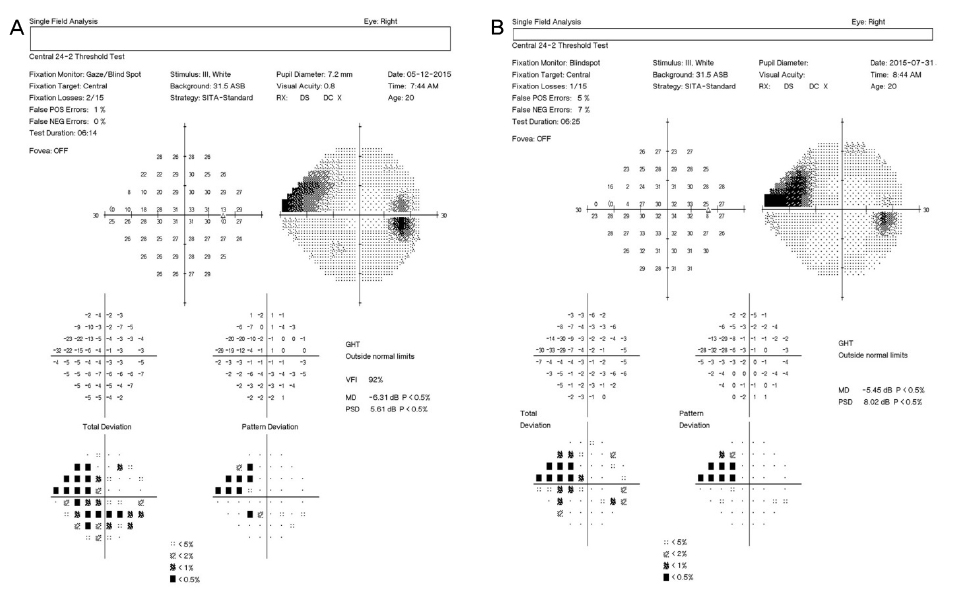
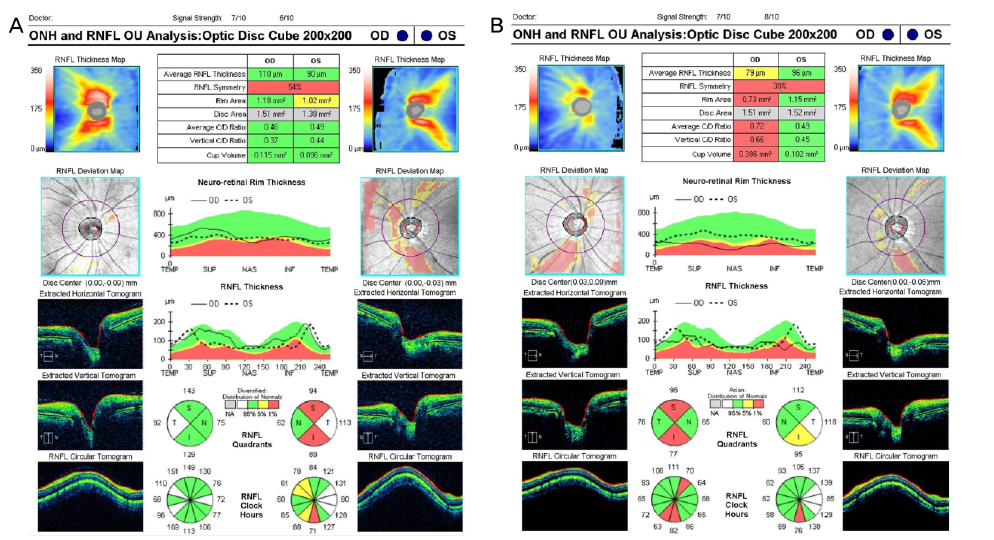
A healthy 21-year-old male visited our clinic complaining of blurred vision in the right eye for 1 week. The intraocular pressure (IOP) was 60 mmHg, as measured by a Goldmann applanation tonometer. No specific anterior segment finding other than severe corneal edema was found on slit lamp examination. Maximum tolerated medical therapy was performed, and a further examination was done 1 day after the IOP lowering. No glaucomatous change in the optic disc or retinal nerve fiber layer was observed on fundus examination and optical coherence tomography (OCT), but the optic disc of the right eye was more hyperemic than that of the left eye. A superonasal visual field defect was also observed using automated perimetry. After treatment, the IOP was kept within the normal range using IOP-lowering eye drops. However, an inferonasal retinal nerve fiber layer defect was observed on fundus examination and OCT, and a superonasal scotoma was detected by perimetry.
MeSH Terms
Figure
Reference
-
1. Anton A, Moreno-Montañes J, Blázquez F, et al. Usefulness of optical coherence tomography parameters of the optic disc and the retinal nerve fiber layer to differentiate glaucomatous, ocular hypertensive, and normal eyes. J Glaucoma. 2007; 16:1–8.2. Tsai JC, Lin PW, Teng MC, Lai IC. Longitudinal changes in retinal nerve fiber layer thickness after acute primary angle closure measured with optical coherence tomography. Invest Ophthalmol Vis Sci. 2007; 48:1659–1664.3. Liu X, Li M, Zhong YM, et al. Damage patterns of retinal nerve fiber layer in acute and chronic intraocular pressure elevation in primary angle closure glaucoma. Int J Ophthalmol. 2010; 3:152–157.4. Asrani S, Moore DB, Jaffe GJ. Paradoxical changes of retinal nerve fiber layer thickness in uveitic glaucoma. JAMA Ophthalmol. 2014; 132:877–880.5. Quigley HA, Guy J, Anderson DR. Blockade of rapid axonal transport. Effect of intraocular pressure elevation in primate optic nerve. Arch Ophthalmol. 1979; 97:525–531.6. Tso MO, Fine BS. Electron microscopic study of human papilledema. Am J Ophthalmol. 1976; 82:424–434.7. Fortune B, Yang H, Strouthidis NG, et al. The effect of acute intraocular pressure elevation on peripapillary retinal thickness, retinal nerve fiber layer thickness, and retardance. Invest Ophthalmol Vis Sci. 2009; 50:4719–4726.8. Yang H, Downs JC, Bellezza A, et al. 3-D histomorphometry of the normal and early glaucomatous monkey optic nerve head: prelaminar neural tissues and cupping. Invest Ophthalmol Vis Sci. 2007; 48:5068–5084.9. Anderson DR, Hendrickson A. Effect of intraocular pressure on rapid axoplasmic transport in monkey optic nerve. Invest Ophthalmol. 1974; 13:771–783.10. Quigley HA, Addicks EM. Chronic experimental glaucoma in primates. II. Effect of extended intraocular pressure elevation on optic nerve head and axonal transport. Invest Ophthalmol Vis Sci. 1980; 19:137–152.11. Minckler DS, Bunt AH, Klock IB. Radioautographic and cytochemical ultrastructural studies of axoplasmic transport in the monkey optic nerve head. Invest Ophthalmol Vis Sci. 1978; 17:33–50.12. Gupta V, Gupta S, Dhawan M, et al. Extent of asymmetry and unilaterality among juvenile onset primary open angle glaucoma patients. Clin Exp Ophthalmol. 2011; 39:633–638.13. Stanmper RL, Drake MV. Becker-Shaffer's Diagnosis and Therapy of the Glaucomas. 7th ed. St Louis: The CV Mosby Company;1999. p. 299.14. Aung T, Husain R, Gazzard G, et al. Changes in retinal nerve fiber layer thickness after acute primary angle closure. Ophthalmology. 2004; 111:1475–1479.15. Chew SS, Vasudevan S, Patel HY, et al. Acute primary angle closure attack does not cause an increased cup-to-disc ratio. Ophthalmology. 2011; 118:254–259.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Significance of Peripapillary Atrophy in the Diagnosis of Open-angle Glaucoma
- Regional Dirfferences in The Stereometric Parameters of Optic Nerve Head in Primary Open Angle Glaucoma
- Optic Nerve Head Appearance in Chronic Primary Angle-Closure Glaucoma and Primary Open-Angle Glaucoma
- Peripapillary Atrophy in Primary Open-Angle Glaucoma and Normal-Tension Glaucoma
- Clinical Evaluation of Unilateral Open-Angle Glaucoma: A Two-Year Follow-Up Study