Ann Surg Treat Res.
2017 Dec;93(6):331-335. 10.4174/astr.2017.93.6.331.
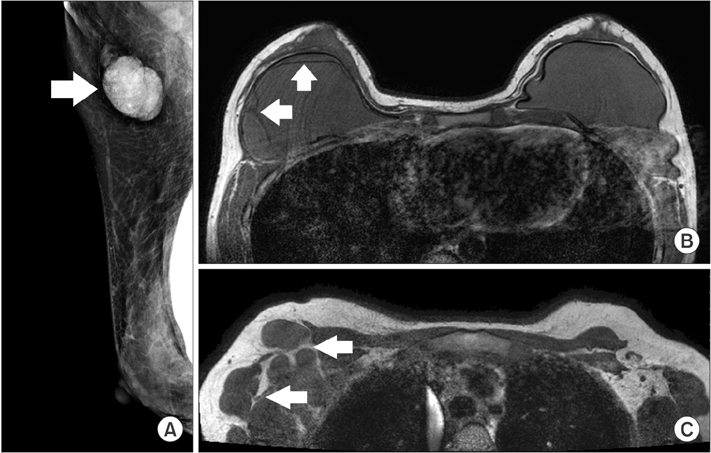
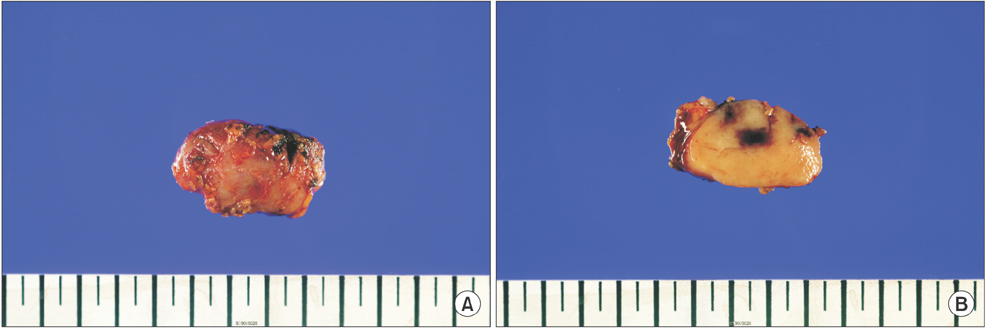
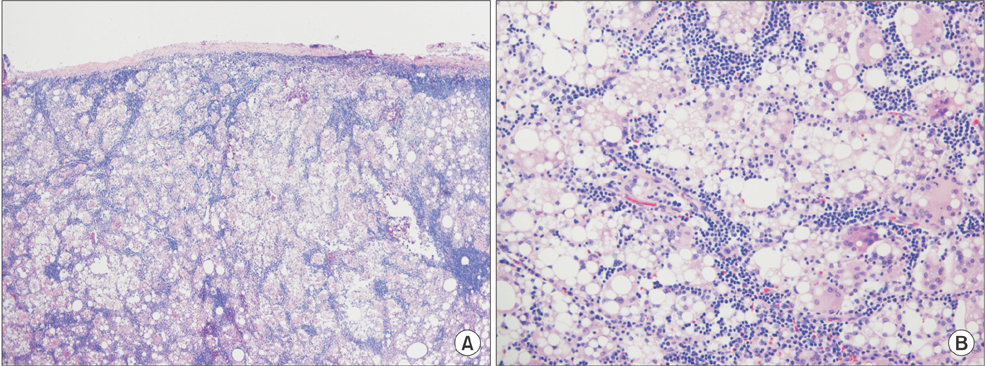
Extensive silicone lymphadenopathy after breast implant insertion mimicking malignant lymphadenopathy
- Affiliations
-
- 1Department of Pathology, Korea University Hospital, Korea University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Korea University Hospital, Korea University College of Medicine, Seoul, Korea.
- 3Department of Plastic Surgery and Reconstructive Surgery, Korea University Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Division of Breast and Endocrine Surgery, Department of Surgery, Korea University Hospital, Korea University College of Medicine, Seoul, Korea. jungspil@korea.ac.kr
- KMID: 2396875
- DOI: http://doi.org/10.4174/astr.2017.93.6.331
Abstract
- Silicone implants are widely used in aesthetic and reconstructive breast surgery. Silicone lymphadenopathy is a well-known rare complication of implant insertion. Silicone leakage from a rupture or silicone bleeding can accumulate in lymph nodes. Foreign body reactions in the affected lymph nodes may be misdiagnosed as metastasis or malignant lymphadeno pathy upon initial presentation if silicone lymphadenopathy is not considered in the initial diagnosis. We report a case of siliconoma with extensive involvement of multiple lymph nodes mimicking malignant features to emphasize that clinicians should carefully evaluate each patient's medical history and disease status during differential diagnosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Gidengil CA, Predmore Z, Mattke S, van Busum K, Kim B. Breast implant-associated anaplastic large cell lymphoma: a systematic review. Plast Reconstr Surg. 2015; 135:713–720.2. Cook PD, Osborne BM, Connor RL, Strauss JF. Follicular lymphoma adja cent to foreign body granulomatous inflammation and fibrosis surrounding silicone breast prosthesis. Am J Surg Pathol. 1995; 19:712–717.3. Gundeslioglu AO, Hakverdi S, Erdem O, Ozen EC, Inan I, Emlik D. Axillary lipogranuloma mimicking carcinoma metastasis after silicone breast implant rupture: a case report. J Plast Reconstr Aesthet Surg. 2013; 66:e72–e75.4. Maxwell GP, Gabriel A. The evolution of breast implants. Clin Plast Surg. 2015; 36:399–404.5. McLaughlin JK, Lipworth L, Murphy DK, Walker PS. The safety of silicone gelfilled breast implants: a review of the epidemiologic evidence. Ann Plast Surg. 2007; 59:569–580.6. de Jong D, Vasmel WL, de Boer JP, Verhave G, Barbe E, Casparie MK, et al. Anaplastic largecell lymphoma in women with breast implants. JAMA. 2008; 300:2030–2035.7. Holmich LR, Friis S, Fryzek JP, Vejborg IM, Conrad C, Sletting S, et al. Incidence of silicone breast implant rupture. Arch Surg. 2003; 138:801–806.8. Allergan Silicone Breast Implant U.S. Core Clinical Study Group. Spear SL, Murphy DK. Natrelle round silicone breast implants: Core Study results at 10 years. Plast Reconstr Surg. 2014; 133:1354–1361.9. Zambacos GJ, Molnar C, Mandrekas AD. Silicone lymphadenopathy after breast augmentation: case reports, review of the literature, and current thoughts. Aesthetic Plast Surg. 2013; 37:278–289.10. Buley ID. Fine needle aspiration of lymph nodes. J Clin Pathol. 1998; 51:881–885.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Axillary silicone lymphadenopathy caused by gel bleeding with intact silicone breast implants: a case report
- The Clinical Implications of Poly Implant Prothese Breast Implants: An Overview
- Silicone Granuloma Mimicking a Lymphatic Metastasis in a Lung Cancer Patient: A Case Report
- Understanding Silicone Breast Implant-Associated Complications for Radiologists
- Toxocariasis Mimicking Lymphoma and Presenting as Multiple Lymphadenopathy: A Case Report