Korean J Ophthalmol.
2017 Dec;31(6):533-537. 10.3341/kjo.2017.0044.
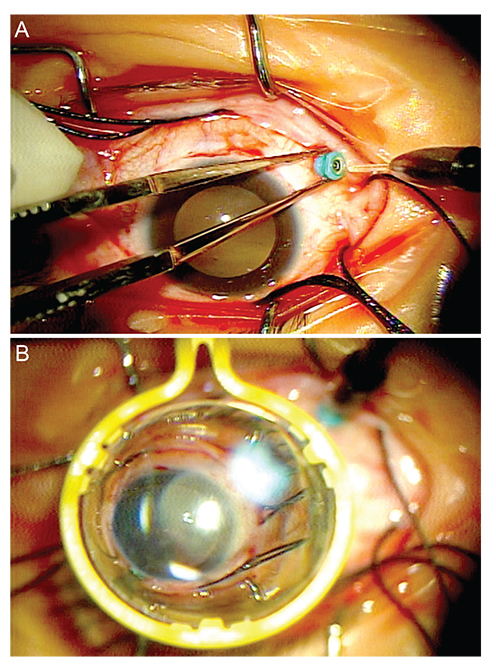
Scleral Buckling Using a Non-contact Wide-Angle Viewing System with a 25-Gauge Chandelier Endoilluminator
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. ophthalmo@amc.seoul.kr
- KMID: 2396704
- DOI: http://doi.org/10.3341/kjo.2017.0044
Abstract
- PURPOSE
To report the outcome of scleral buckling using a non-contact wide-angle viewing system with a 25-gauge chandelier endoilluminator.
METHODS
Retrospective analyses of medical records were performed for 17 eyes of 16 patients with primary rhegmatogenous retinal detachment (RRD) without proliferative vitreoretinopathy who had undergone conventional scleral buckling with cryoretinopexy using the combination of a non-contact wide-angle viewing system and chandelier endoillumination.
RESULTS
The patients were eight males and five females with a mean age of 26.8 ± 10.2 (range, 11 to 47) years. The mean follow-up period was 7.3 ± 3.1 months. Baseline best-corrected visual acuity was 0.23 ± 0.28 logarithm of the minimum angle of resolution units. Best-corrected visual acuity at the final visit showed improvement (0.20 ± 0.25 logarithm of the minimum angle of resolution units), but the improvement was not statistically significant (p = 0.722). As a surgery-related complication, there was vitreous loss at the end of surgery in one eye. As a postoperative complication, increased intraocular pressure (four cases) and herpes simplex epithelial keratitis (one case) were controlled postoperatively with eye drops. One case of persistent RRD after primary surgery needed additional vitrectomy, and the retina was postoperatively attached.
CONCLUSIONS
Scleral buckling with chandelier illumination as a surgical technique for RRD has the advantages of relieving the surgeon's neck pain from prolonged use of the indirect ophthalmoscope and sharing the surgical procedure with another surgical team member. In addition, fine retinal breaks that are hard to identify using an indirect ophthalmoscope can be easily found under the microscope by direct endoillumination.
MeSH Terms
-
Female
Follow-Up Studies
Herpes Simplex
Humans
Intraocular Pressure
Keratitis
Lighting
Male
Medical Records
Neck Pain
Ophthalmic Solutions
Ophthalmoscopes
Postoperative Complications
Retina
Retinal Detachment
Retinal Perforations
Retrospective Studies
Scleral Buckling*
Visual Acuity
Vitrectomy
Vitreoretinopathy, Proliferative
Ophthalmic Solutions
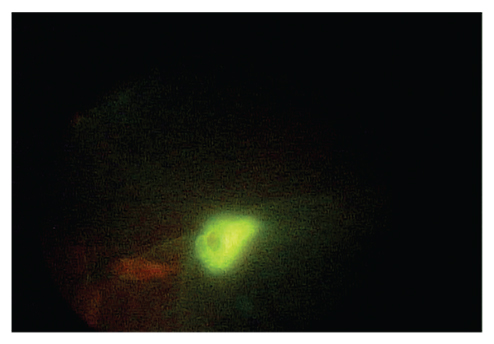
Figure
Reference
-
1. D'Amico DJ. Clinical practice: primary retinal detachment. N Engl J Med. 2008; 359:2346–2354.2. Narayanan R, Tyagi M, Hussein A, et al. Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina. 2016; 36:830–833.3. Adelman RA, Parnes AJ, Ducournau D. European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of uncomplicated retinal detachments: the European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013; 120:1804–1808.4. Ohji M, Tano Y. Vitreoretinal surgery with slit-lamp illumination combined with a wide-angle-viewing contact lens. Am J Ophthalmol. 2004; 137:955–956.5. Aras C, Ucar D, Koytak A, Yetik H. Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica. 2012; 227:107–110.6. Nam KY, Kim WJ, Jo YJ, Kim JY. Scleral buckling technique using a 25-gauge chandelier endoilluminator. Retina. 2013; 33:880–882.7. Kita M, Fujii Y, Kawagoe N, Hama S. Scleral buckling with a noncontact wide-angle viewing system in the management of retinal detachment with undetected retinal break: a case report. Clin Ophthalmol. 2013; 7:587–589.8. Imai H, Tagami M, Azumi A. Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol. 2015; 9:2103–2107.9. Nagpal M, Bhardwaj S, Mehrotra N. Scleral buckling for rhegmatogenous retinal detachment using vitrectomy-based visualization systems and chandelier illumination. Asia Pac J Ophthalmol (Phila). 2013; 2:165–168.10. Mehta S, Hubbard GB 3rd. Avoiding neck strain in vitreoretinal surgery: an ergonomic approach to indirect ophthalmoscopy and laser photocoagulation. Retina. 2013; 33:439–441.11. Shaw C, Bourkiza R, Wickham L, et al. Mechanical exposure of ophthalmic surgeons: a quantitative ergonomic evaluation of indirect ophthalmoscopy and slit-lamp biomicroscopy. Can J Ophthalmol. 2017; 52:302–307.12. Yokoyama T, Kanbayashi K, Yamaguchi T. Scleral buckling procedure with chandelier illumination for pediatric rhegmatogenous retinal detachment. Clin Ophthalmol. 2015; 9:169–173.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Scleral Buckling under a Slit-lamp Illumination System with a Contact Wide-angle Viewing Lens Compared with an Indirect Ophthalmoscope
- 2 Cases of Combined Cataract and Scleral Buckling Surgery
- Enhanced Peripheral Retinal Illumination by Curved Endoilluminator During Phakic Vitrectomy
- Comparative Analysis of Scleral Buckling With or Without Postoperative Photocoagulation
- Scleral perforation after scleral buckling surgery for retinopathy of prematurity